While HTN is widely seen as a primary threat to cardiovascular conditions worldwide, it is essential to recognize that not all HTN is identical.
ObjectiveTo determine the prevalence, trend, and factors associated with each type of HTN: isolated systolic (ISH), isolated diastolic (IDH), and systolic–diastolic (SDH).
MethodsA secondary analysis of data from the Demographic and Family Health Survey from 2014 to 2022 was conducted. For the analysis of associated factors, a Poisson regression model with robust variance was implemented to calculate adjusted prevalence ratios (aPR) along with their 95% confidence intervals.
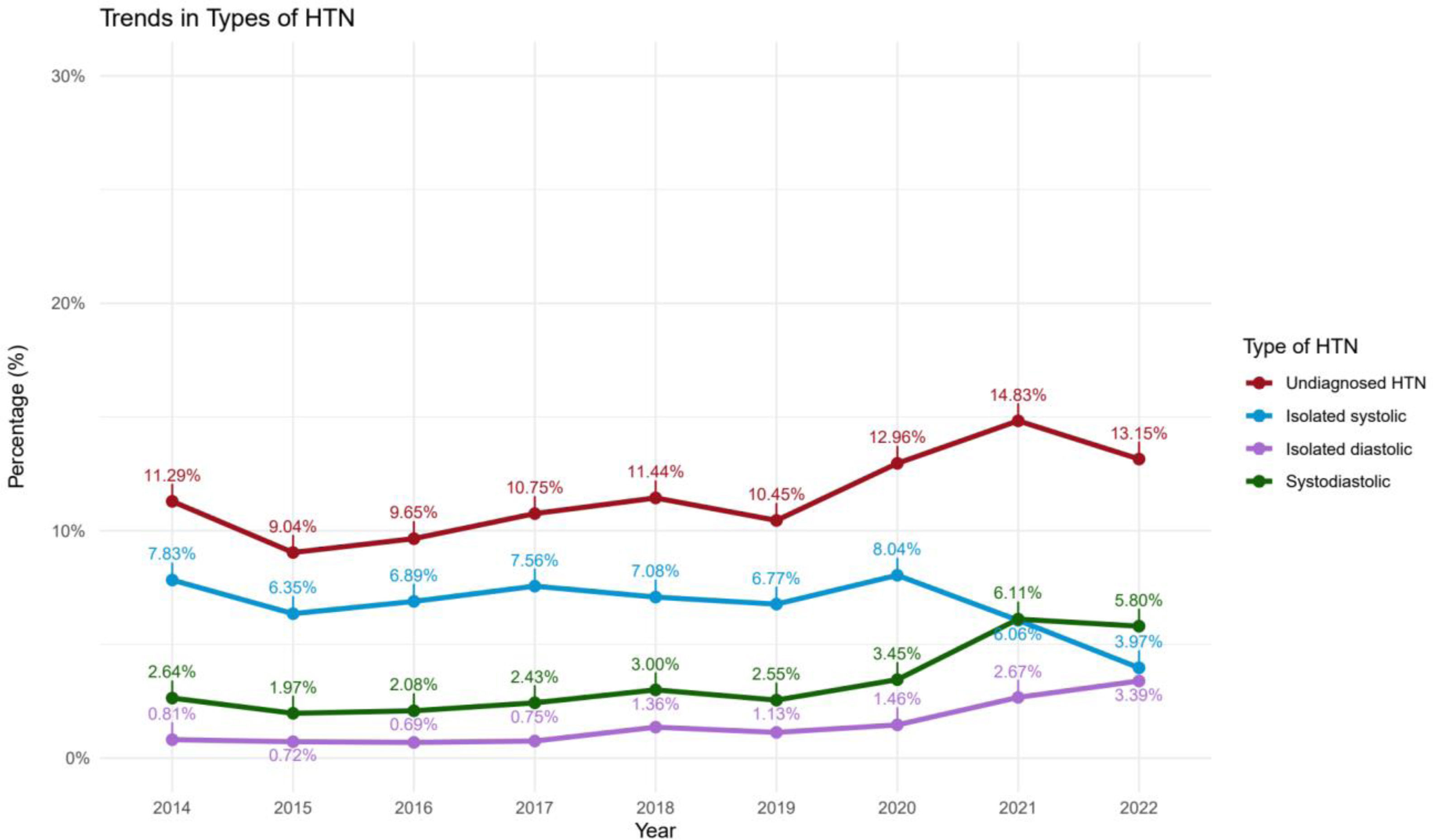
ResultsThe prevalence was 7.02%, 1.55%, and 3.28% for ISH, IDH, and SDH, respectively. ISH showed a decline in 2022, unlike the other two types, which seem to be on the rise. A statistically significant association was found in men and an increased risk with age for ISH and SDH, unlike IDH, where age acts as a protective factor. Additional factors identified include smoking and excessive alcohol consumption, while a high intake of fruits/vegetables offers a protective effect. Obesity and diabetes were associated with a higher risk, and significant variations by region and altitude, as well as among ethnic groups, were observed.
ConclusionsSignificant differences in the prevalence of HTN subtypes have been found, underscoring the heterogeneity of this chronic condition, both in related factors and in trends over the years.
Si bien la hipertensión arterial (HTA) es reconocida globalmente como un importante factor de riesgo para enfermedades cardiovasculares, es crucial entender que no todos los tipos de HTA son iguales.
ObjetivoDeterminar la prevalencia, tendencia y los factores asociados a cada tipo de HTA: sistólica aislada (ISH), diastólica aislada (IDH) y sistodiastólica (SDH).
MétodosAnálisis secundario de datos provenientes de la Encuesta Demográfica y de Salud Familiar de los años 2014-2022. Para el análisis de los factores asociados, se implementó un modelo de regresión de Poisson con varianza robusta con el propósito de calcular las Razones de Prevalencia ajustados (RPa), acompañados de su intervalo de confianza al 95%.
