Changes in various cytokine activities have been reported during both HBV and HCV infections, while an imbalance of pro-inflammatory and anti-inflammatory cytokine production influences their immunopathogenesis. The aims of the present study are (a) to measure serum levels of interleukin-6 (IL-6), tumor necrosis factor α (TNF-α), interleukin-10 (IL-10), interleukin-2 (IL-2) and interleukin-4 (IL-4) in a sample of patients affected either by chronic HBV infection or by chronic HCV infection and in healthy controls (b) to correlate serum levels of IL-6, TNF-α, IL-10, IL-2 and IL-4 with biochemical markers of liver disease and (c) to evaluate differences of the aforementioned cytokines between HBV and HCV patients, as well as between patients and healthy controls.
MethodsThe study population consisted of 50 patients with chronic hepatitis B, 40 patients with chronic hepatitis C and 30 healthy controls aged between 28 and 75 years. Biochemical markers of liver disease were evaluated by routine methods approved by IFCC. Serum concentrations of IL-6, TNF-α, IL-10, IL-2 and IL-4 were determined with the Human Cytokine/Chemokine Panel I Merck Millipore.
ResultsHBV patients showed statistically significant difference in TNF-α and IL-2 levels, versus healthy controls. HCV patients showed statistically significant difference in TNF-α, IL-10 and IL-2 levels versus healthy controls. IL10 and IL-2 levels were significantly different between HBV and HCV patients.
ConclusionsThis study evaluated the serum cytokine levels (IL-6, TNF-α, IL-10, IL-2 and IL-4) of chronic hepatitis B or C patients, as well as the differences in such levels between patients and healthy controls. Correlations of cytokine levels with biochemical markers of liver disease were also observed, reflecting the degree of activity of the inflammatory process in the liver.
Tanto en las infecciones por VHB como por VHC se han notificado cambios en las diversas actividades de las citocinas, y es conocido que su inmunopatogénesis está influida por un desequilibrio en la producción de citocinas pro y antiinflamatorias. Los objetivos del presente estudio son: a) medir las concentraciones séricas de interleucina 6 (IL-6), factor de necrosis tumoral α (TNF-α), interleucina 10 (IL-10), interleucina 2 (IL-2) e interleucina 4 (IL-4) en una muestra de pacientes afectados, ya sea por una infección crónica por VHB o por VHC y en controles sanos; b) correlacionar las concentraciones séricas de IL-6, TNF-α, IL-10, IL-2 e IL-4 con los marcadores bioquímicos de enfermedad hepática, y c) evaluar las diferencias de las citocinas antes mencionadas entre los pacientes con VHB y con HCV, así como entre los pacientes y los controles sanos.
MétodosLa población del estudio consistió en 50 pacientes con hepatitis B crónica, 40 pacientes con hepatitis C crónica y 30 controles sanos de edades comprendidas entre 28 y 75 años. Se evaluaron los marcadores bioquímicos de la enfermedad hepática mediante métodos rutinarios aprobados por la IFCC. Las concentraciones séricas de IL-6, TNF-α, IL-10, IL-2 e IL-4 se determinaron mediante el Panel I de citocinas/quimiocinas humanas de Merck Millipore.
ResultadosLos pacientes con VHB mostraron diferencias estadísticamente significativas en las concentraciones de TNF-α e IL-2, comparadas con las de controles sanos. Los pacientes con HCV mostraron diferencias estadísticamente significativas en TNF-α, IL-10 e IL-2 respecto a las concentraciones de los controles sanos. Las concentraciones de IL-10 e IL-2 fueron significativamente diferentes entre los pacientes con VHB y con HCV.
ConclusionesEste estudio evaluó las concentraciones séricas de citocinas (IL-6, TNF-α, IL-10, IL-2 e IL-4) de pacientes con hepatitis crónica B o C, así como las diferencias en dichas concentraciones entre pacientes y controles sanos. También se observaron correlaciones de las concentraciones de citocinas con marcadores bioquímicos de la enfermedad hepática, lo que refleja el grado de actividad del proceso inflamatorio en el hígado.
Hepatitis B virus (HBV) and hepatitis C virus (HCV) infections constitute serious global health problems due to their high morbidity and mortality. It is estimated that 2 billion people worldwide have been infected with HBV, among which 350 million are chronically infected.1–3 It is also estimated that about 200 million people are infected with HCV, among which 170 million are chronically infected.4,5 Chronic HBV and HCV infections can have severe consequences including debilitating symptoms, impaired quality of life, disability, costly health care expenditures and death. More than 600,000 deaths are attributed to HBV infection annually, while more than 350,000 deaths are attributed to HCV infection annually. Most of these deaths are caused by liver cirrhosis and hepatocellular carcinoma.2,6–8 However, the pathogenesis of liver damage during chronic HBV and HCV infections is not fully understood. Although HBV and HCV are both hepatotropic viruses, they differ in the way they interact with the host immune system. In particular, HBV establishes chronic infection mainly by infecting neonates, but it is controlled by most newly infected adults. On the other hand, in the case of HCV, chronic infection occurs in 75% to 85% of the infected individuals.9 The reasons for viral persistence of these two viruses and transformation from acute to chronic infection are not clear, but it is known that both viral and host characteristics can influence the outcome of the infection.9,10 The host response to hepatitis viruses involves various components of the immune system, including T-lymphocyte immune-regulatory cytokines. Cytokines are a group of protein molecules involved in various biological processes including growth, differentiation, cell survival, hematopoiesis, immunological functions, inflammation, apoptosis, necrosis and fibrosis.11,12 The cytokine group is highly heterogeneous and consists of different types of molecules, such as the interleukins, the tumor necrosis factor family, the interferons, the chemokines, the transforming growth factor-b and others. The control of cytokine production is highly complex, while the effects of cytokines are widespread throughout multiple regulatory molecule networks. Cytokines are produced by a wide variety of cells, mainly the Th1 and Th2 cells. Th1 cells secrete pro-inflammatory cytokines, whereas the Th2 cells secrete anti-inflammatory cytokines. Th1 cytokines are involved in cell-mediated immunity, and play a crucial role in protection from intracellular pathogens and are associated with recovery. Th2 cytokines regulate humoral immune responses, and their rising levels are often associated with the development of persistent infections.11–13 The liver is a major organ in the production of cytokines. Cytokines are involved in physiologic and pathologic processes occurring in the liver. They play an important role in liver growth and regeneration, as well as in inflammatory processes including viral liver disease, in liver fibrosis and cirrhosis.11,12 They can recognize virus-infected cells and can regulate the immunological and inflammatory responses, viral clearance and tissue damage mechanisms. Changes in various cytokine activities have been reported during both HBV and HCV infections, while an imbalance of pro-inflammatory and anti-inflammatory cytokine production influences their immunopathogenesis.9,13 In particular, alterations in serum and intrahepatic Th1 and Th2 cytokine patterns play a critical role in viral persistence, as well as in host immune response, in liver damage and liver disease progression from chronic hepatitis to hepatocellular carcinoma.14–17 Given that cytokines are involved in many processes occurring in the liver which impact on the development of chronic hepatitis, it is of interest to study their levels in chronic hepatitis patients and their correlation with markers of liver disease.
