Inflammatory bowel disease may cause both intestinal and extraintestinal manifestations. Respiratory symptoms in ulcerative colitis are rare and tracheal involvement is exceedingly rare in children.
Case 1Sixteen year-old female with a 4-week-complaint of abdominal pain, bloody diarrhea, fever and cough. The investigation was consistent with the diagnosis of concomitant ulcerative colitis/coinfection to Escherichia coli. On day 4 respiratory signs persisted so azithromycin and inhaled corticosteroids were added. By day 6 she progressed to respiratory failure and was diagnosed with necrotic tracheitis so started on intravenous steroids with fast clinical improvement.
Case 2Twelve-year-old male adolescent with ulcerative colitis and sclerosing cholangitis started dry cough and throat pain 10 days after diagnosis. Laboratory investigations showed increased inflammatory signs and normal chest X-ray. He started treatment with azithromycin without clinical improvement and on day five he presented dyspnea and fever. Laryngeal fibroscopy suggested tracheitis and so systemic steroids where added with fast clinical and analytic improvement.
DiscussionTracheitis should be suspected if there are persistent respiratory symptoms even when exams are normal. Early recognition and early treatment are essential for a good prognosis preventing progression to respiratory failure.
A doença inflamatória intestinal pode ser causa de complicações intestinais e extraintestinais. As manifestações respiratórias de colite ulcerosa são raras e o envolvimento traqueal é extremamente raro em crianças.
Caso 1Adolescente do sexo feminino, de dezasseis anos de idade, com queixas de dor abdominal, diarreia sanguinolenta, febre e tosse seca com 4 semanas de evolução. A investigação realizada foi compatível com o diagnóstico de colite ulcerosa/co-infecção a Escherichia coli. No 4ª dia de internamento, por persistência das queixas respiratórias, iniciou azitromicina e corticoterapia inalada. Dois dias mais tarde evoluiu para insuficiência respiratória; foi-lhe diagnosticada traqueíte necrotizante pelo que iniciou corticóides endovenosos com rápida melhora clínica.
Caso 2Adolescente do sexo masculino de 12 anos de idade com colite ulcerosa e colangite esclerosante que inicia queixas de odinofagia e tosse seca 10 dias após o diagnóstico. O estudo analítico revelou aumento dos parâmetros inflamatórios e radiografia de tórax normal. Nesta altura inicia azitromicina, sem melhora clínica, iniciando, no quinto dia de doença, dispnéia e febre. A fibroscopia laríngea foi sugestiva de traqueíte pelo que iniciou corticoterapia sistémica com rápida melhoria clínica e analítica.
DiscussãoA traqueíte é uma entidade que deve ser equacionada em doentes com doença inflamatória intestinal na presença de sintomas respiratórios persistentes, mesmo com estudo complementar normal. O seu reconhecimento e tratamento precoces são essenciais para um prognóstico favorável e prevenção da progressão para insuficiência respiratória.
Inflammatory bowel disease (IBD) has long been recognized to cause both intestinal and extra-intestinal complications. Airway involvement in IBD can affect any part of the respiratory system but the exact incidence and prevalence of this manifestation are not known.1–4 Sporadic reports of tracheal involvement in ulcerative colitis are exceedingly rare, and are reported in 16 previous adult cases.5–14 The aim of this paper is to document the occurrence of this rare situation in children and stress the importance of an early diagnosis and treatment of a potential life threatening condition.