ResultadosLa prevalencia fue del 7,02%, 1,55% y el 3,28% para la ISH, IDH y SDH, respectivamente. La ISH presentó un decaimiento en el año 2022, a diferencia de las otras dos, que parecen estar en aumento. Se encontró asociación estadísticamente significativa en hombres y un incremento del riesgo con la edad para la ISH y SDH, a diferencia de la IDH, donde la edad actúa como factor protector. Se identificaron factores adicionales, incluyendo el tabaquismo y el consumo excesivo de alcohol, mientras que un alto consumo de frutas/verduras ofrecen un efecto protector. La obesidad y la diabetes se asociaron con un mayor riesgo de este, y se observaron variaciones significativas por regiones y altitud, así como entre grupos étnicos.
ConclusionesSe han encontrado diferencias importantes en la prevalencia de los subtipos de HTA, subrayando la heterogeneidad de esta condición crónica, tanto en los factores relacionados como en los cambios de la tendencia de estos a través de los años.
Hypertension (HTN), a multifactorial clinical condition typified by persistently elevated arterial blood pressure, is likely to ultimately result in increased susceptibility to developing various long-term complications involving the cardiovascular, cerebrovascular, and renal body systems, among other consequences, if left untreated, according to medical research.1 The rapidly increasing global ubiquity of HTN presents a formidable test for healthcare frameworks, motivating recent analyses to disentangle the intricacies of HTN and its consequences for public wellness, emphasizing the value of timely administration and preemptive tactics.2,3
While HTN is widely recognized as a global primary threat to cardiovascular health, it is essential to acknowledge that not all HTN is identical. Current medical literature distinguishes between three main subtypes of HTN: isolated systolic hypertension (ISH), isolated diastolic hypertension (IDH), and systolic–diastolic hypertension (SDH).4,5 Each subtype may have different prevalence profiles across age groups, distinct associated risk factors, and potentially different implications for clinical management and long-term health outcomes.6–9
While the medical literature often treats HTN as a single entity, there is a lack of clear distinction on how its specific subtypes are distributed within the population. This generalization overlooks the crucial differences between the three types. A detailed understanding of the prevalence, trend, and associated factors of every kind of HTN is imperative, as the variability in therapeutic management required for each subtype necessitates a personalized approach.10–12 Optimizing treatment strategies based on this differentiation is critical to improving health outcomes in the affected population, emphasizing the importance of a more detailed and specific evaluation of HTN in future studies.
MethodsDesignAn analytical cross-sectional study was conducted through secondary data analysis of the Demographic and Family Health Survey (ENDES) data, provided by the National Institute of Statistics and Informatics (INEI) for the period 2014–2022.13 This analysis followed the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines to ensure quality and transparency in reporting observational studies.14
Population, eligibility criteria, and sampleThe target population of this study included Peruvian individuals aged between 15 and 99 years, covering both urban and rural areas across all 24 departments of the country. ENDES employs a probabilistic, balanced, two-stage, stratified, and independent sampling design at the departmental level and by urban and rural areas. In the first stage, clusters or primary sampling units (PSUs) are selected through systematic sampling with probability proportional to size. In the second stage, households within each PSU are selected via simple systematic sampling. This design ensures that the sample is representative at the national level, by area of residence (urban and rural), by natural region (coast, Highlands, and Jungle), and for each of the country's 24 departments and the Constitutional Province of Callao.13
Individuals aged 18 years or older were selected for analysis, in line with standard definitions of HTN applicable to this age group. Participants not having their blood pressure measured and those reporting a history of HTN were excluded.
Assessment of consistency and plausibility of measurementsCutoff thresholds were defined based on methodologies from previous pooled studies to include only blood pressure measurements considered plausible for analysis. Specifically, systolic blood pressure (SBP) measurements were required to be between 70mmHg and 270mmHg, and diastolic blood pressure (DBP) measurements were between 50mmHg and 150mmHg. Measurements not meeting these plausibility criteria were excluded from the analysis.15
Variables and measurementThe main variables were as follows4,7,16:
- •
Undiagnosed HTN (which will be mentioned simply as HTN) was defined as those with SBP ≥140mmHg and/or DBP ≥90mmHg.
- •
ISH was defined as individuals with SBP ≥140mmHg but with DBP <90mmHg, regardless of previous hypertension diagnosis.
- •
IDH was defined as individuals with DBP ≥90mmHg but with SBP <140mmHg.
- •
SDH was defined as individuals with both SBP ≥140mmHg and DBP ≥90mmHg.
Covariables used were sex (female and male), age categorized in years (18–35 years, 36–59 years, 60–69 years, and 70 years and over), natural region (Metropolitan Lima, rest of the coast, Highlands, and Jungle), educational level (none, primary, secondary, and higher), wealth index (the wealth index is a composite measure of household socioeconomic status, calculated by INEI using principal component analysis; this index is based on the possession of durable goods, housing characteristics, and access to basic services. Households are classified into quintiles: very poor, poor, middle, rich, and very rich, representing the relative socioeconomic level within the studied population), area of residence (urban, rural), smoking status (never smoked, former smoker, current smoker, daily smoker), alcohol consumption was defined by self-report and classified into three categories: (1) never or not used in the last 12 months; (2) non-excessive consumption (≥one occasion in the last 30 days, but <5 drinks for men or <4 for women on one occasion in the last 12 months); and (3) excessive consumption (≥one occasion in the last 30 days and ≥five drinks for men or ≥four drinks for women on one occasion), fruit and vegetable intake over 5 servings per day (yes and no), nutritional status measured through body mass index (BMI=Weight (kg)/Height (m2)) (normal weight if BMI ≤24.99kg/m2, overweight if BMI ≥25–29.99kg/m2, and obesity ≥30kg/m2), abdominal obesity (if waist circumference ≥102 in males or ≥88 in females), self-reported diabetes mellitus type 2 (T2DM) (yes, no), race (Quechua, Aymara, Native or Indigenous Amazonian, Negroid/Black, White/Caucasian, and Mestizo), and altitude (0–499, 500–1499, 1500–2999, and 3000 or more).
