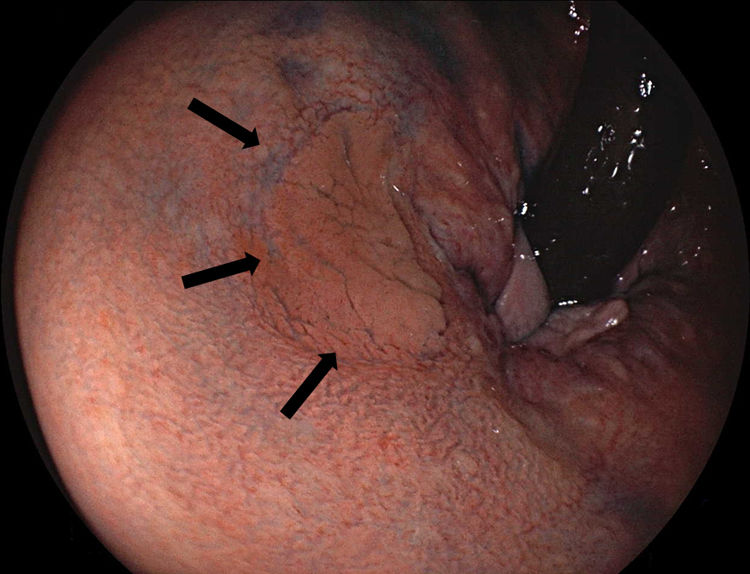
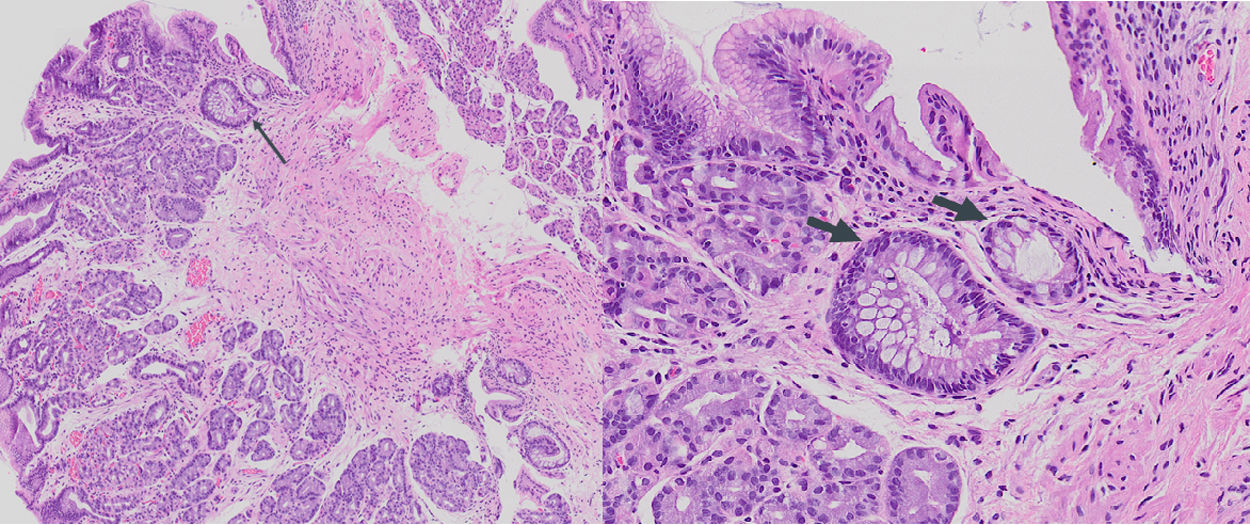
A 44-year-old male was referred for colonoscopy due to family history of colorectal cancer. Colonoscopy revealed a laterally spreading, non-granular flat type lesion (Paris classification 0-IIa), measuring 12mm, localized in the rectum at 3cm from the anal verge (Fig. 1), which was removed en bloc by endoscopic mucosal resection (EMR). Histologic evaluation showed fragments of fundic gastric mucosa along with unaltered colonic mucosa (Fig. 2).
Gastric heterotopia (GHT) has been reported in various locations along the gastrointestinal tract. GHT in the colon is very rare, and most cases are located in the rectum.1 Clinical presentation is variable, ranging from asymptomatic to the most common symptom of painless rectal bleeding. Endoscopically, rectal GHT may present as diverticula, ulcer, polyp or flat/depressed lesion mimicking early cancer. Histopathological examination is the gold standard for diagnosis. Fundic-type mucosa is the most common histologic subtype described.2 Helicobacter pylori may colonize gastric mucosa regardless of its location. GHT has an associated risk of malignant transformation, as the first case of colonic adenocarcinoma arising from GHT has already been described.3 Endoscopic removal either by EMR or endoscopic submucosal dissection (ESD) or, alternatively, surgical excision, are considered the treatment of choice.