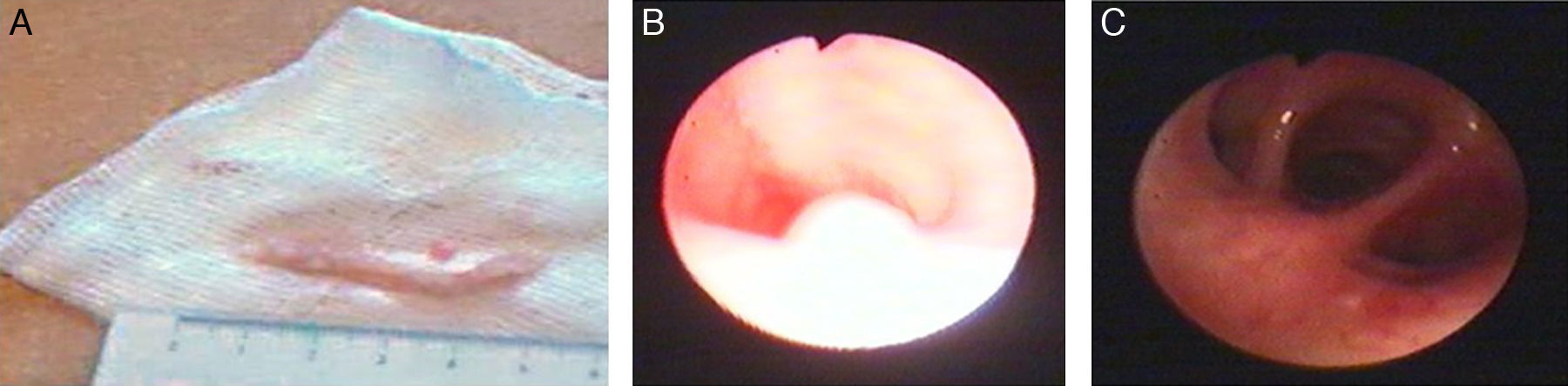
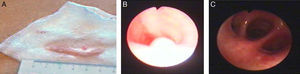
2Clinical cases2.1Case 1A previously healthy 16-year-old female presented with abdominal pain, bloody diarrhea, fever and productive cough for 4 weeks. Physical evaluation showed a normal lung exam and diffuse abdominal pain without tenderness or other peritoneal signs. Laboratory investigations revealed normocytic anemia (hemoglobin 9.5g/dL, reference value 12–16g/dL), thrombocytosis (platelets 425,000/μL, reference value 150,000–300,000/μL), increased C reactive protein (CRP) 203mg/L (reference value <3mg/L) and negative pANCA; Escherichia coli O157 H7 positive stool culture and normal abdominal X-ray. Suspecting infectious colitis she started intravenous metronidazole and ciprofloxacin with no clinical improvement of diarrhea after a week. Subsequent endoscopic investigation and histology were consistent with the diagnosis of ulcerative colitis. During this period she maintained persistent productive cough sometimes spasmodic. Presumptive diagnosis of ulcerative colitis with concomitant infective colitis and respiratory infection was done and she started treatment with messalazin, azithromycin and inhaled corticosteroid. Bacteriology, virology, polymerase chain reaction (PCR) for Bordetella pertussis in sputum and serological tests for Mycoplasma pneumoniae were negative. By day six she progressed to respiratory failure needing endotracheal intubation and mechanical ventilation. Abundant tracheal secretions were seen and cytological evaluation showed necrotic inflammatory exudate suggesting necrotic inflammatory process. Bronchoscopy disclosed mucous ulceration and white plaques along trachea; inflammatory exudate with necrosis debris and squamous metaplasia was observed in mucosal biopsies. At this time necrotic tracheitis was diagnosed and intravenous steroids were started with fast clinical improvement. No microorganisms were identified in bronchoscopy aspirates. One week later, fibroscopy showed significant improvement with persistence of some mucosal irregularities and one polypoid tracheal lesion (Fig. 1). Bronchoscopy performed seven weeks after the admission was normal and ileocolonoscopy at the same time showed pseudopolyps formation in mucosal areas of transverse and descending colon; biopsies revealed normal ileum and the colic mucosa displayed focal crypt architectural distortion; mild lymphoplasmacytic inflammation in the descending and sigmoid mucosae, and occasional crypt abscesses. Pulmonary functional studies were normal two months after the event. Six years later she has been in remission of IBD without any respiratory symptoms.