ProceduresTo ensure accuracy and reliability in SBP and DBP measurement, a standardized procedure was adopted using an OMRON brand digital blood pressure monitor, model HEM-713. Two types of cuffs were used to accommodate different arm sizes: one for standard-size arms (220–320mm) and another for larger arms (330–430mm).
Blood pressure measurements were taken under controlled conditions, with participants at rest, seated, and with the right arm positioned at heart level on a flat surface. The initial measurement was taken after a five-minute rest period, followed by a second measurement 2min later, allowing the individual's cardiovascular conditions to reach a more stable state. The average of these two measurements for SBP and DBP was calculated for each individual, and this average was used for analyses. This method seeks to reduce momentary fluctuations in blood pressure and provides a more accurate and representative measure.
In addition to the measurements above, the remaining sociodemographic covariates were obtained through standardized questionnaires administered by trained interviewers during the ENDES survey. Sex, age, educational level, race, and area of residence were collected through self-reporting by the participants. The natural region and altitude of residence were determined based on the geographic location of the participant's household. The wealth index was calculated using information on household assets and housing characteristics, following the standard ENDES methodology.
Statistical analysisIn this study, the R 4.03 program will be used for various statistical analyses. Initially, a descriptive analysis of all variables will be conducted, providing an overview of the dataset's characteristics. Subsequently, to delve deeper into the analysis of associated factors, a Poisson regression model with robust variance will be implemented to calculate adjusted prevalence ratios (aPRs), accompanied by their 95% confidence intervals (95% CI). Finally, for result visualization, various trend graphs covering the period from 2014 to 2022 for each type of HTN will be generated.
Ethical considerationsThis study used publicly available, anonymized data accessible at no cost to interested parties, ensuring participant privacy by not including information that could personally identify them, thus eliminating potential ethical risks. INEI, in collecting ENDES data, ensured informed consent was obtained from participants before collecting information through the survey.
The database is publicly available for initial consultation and follow-up,17 offering open access to collected information without personal identifiers and direct contact with the involved human subjects. For these reasons, it was determined that it was not necessary to submit the study for ethics committee evaluation.
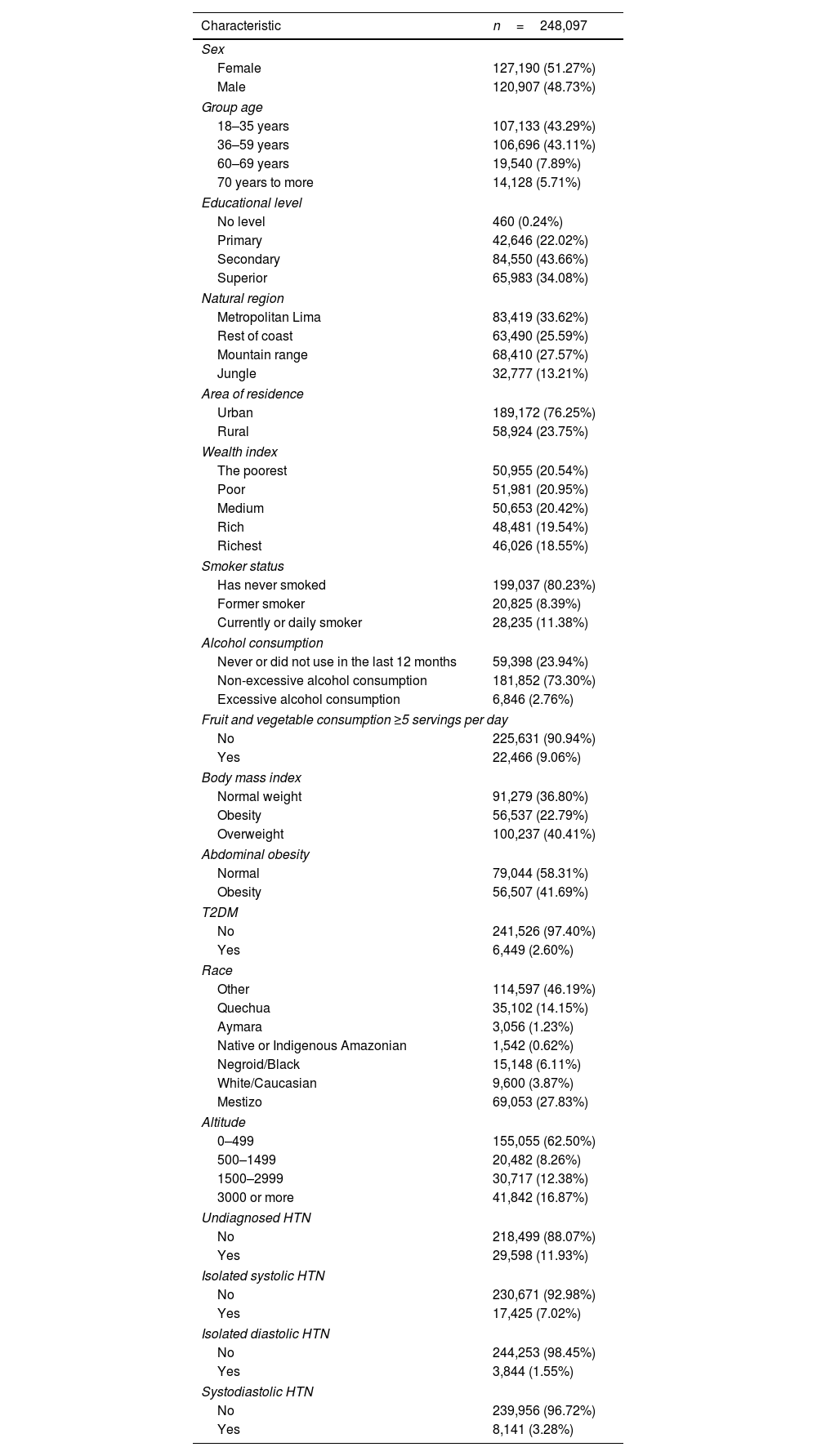
ResultsRegarding the general characteristics of the study sample, 51.27% were women, while 13.60% were older adults. A total of 33.62% resided in Metropolitan Lima, the capital of Peru, and 23.75% lived in rural areas. As for lifestyle factors, 11.38% were current smokers, 2.76% consumed alcohol excessively, and only 9.06% consumed at least 5 daily servings of fruits/vegetables. The prevalence based on BMI and WC was 22.76% and 41.69%, respectively. The rest of the characteristics can be seen in Table 1. Additionally, in supplementary material 1 the distribution of these characteristics according to the type of HTN can be visualized.
