Portal hypertensive colopathy (PHC) is the colonic manifestation of portal hypertension. It refers to mucosal changes distributed along the colon: mucosal edema, erythema, granularity, friability, and vascular lesions such as angiodysplasia1.
We report the case of a 77-year-old man with a long-course history of cirrhosis to alcohol and hepatitis C virus, Child–Pugh B (8 points), with a previous episode of esophageal variceal bleeding, diabetes mellitus type 2, and iron-deficiency anemia, medicated with propranolol 30mg/day, furosemide 40mg/day, metformin plus sitagliptin and oral iron who was referred to our Emergency Department for hematochezia.
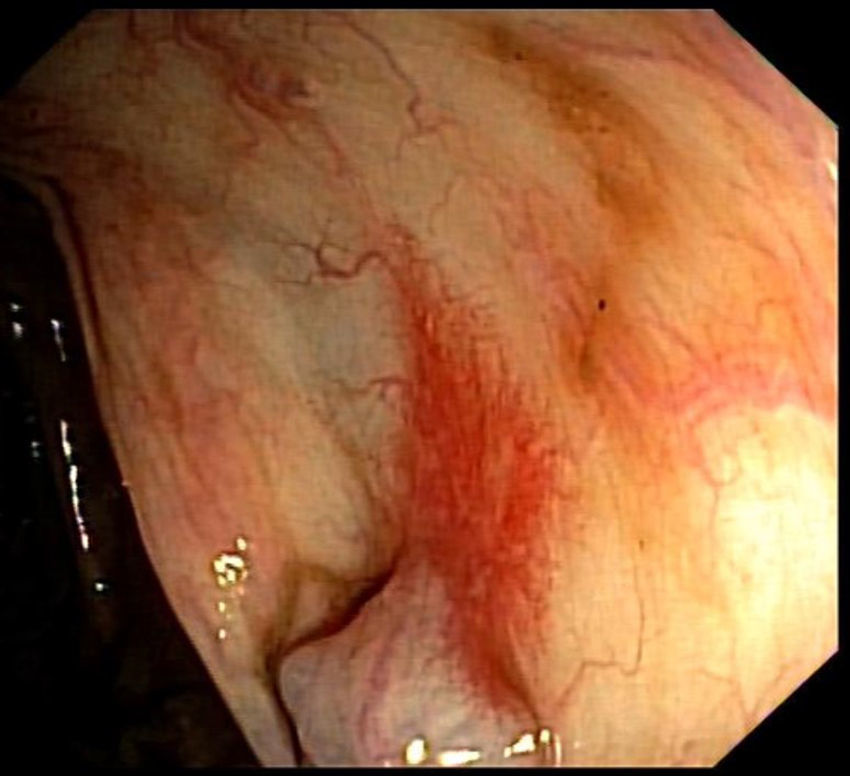
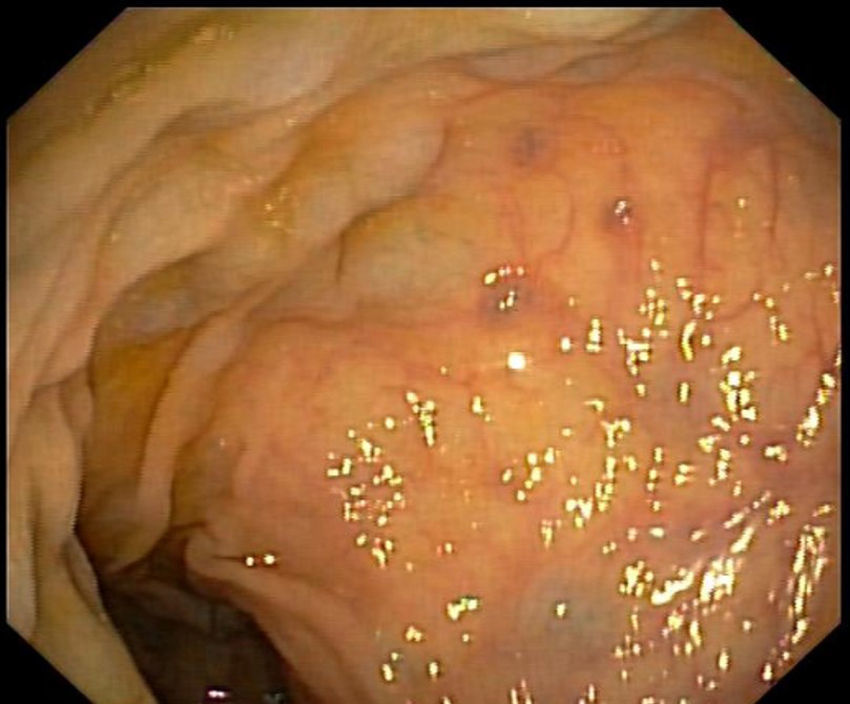
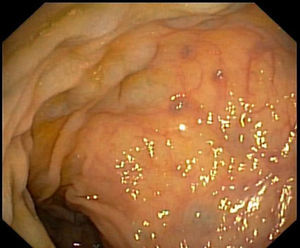
For the investigation of the iron-deficiency anemia an endoscopic study had been conducted two months before, which included: an esophagogastroduodenoscopy (EGD), where small esophageal varices and mucosal changes compatible with mild portal hypertensive gastropathy were found; and a colonoscopy, where the colonic mucosa was diffusely altered by the presence of edema, erythema, angiectasia (Fig. 1) and varices (Fig. 2) and a diagnosis of PHC was established.
On admission the patient was conscious and hemodynamically stable and the blood analysis demonstrated an acute anemia with a hemoglobin of 8.3g/dL, platelets of 75,000/μL and an INR of 1.3. A colonoscopy was performed which showed hematochezia from the rectum to the transverse colon and the already known mucosal changes. It was assumed that the CPH was the cause of the lower gastrointestinal bleeding (LGIB). The patient was started on octreotide perfusion for 5 days, along with antibiotic prophylaxis with ceftriaxone. Two days later he showed another episode of LGIB, but this time with hemodynamic instability and a profound drop on hemoglobin to a minimum of 6.2g/dL. To exclude an upper source of the hemorrhage he was submitted to an EGD, which was superimposable to the other one, with no blood. Thereafter the patient had an uneventful stay at the hospital and he was discharged with a hemoglobin of 9.3g/dL. As he was already under beta-blocker therapy (propranolol), the only medical therapeutic approach left was long-acting octreotide, which was initiated at a dose of 10mg per month, by intramuscular route.