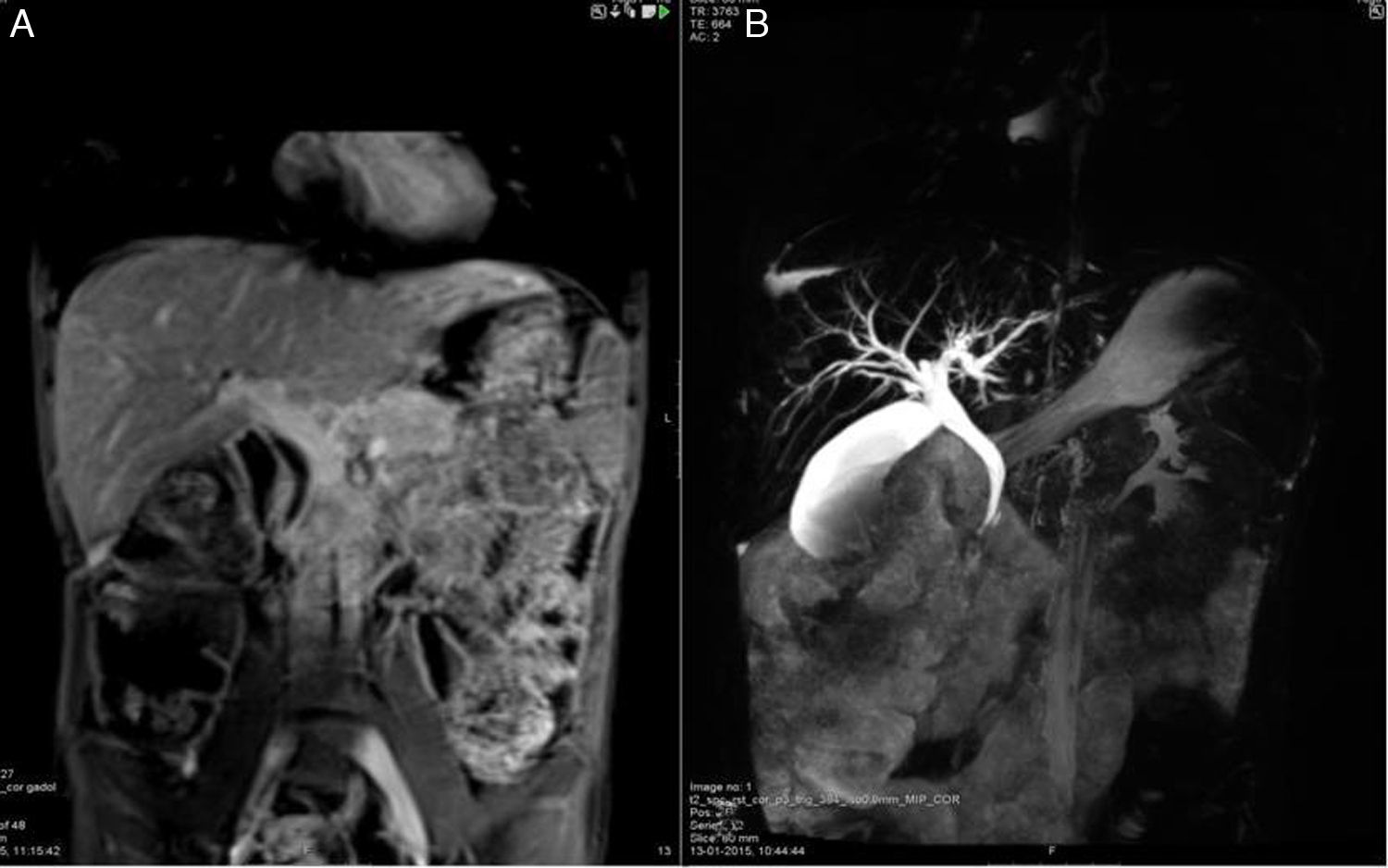
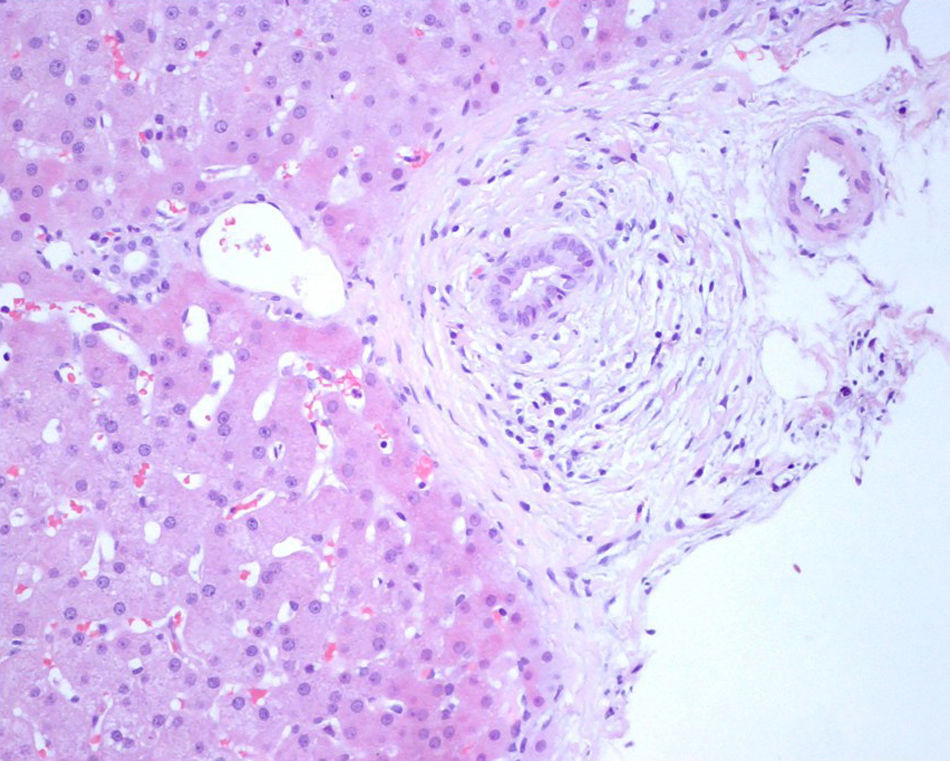
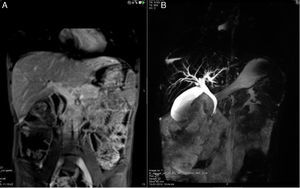
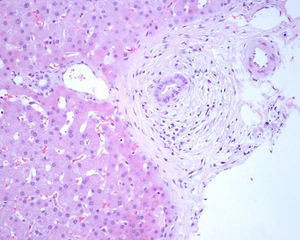
2.2Case 2A 12-year-old male adolescent diagnosed ulcerative colitis and sclerosing cholangitis under oral messalazin and ursodeoxycholic acid treatment. Clinical picture at diagnosis included recurrent episodes of jaundice, pruritus, diarrhea and vomiting for the last four months; laboratory data showed elevated aminotransferases, y-glutamyl transpeptidase and conjugated bilirubin; ANCA serology was negative with no other analytic changes. Colonoscopy and histology were consistent with the diagnosis of ulcerative colitis. Cholangio magnetic resonance imaging (MRI) disclosed increased diameter of the common bile duct (12mm) and irregular intrahepatic ducts with biliary ectasia and some segmental stenosis suggestive of sclerosing cholangitis (Fig. 2). Liver biopsy revealed, in several portal tracts, cholangitis with concentric periductal fibrosis and mild mixed inflammatory infiltrate around bile ducts or infiltrating its epithelial lining (Fig. 3).
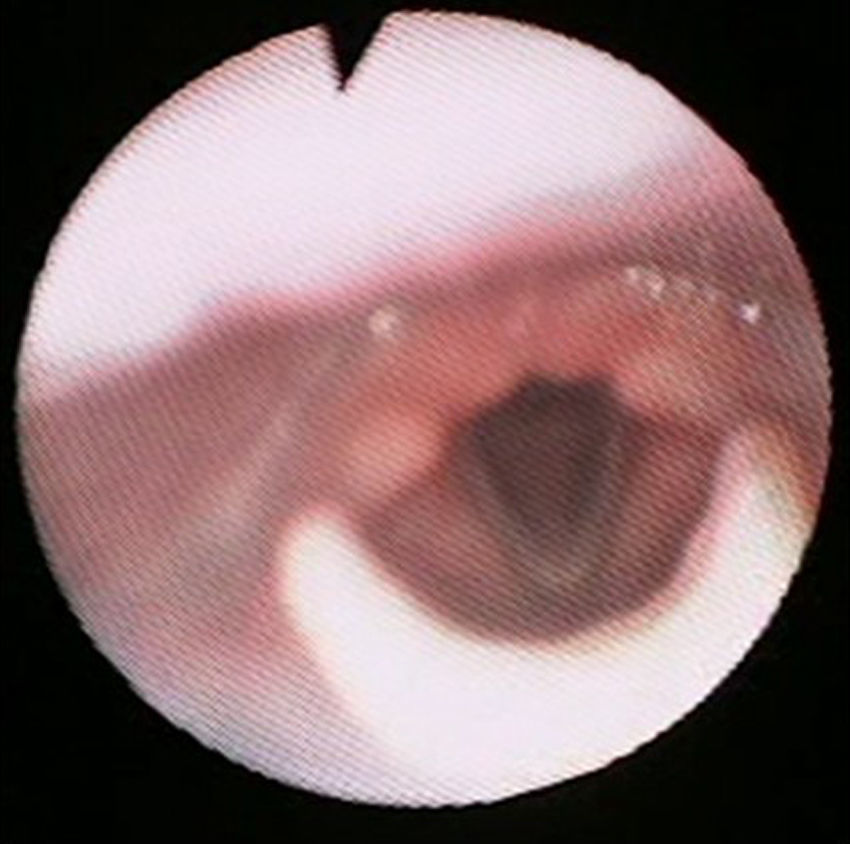
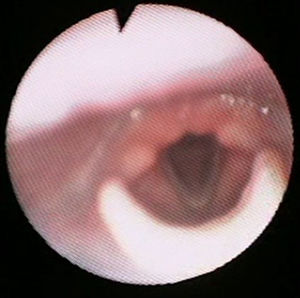
Ten days after the initial diagnose he came back to emergency room with dry cough and throat pain. Laboratory results showed elevated CRP (211mg/L), erythrocyte sedimentation rate (62mm/1st h, reference value 4–20mm/1st h) with no leukocytosis. He started treatment with azithromycin for 4 days without clinical improvement. Fever and shortness of breath started by day five. On physical exam the boy was pale with respiratory distress signs, and respiratory crackles. Chest X-ray was normal and analytics showed leukocytosis 34,500/μL (reference value 4500–13,000/μL) and worsening of inflammatory parameters (CRP 292mg/L, ESR 111mm). The severity of throat complaints led to laryngeal fibroscopy: subglottic and tracheal erythema were seen as well as edema and plaques suggesting tracheitis. At this time he was started on intravenous steroids and inhaled epinephrine with fast clinical improvement. Blood and respiratory cultures were both negative and by day four serial laboratory evaluation showed decreased inflammatory signs (leukocytes 22,500/μL and CRP 31mg/L). Fibroscopy on day 7 was normal (Fig. 4). Nine months later he was on remission and maintains follow-up without any respiratory symptoms.