Demographic and anthropometric characteristics of participants.
| Characteristic | n=248,097 |
|---|---|
| Sex | |
| Female | 127,190 (51.27%) |
| Male | 120,907 (48.73%) |
| Group age | |
| 18–35 years | 107,133 (43.29%) |
| 36–59 years | 106,696 (43.11%) |
| 60–69 years | 19,540 (7.89%) |
| 70 years to more | 14,128 (5.71%) |
| Educational level | |
| No level | 460 (0.24%) |
| Primary | 42,646 (22.02%) |
| Secondary | 84,550 (43.66%) |
| Superior | 65,983 (34.08%) |
| Natural region | |
| Metropolitan Lima | 83,419 (33.62%) |
| Rest of coast | 63,490 (25.59%) |
| Mountain range | 68,410 (27.57%) |
| Jungle | 32,777 (13.21%) |
| Area of residence | |
| Urban | 189,172 (76.25%) |
| Rural | 58,924 (23.75%) |
| Wealth index | |
| The poorest | 50,955 (20.54%) |
| Poor | 51,981 (20.95%) |
| Medium | 50,653 (20.42%) |
| Rich | 48,481 (19.54%) |
| Richest | 46,026 (18.55%) |
| Smoker status | |
| Has never smoked | 199,037 (80.23%) |
| Former smoker | 20,825 (8.39%) |
| Currently or daily smoker | 28,235 (11.38%) |
| Alcohol consumption | |
| Never or did not use in the last 12 months | 59,398 (23.94%) |
| Non-excessive alcohol consumption | 181,852 (73.30%) |
| Excessive alcohol consumption | 6,846 (2.76%) |
| Fruit and vegetable consumption ≥5 servings per day | |
| No | 225,631 (90.94%) |
| Yes | 22,466 (9.06%) |
| Body mass index | |
| Normal weight | 91,279 (36.80%) |
| Obesity | 56,537 (22.79%) |
| Overweight | 100,237 (40.41%) |
| Abdominal obesity | |
| Normal | 79,044 (58.31%) |
| Obesity | 56,507 (41.69%) |
| T2DM | |
| No | 241,526 (97.40%) |
| Yes | 6,449 (2.60%) |
| Race | |
| Other | 114,597 (46.19%) |
| Quechua | 35,102 (14.15%) |
| Aymara | 3,056 (1.23%) |
| Native or Indigenous Amazonian | 1,542 (0.62%) |
| Negroid/Black | 15,148 (6.11%) |
| White/Caucasian | 9,600 (3.87%) |
| Mestizo | 69,053 (27.83%) |
| Altitude | |
| 0–499 | 155,055 (62.50%) |
| 500–1499 | 20,482 (8.26%) |
| 1500–2999 | 30,717 (12.38%) |
| 3000 or more | 41,842 (16.87%) |
| Undiagnosed HTN | |
| No | 218,499 (88.07%) |
| Yes | 29,598 (11.93%) |
| Isolated systolic HTN | |
| No | 230,671 (92.98%) |
| Yes | 17,425 (7.02%) |
| Isolated diastolic HTN | |
| No | 244,253 (98.45%) |
| Yes | 3,844 (1.55%) |
| Systodiastolic HTN | |
| No | 239,956 (96.72%) |
| Yes | 8,141 (3.28%) |
n (%).
Regarding the overall prevalence of the types of HTN presented in Fig. 1, 11.93% had undiagnosed HTN, while 7.02%, 1.55%, and 3.28% had ISH, IDH, and SDH, respectively. In terms of trends, there has been an increase in the prevalence of undiagnosed HTN over the years, with a slight decrease in 2022; regarding ISH, it showed a decline in the year 2022, unlike the other two, which seems to be increasing.