On 9 month follow-up he maintains his hemoglobin level at 9–10g/dL, at the expense of iron-replacement therapy, although he had no need for red blood cell transfusions, showed no more bleeding episodes, and no adverse events with the therapy were recorded; these facts highlight both long-acting octreotide's effectiveness and safety.
PHC was described for the first time in 19912 and since then no more than 50 case series or reports are published in Pubmed database on this subject.
The prevalence of PHC in cirrhotic patients, reported in the four most recent series (that comprises the last seven years), varies from 23.9 to 71%.1,3–5 Although its relatively high prevalence it rarely produces symptoms, especially bleeding, which is estimated to occur in no more than 9% of patients.1 There are conflicting results about the correlation between PHC's prevalence and severity and cirrhosis’ or portal hypertension's severity,1 so currently there are no consensual predictive factors for its presence.
The diagnosis is made endoscopically although there is not a universal classification system and, until now, three different systems – even if very similar – have been proposed.6–8 All of them include vascular ectasia.
The pathogenesis is not also fully understood but it is essentially based on colonic mucosal capillary ectasia.1
Therapeutic strategies are not unanimous as evidence is limited, due, essentially, to the rarity of symptomatic patients. For chronic LGIB beta-blockers are said to be effective.6,9 For acute LGIB vasoactive medications such as octreotide may be a good option. The use of octreotide in PHC has been reported in a single case report; in this case the authors used only the perfusion and not the long-acting formulation, which may explain their poorer results.9 These medications have also been tried in animal models with positive effects.1
The use of laser photocoagulation therapy may be less effective as CPH are normally numerous and diffuse. In the context of rescue therapy other options have been used in unique cases: TIPS, sclerotherapy and even colectomy.1
This case report highlights the use of a rather unknown therapeutic option (long-acting octreotide) for a relatively rare condition – lower gastrointestinal bleeding in the context of PHC – which may contribute to our knowledge about this entity, which is also not fully understood.