3DiscussionThe causes and mechanisms of respiratory tract involvement in ulcerative colitis and Crohn's disease remain poorly understood. Some authors speculate that many of the extraintestinal manifestations of IBD, including respiratory disease, are secondary to circulating inflammatory mediators released by the inflamed bowel mucosa. These inflammatory mediators may remain in the respiratory system for a long time, causing smoldering injuries. Other authors propose that although the trigger of the immune response may be essentially the same in the respiratory tract and the large intestine, amplification of the inflammatory process might be different, resulting in unparalleled clinical courses in those organs.15–19
Upper airway disease may involve pharynx, trachea and main stem bronchi. According to the published cases it rarely precedes the diagnosis of ulcerative colitis, do not correlate with the activity of colonic disease and may even present several years after inactive colic disease or after colectomy. Tracheitis may present with gradually increasing cough (dry or productive), dyspnea on exertion, wheezing or stridor. Investigations may be normal or reveal slight leukocytosis with elevated neutrophil count and increased erythrocyte sedimentation rate and C reactive protein. Chest X-ray is usually normal. Bronchoscopy can show diffuse inflammation of the trachea and bronchi with widely scattered whitish lesions if the large airway is involved and narrowing of the lumen, while biopsy often reveals a granulation tissue, inflammatory infiltration. Differential diagnosis of infectious causes of tracheitis should be considered. In our cases the respiratory manifestations were simultaneous to the diagnosis of ulcerative colitis and presented in a very young age in contrast to the majority of the cases related in the literature (mean age 45 years).5–14 The clinical presentation, bronchoscopic and histological finds were very similar to that described in adult population.
Because of the paucity of reported cases of laryngotracheal involvement and IBD, no generally consensual or evidence-based treatment regimen exists. Most adult patients responded rapidly to a regimen of oral or intravenous corticosteroids. Other reported treatment modalities have included inhaled corticosteroids and epinephrine. In refractory cases procedures like laser beam, balloon dilatation, stent placement or tracheotomy may be necessary to maintain patent airway.10–13,20–24 According to our experience, in the first case the girl had evolution to respiratory failure in spite of inhaled corticosteroid therapy. This highlights the fact that inhaled administration may not be efficient enough in severe cases. In both our patients intravenous corticosteroids were very successful in treating this condition with rapid clinical improvement. The experience of the first case allowed a high index of suspicion when the second patient worsened respiratory symptoms and led to an earlier and effective therapeutic intervention. The knowledge of this entity can contribute to avoid unnecessary combination of antibiotics and delayed correct treatment especially in pediatric population in whom infection picture is very common. Suspicion index can be very useful when empiric antibiotic treatment has not been successful in progressive respiratory complaints picture.
Early identification and therapy of related respiratory manifestations of IBD are important to improve short and long-term outcome; if left untreated this condition may progress to irreversible airway fibrosis.12,17,25
In conclusion, when children with inflammatory bowel disease have persistent respiratory symptoms (as cough, dyspnea, hoarseness and/or respiratory distress) it is important to consider the possibility of tracheitis, as in adults. Awareness and early recognition and treatment are essential for a good prognosis preventing progression to respiratory failure.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
AuthorshipAll authors have actively contributed to the article and the International Committee of Medical Journal Editors (ICMJE) requirements for authorship have been met.