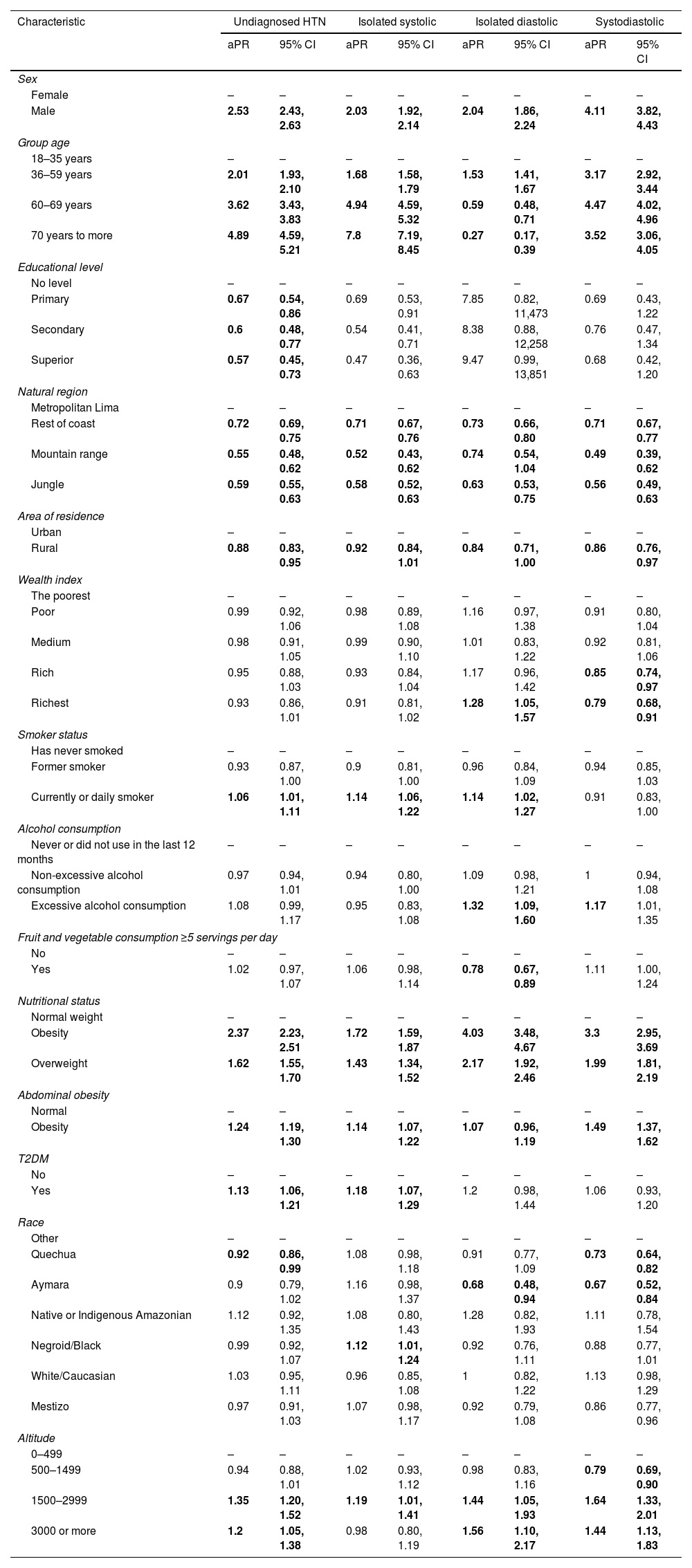
The multivariable analysis of Table 2 found that males had a higher risk of presenting any HTN, especially SDH. However, regarding age, it was found that older age was associated with a higher risk of undiagnosed HTN, ISH, and SDH; this was not the case for those with IDH, as older age acted as a protective factor. On the other hand, it was found that different regions of the country had a lower probability of presenting any of the types of HTN compared to those living in Metropolitan Lima. The same occurred with living in rural areas. Isolatedly, the wealthy and very wealthy economic classes seemed to have a protective effect against presenting SDH.
Multivariable regression analysis of the factors associated with the different types of HTN.
| Characteristic | Undiagnosed HTN | Isolated systolic | Isolated diastolic | Systodiastolic | ||||
|---|---|---|---|---|---|---|---|---|
| aPR | 95% CI | aPR | 95% CI | aPR | 95% CI | aPR | 95% CI | |
| Sex | ||||||||
| Female | – | – | – | – | – | – | – | – |
| Male | 2.53 | 2.43, 2.63 | 2.03 | 1.92, 2.14 | 2.04 | 1.86, 2.24 | 4.11 | 3.82, 4.43 |
| Group age | ||||||||
| 18–35 years | – | – | – | – | – | – | – | – |
| 36–59 years | 2.01 | 1.93, 2.10 | 1.68 | 1.58, 1.79 | 1.53 | 1.41, 1.67 | 3.17 | 2.92, 3.44 |
| 60–69 years | 3.62 | 3.43, 3.83 | 4.94 | 4.59, 5.32 | 0.59 | 0.48, 0.71 | 4.47 | 4.02, 4.96 |
| 70 years to more | 4.89 | 4.59, 5.21 | 7.8 | 7.19, 8.45 | 0.27 | 0.17, 0.39 | 3.52 | 3.06, 4.05 |
| Educational level | ||||||||
| No level | – | – | – | – | – | – | – | – |
| Primary | 0.67 | 0.54, 0.86 | 0.69 | 0.53, 0.91 | 7.85 | 0.82, 11,473 | 0.69 | 0.43, 1.22 |
| Secondary | 0.6 | 0.48, 0.77 | 0.54 | 0.41, 0.71 | 8.38 | 0.88, 12,258 | 0.76 | 0.47, 1.34 |
| Superior | 0.57 | 0.45, 0.73 | 0.47 | 0.36, 0.63 | 9.47 | 0.99, 13,851 | 0.68 | 0.42, 1.20 |
| Natural region | ||||||||
| Metropolitan Lima | – | – | – | – | – | – | – | – |
| Rest of coast | 0.72 | 0.69, 0.75 | 0.71 | 0.67, 0.76 | 0.73 | 0.66, 0.80 | 0.71 | 0.67, 0.77 |
| Mountain range | 0.55 | 0.48, 0.62 | 0.52 | 0.43, 0.62 | 0.74 | 0.54, 1.04 | 0.49 | 0.39, 0.62 |
| Jungle | 0.59 | 0.55, 0.63 | 0.58 | 0.52, 0.63 | 0.63 | 0.53, 0.75 | 0.56 | 0.49, 0.63 |
| Area of residence | ||||||||
| Urban | – | – | – | – | – | – | – | – |
| Rural | 0.88 | 0.83, 0.95 | 0.92 | 0.84, 1.01 | 0.84 | 0.71, 1.00 | 0.86 | 0.76, 0.97 |
| Wealth index | ||||||||
| The poorest | – | – | – | – | – | – | – | – |
| Poor | 0.99 | 0.92, 1.06 | 0.98 | 0.89, 1.08 | 1.16 | 0.97, 1.38 | 0.91 | 0.80, 1.04 |
| Medium | 0.98 | 0.91, 1.05 | 0.99 | 0.90, 1.10 | 1.01 | 0.83, 1.22 | 0.92 | 0.81, 1.06 |
| Rich | 0.95 | 0.88, 1.03 | 0.93 | 0.84, 1.04 | 1.17 | 0.96, 1.42 | 0.85 | 0.74, 0.97 |
| Richest | 0.93 | 0.86, 1.01 | 0.91 | 0.81, 1.02 | 1.28 | 1.05, 1.57 | 0.79 | 0.68, 0.91 |
| Smoker status | ||||||||
| Has never smoked | – | – | – | – | – | – | – | – |
| Former smoker | 0.93 | 0.87, 1.00 | 0.9 | 0.81, 1.00 | 0.96 | 0.84, 1.09 | 0.94 | 0.85, 1.03 |
| Currently or daily smoker | 1.06 | 1.01, 1.11 | 1.14 | 1.06, 1.22 | 1.14 | 1.02, 1.27 | 0.91 | 0.83, 1.00 |
| Alcohol consumption | ||||||||
| Never or did not use in the last 12 months | – | – | – | – | – | – | – | – |
| Non-excessive alcohol consumption | 0.97 | 0.94, 1.01 | 0.94 | 0.80, 1.00 | 1.09 | 0.98, 1.21 | 1 | 0.94, 1.08 |
| Excessive alcohol consumption | 1.08 | 0.99, 1.17 | 0.95 | 0.83, 1.08 | 1.32 | 1.09, 1.60 | 1.17 | 1.01, 1.35 |
| Fruit and vegetable consumption ≥5 servings per day | ||||||||
| No | – | – | – | – | – | – | – | – |
| Yes | 1.02 | 0.97, 1.07 | 1.06 | 0.98, 1.14 | 0.78 | 0.67, 0.89 | 1.11 | 1.00, 1.24 |
| Nutritional status | ||||||||
| Normal weight | – | – | – | – | – | – | – | – |
| Obesity | 2.37 | 2.23, 2.51 | 1.72 | 1.59, 1.87 | 4.03 | 3.48, 4.67 | 3.3 | 2.95, 3.69 |
| Overweight | 1.62 | 1.55, 1.70 | 1.43 | 1.34, 1.52 | 2.17 | 1.92, 2.46 | 1.99 | 1.81, 2.19 |
| Abdominal obesity | ||||||||
| Normal | – | – | – | – | – | – | – | – |
| Obesity | 1.24 | 1.19, 1.30 | 1.14 | 1.07, 1.22 | 1.07 | 0.96, 1.19 | 1.49 | 1.37, 1.62 |
| T2DM | ||||||||
| No | – | – | – | – | – | – | – | – |
| Yes | 1.13 | 1.06, 1.21 | 1.18 | 1.07, 1.29 | 1.2 | 0.98, 1.44 | 1.06 | 0.93, 1.20 |
| Race | ||||||||
| Other | – | – | – | – | – | – | – | – |
| Quechua | 0.92 | 0.86, 0.99 | 1.08 | 0.98, 1.18 | 0.91 | 0.77, 1.09 | 0.73 | 0.64, 0.82 |
| Aymara | 0.9 | 0.79, 1.02 | 1.16 | 0.98, 1.37 | 0.68 | 0.48, 0.94 | 0.67 | 0.52, 0.84 |
| Native or Indigenous Amazonian | 1.12 | 0.92, 1.35 | 1.08 | 0.80, 1.43 | 1.28 | 0.82, 1.93 | 1.11 | 0.78, 1.54 |
| Negroid/Black | 0.99 | 0.92, 1.07 | 1.12 | 1.01, 1.24 | 0.92 | 0.76, 1.11 | 0.88 | 0.77, 1.01 |
| White/Caucasian | 1.03 | 0.95, 1.11 | 0.96 | 0.85, 1.08 | 1 | 0.82, 1.22 | 1.13 | 0.98, 1.29 |
| Mestizo | 0.97 | 0.91, 1.03 | 1.07 | 0.98, 1.17 | 0.92 | 0.79, 1.08 | 0.86 | 0.77, 0.96 |
| Altitude | ||||||||
| 0–499 | – | – | – | – | – | – | – | – |
| 500–1499 | 0.94 | 0.88, 1.01 | 1.02 | 0.93, 1.12 | 0.98 | 0.83, 1.16 | 0.79 | 0.69, 0.90 |
| 1500–2999 | 1.35 | 1.20, 1.52 | 1.19 | 1.01, 1.41 | 1.44 | 1.05, 1.93 | 1.64 | 1.33, 2.01 |
| 3000 or more | 1.2 | 1.05, 1.38 | 0.98 | 0.80, 1.19 | 1.56 | 1.10, 2.17 | 1.44 | 1.13, 1.83 |
Each factor has been independently adjusted for sex, group age, natural region, area of residence, education, wealth index, smoker status, alcohol consumption, nutritional status, obesity abdominal, T2DM, consumption of fruits and vegetables, race and altitude. aRP: adjusted prevalence ratio; 95% CI: 95% confidence interval.
Current smokers had a higher risk of presenting any HTN, except for SDH. Those who consumed alcohol excessively were more likely to present IDH and SDH. Those consuming more than five portions of fruits/vegetables daily were less likely to present IDH. Regarding obesity by BMI or WC, there was a higher probability of presenting any HTN. Moreover, patients with T2DM were more likely to have undiagnosed HTN and ISH.
Regarding race, Quechuas and Aymaras were less likely to present undiagnosed HTN, IDH, and SDH. Meanwhile, those of Black race were more likely to have ISH. Finally, higher altitude was generally associated with a higher probability of presenting some HTN.
DiscussionThe observed shifts in HTN subtype trends suggest significant changes in public health dynamics and intervention effectiveness. The decline in ISH prevalence, particularly notable in 2022, might reflect the success of targeted interventions for older populations. These interventions, including exercise programs and promotion of healthy diets, have shown effectiveness in reducing systolic blood pressure.18,19 This trend could indicate the partial success of public health strategies in addressing this specific HTN subtype in the elderly.
Conversely, the increase in the prevalence of IDH and SDH, more common in younger populations, could be attributed to evolving lifestyle factors. The rise in obesity rates and increasingly sedentary behaviors, particularly among younger adults, may contribute to this trend. Recent research indicates these risk factors are becoming more prevalent in the general population, potentially explaining the uptick in these forms of HTN.10,19 It is important to note that the underlying pathophysiological mechanisms and risk factors may differ among HTN types, necessitating age- and subtype-specific approaches to prevention and management.
Furthermore, the growing prevalence of IDH, previously considered less common and of lower risk, is gaining recognition for its association with long-term cardiovascular risks, especially in young and middle-aged adults.9,20 This shift in understanding underscores the need for increased attention to this subtype in younger populations.
These divergent trends highlight the complexity of HTN epidemiology and emphasize the importance of tailored public health strategies. While interventions for older adults seem to be yielding positive results in reducing ISH, it is evident that additional efforts and potentially different approaches are needed to address the increase in IDH and SDH in younger populations. Future research and public health initiatives should focus on developing and implementing targeted interventions that consider the specific characteristics and risk factors associated with each HTN subtype across different age groups.
The results suggest that HTN determinants are not uniform across its subtypes. The greater predisposition of men to develop any HTN, particularly SDH, aligns with existing literature indicating gender differences in cardiovascular physiology and HTN risk factors.3,21,22 However, discrepancies exist regarding other studies that suggest women exhibit a more pronounced elevation in blood pressure.10,23 These discrepancies can be explained by several factors specific to the Peruvian population, including genetic, dietary, and lifestyle factors and socioeconomic and cultural elements such as differences in gender roles and access to healthcare. Moreover, our focus on specific HTN subtypes might reveal patterns that are not evident when HTN is considered a single category. It is important to consider that Peru, like many developing countries, is undergoing an epidemiological transition, which could be changing HTN patterns by gender as the population adopts more urbanized lifestyles.
The relationship between age and HTN type highlights exciting patterns. While advanced age is associated with a higher risk of ISH and SDH, a protective effect was observed in IDH. The pathophysiological mechanisms may involve aging-related arterial stiffness and vascular elasticity loss contributing to increased systolic pressure, while diastolic pressure may decrease or stabilize.22,24,25 The interaction between age and gender plays a crucial role, as the relationship between gender and blood pressure may vary with age. Although our study did not specifically analyze the impact of menopause, this factor could influence the observed gender differences, especially in older age groups. These observations underscore the complexity of the relationship between gender, age, and HTN, highlighting the need for further research considering context-specific factors of the Peruvian population. Future studies could benefit from a more detailed analysis of how sociocultural, biological, and environmental factors interact with gender and age to influence HTN patterns across different populations and life stages.
The analysis also revealed that living outside Metropolitan Lima and in rural areas is associated with a lower likelihood of presenting any HTN. This finding could reflect differences in lifestyles, exposure to environmental factors, and access to health services between urban and rural areas. A study by Miranda et al. highlights how urbanization and associated lifestyles can increase HTN risk.26
The observation that smoking increases the risk of all HTN types, except for SDH, suggests a complex relationship between smoking and blood pressure dynamics. Unlike previous studies that showed a direct relationship between smoking and an increased risk of HTN in general, our results indicate that the impact of smoking may vary by HTN type. This could be due to tobacco's differentiated effects on vascular function and arterial stiffness, necessitating further research to fully understand its role in SDH.27,28
The link between excessive alcohol consumption and a higher risk of IDH and SDH highlights alcohol's role in disrupting blood pressure regulation. Alcohol is known to affect the cardiovascular system, including endothelial function alterations and vascular tone regulation, which could explain its association with these specific HTN types. Research into reducing alcohol intake corresponds with claims that it may prove advantageous towards both preventing and handling HTN.29,30
The protective impacts of a diet abundant in fruits and vegetables against IDH may be due to the advantages of consuming foods packed with essential nutrients, antioxidants, and fiber which effectively support cardiovascular well-being. Research has revealed that eating more fruits and vegetables in one's diet is linked to decreased blood pressure readings, potentially as a result of beneficial modifications to how blood vessels work and decreased rigidity in the arteries. This may also indicate that consuming these can specifically protect against certain types of HTN.31,32
The association of obesity, measured by both BMI and WC, with an increased risk of all HTN types, underscores obesity as a critical risk factor for HTN. Through various mechanisms such as insulin resistance, systemic inflammation, and alterations in renal and endothelial function that collectively emphasize the significance of weight management for HTN prevention, obesity has been shown to contribute to the onset of HTN.28,33
Our results indicate a higher likelihood of undiagnosed HTN in patients with T2DM, which is an unexpected and concerning finding, considering that these patients typically have more frequent health check-ups. This observation merits deeper analysis. The higher prevalence of ISH in patients with T2DM highlights the interconnection between both pathologies. Diabetes can exacerbate HTN risk through insulin resistance, endothelial dysfunction, and the accumulation of advanced glycation end-products, specifically affecting endothelial stiffness and increasing myocardial contraction force, leading to an increase in SBP.34,35 Several hypotheses could explain this finding. Firstly, it could reflect deficiencies in the primary care system, where the focus on glycemic control might overshadow the detection and adequate management of HTN in diabetic patients. Gedebjerg et al. found that up to 24% of patients with newly diagnosed diabetes had previously undetected HTN.36
This finding could indicate a more rapid or silent progression of HTN in patients with T2DM, possibly due to shared pathophysiological mechanisms. Petrie et al. described how insulin resistance, endothelial dysfunction, and oxidative stress contribute to T2DM and HTN.37 Chronic hyperglycemia can exacerbate arterial stiffness and alter blood pressure regulation, as demonstrated by Climie et al.38 Our study is based on point measurements of blood pressure, which may not fully capture blood pressure variability in diabetic patients. Parati et al. emphasized the importance of ambulatory blood pressure monitoring in patients with T2DM to detect abnormal patterns that might be overlooked in office measurements.39 These findings underscore the need to improve surveillance and comprehensive management of patients with T2DM, particularly emphasizing early detection and control of HTN.
The higher likelihood of having ISH in patients with T2DM highlights the interconnection between both pathologies. Diabetes can exacerbate HTN risk through insulin resistance, endothelial dysfunction, and the accumulation of advanced glycation end-products, reinforcing the need for integrated management of both conditions, specifically affecting endothelial stiffness and increasing myocardial contraction force, leading specifically to an increase in SBP.34,35
The findings regarding ethnic differences in HTN prevalence underscore the importance of considering genetic and cultural diversity in HTN study and management. The finding that individuals of Quechua and Aymara origin are less likely to suffer from IDH and SDH suggests that genetic factors or lifestyles associated with these communities may confer a degree of protection against these forms of HTN. Conversely, the higher prevalence of ISH among Black individuals highlights the need for public health strategies that address ethnic disparities in HTN risk.40,41 This finding emphasizes the importance of implementing personalized and culturally sensitive public health approaches that not only consider general recommendations for HTN prevention and management but also tailor to the specific needs of different ethnic groups. Promoting further research to explore in depth the genetic bases and lifestyle factors contributing to these ethnic differences in HTN prevalence may facilitate the development of more effective and targeted interventions, thus contributing to health equity.
While demographic, socioeconomic, and geographical elements hold significance for HTN prevention and management, these findings especially underscore the necessity of encouraging a lifestyle emphasizing smoking cessation, moderate alcohol intake, a diet rich in fruits and vegetables, weight maintenance, and appropriate diabetes care to promote wellness. Public health interventions aiming to reduce the burden of all HTN types would be most effective if they prioritized lifestyle modifications tailored specifically to the varying needs and risk profiles of diverse population groups.
Contribution in public healthThis research reflects the underlying complexity in the epidemiology of HTN, emphasizing the importance of distinguishing between different types of hypertension for accurate diagnosis and appropriate therapeutic management. This study highlights the necessity of tailoring screening and preventative tactics to account for the idiosyncrasies uncovered in the prevalence patterns of distinct HTNs, with personalized strategies considering demographic particulars like age and gender alongside lifestyle habits encompassing the usage of tobacco and alcohol and dietary selections.
Thus, by observing a lower likelihood of presenting HTN in regions outside of Metropolitan Lima and in rural areas, as well as the protective effect of a higher economic position on IDH, the manuscript highlights the importance of addressing socioeconomic disparities and access to health services in public health strategies to combat HTN. Meanwhile, the association found between lifestyle, including tobacco and alcohol consumption, obesity, and T2DM, with the prevalence of different types of HTN underscores the importance of promoting healthy living habits as a central pillar in hypertension prevention.
Through illuminating the tendency to underestimate and underdiagnose high blood pressure within broader society, especially where it remains unseen, the report makes a pressing plea to better develop early discovery tactics and entry to healthcare services. By both enabling early interventions to diminish the frequency of high blood pressure while also helping to curb potential long-term issues linked to poorly regulated hypertension, such as cardiovascular illnesses, kidney deterioration, and brain attacks, this method could serve to dually curb prevalence and complications.
This manuscript makes an exceptionally meaningful addition to the current understanding of health technology assessment and its governance in matters concerning public health. This provides fertile ground for further exploration and the crafting of more discerning and impactful healthcare directives going forward. By determining which risk factors and how prevalence may change for various hypertensive artery types, public health officials can design interventions focused on where needs are greatest, allowing efforts to make a society increasingly robust against this long-term illness by lessening its widespread influence.
LimitationsThis study has several limitations. First, the cross-sectional design prevents us from establishing causality between the identified factors and HTN subtypes. Second, there is potential bias due to self-reported data, particularly concerning lifestyle factors. Third, while information on certain possible skewing factors, like dietary sodium consumption and exercise habits, was absent which could have impacted outcomes, the lack of data on some potential confounders may have influenced the results.
ConclusionThis research offers meaningful understanding of the frequency and influencing factors of distinctive high blood pressure classifications within a Peruvian community. The findings underscore the necessity of carefully crafted public health initiatives considering diverse demographic segments’ unique needs and vulnerabilities. Addressing lifestyle factors, promoting healthy behaviors, and considering demographic and socioeconomic disparities are crucial steps in reducing the burden of HTN. Further investigation is required to examine the causal links discovered and craft more impactful approaches for avoidance and treatment.
CRediT authorship contribution statementVíctor Juan Vera-Ponce: Conceptualization, Investigation, Methodology, Resources, Writing – Original draft, Writing – Review & Editing.
Fiorella E. Zuzunaga-Montoya: Investigation, Project administration, Writing – Original draft, Writing – Review & Editing.
Luisa Erika Milagros Vásquez-Romero: Investigation, Resources, Writing – Original draft, Writing – Review & Editing.
Joan A. Loayza-Castro: Software, Data curation, Formal analysis, Writing – Review & Editing.
Carmen Inés Gutierrez De Carrillo: Validation, Visualization, Writing – Original draft, Writing – Review & Editing.
Enrique Vigil-Ventura: Methodology, Supervision, Funding acquisition, Writing – Review & Editing.
Informed consentIt was not necessary to obtain informed consent in this study.
FundingThis study is self-financed.
Conflict of interestThe authors declare no conflict of interest.
AcknowledgmentsA special thanks to the members of Instituto de Investigación de Enfermedades Tropicales, Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas (UNTRM), Amazonas, Perú who provided valuable comments during the preparation of this study.
Data availabilityThe data supporting the findings of this study can be accessed in the follow link: https://proyectos.inei.gob.pe/microdatos/.