The aims of the present study are (a) to measure serum levels of interleukin-6 (IL-6), tumor necrosis factor α (TNF-α), interleukin-10 (IL-10), interleukin-2 (IL-2) and interleukin-4 (IL-4) in a sample of patients affected either by chronic HBV infection or by chronic HCV infection and in healthy controls (b) to correlate serum levels of IL-6, TNF-α, IL-10, IL-2 and IL-4 with biochemical markers of liver disease and (c) to evaluate differences of the aforementioned cytokines between HBV and HCV patients as well as between patients and healthy controls.
Materials and methodsThe study population consisted of 50 patients with chronic hepatitis B (27 men and 23 women), 40 patients with chronic hepatitis C (32 men and 8 women) and 30 healthy controls (15 men and 15 women) aged between 28 and 75 years (mean age 49.2 years). Patients were recruited from the Internal Medicine Department, of Asklipieio Voulas General Hospital, during a three-year period of time. Patients with chronic hepatitis B were HBsAg (+), anti-HBc (+), anti-HBe (+), HBVDNA (+) by PCR, anti-HCV (−) and anti-HDV (−). Patients with chronic hepatitis C were anti-HCV (+), HCVRNA (+) by PCR, HBsAg (−), anti-HBc (−) and anti-HDV (−). All patients had liver histology consistent with chronic hepatitis. Presence of co-infection with human immunodeficiency virus was excluded in all patients in this study. Exclusion criteria also included co-existence of other causes of chronic liver disease, alcohol consumption and a history of immunosuppressive or antiviral therapy. The controls incorporated in the study were blood donors without any clinical history of hepatitis and were considered healthy through routine laboratory analysis.
Blood samples were collected by venipuncture and allowed to clot at room temperature for 30min. After centrifugation for 10min at 3000×g the sera were separated, aliquoted and then frozen at −70°C. Freeze/thaw cycles of the samples were completely avoided. When assayed, samples were thawed completely, mixed well by vortex and centrifuged to remove particulates. The study was approved by the Medical Ethics Committee of Attikon University Hospital and was conformant to the ethical guidelines of the Declaration of Helsinki.
Serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT) and total bilirubin levels were measured on Siemens ADVIA 1800 fully automated analyzer (Siemens, Erlangen, Germany) at the Biochemistry Laboratory of Asklipieio Voulas General Hospital. Measurements were performed by routine methods approved by IFCC. The upper limit of ALT activity was set at 35IU/L, of AST at 37IU/L, of ALP at 104IU/L, of GGT 38IU/L and of total bilirubin at 1.00mg/dL.
Serum concentrations of IL-6, TNF-α, IL-10, IL-2 and IL-4 were determined with the Human Cytokine/Chemokine Panel I Merck Millipore (Cat. No. MPXHCYTO-60K, Millipore Corporation, Billerica), according to the manufacturer's instructions on the Luminex fully automated analyzer. Luminex uses a bead-based technology whose principles are as follows: using proprietary techniques it internally color-codes microspheres with two fluorescent dyes. Through precise selection of the concentrations of these dyes, distinctly colored bead sets can be created, each of which is coated with a specific capture antibody. After an analyte from a test sample is captured by the bead, a biotinylated detection antibody is introduced. The reaction mixture is then incubated with streptavidin-PE conjugate, serving as the reporter molecule, to complete the reaction on the surface on each microsphere. The microspheres are allowed to pass rapidly through a laser that excites the internal dyes marking the microsphere set. A second laser excites PE, i.e. the fluorescent dye on the reporter molecule. Finally, high-speed digital-signals identify each individual microsphere and quantify the result of its bioassay based on fluorescent reporter signals.
The assay procedure was given briefly as follows: The filter plate was prewashed with 200μL Wash buffer on a plate shaker for 10min at room temperature. Wash buffer was removed by vacuum and 25μL of standards, controls, assay buffer, matrix solution and serum sample were added into the appropriate wells. 25μL of the beads were added to each well. The plate was incubated with agitation overnight (for 16–18h) at 4°C. After several washes, 25μL of detection antibodies were added and were incubated for 1h at room temperature followed by the addition of 25μL streptavidin-phycoerythrin and 30min incubation. Finally 150μL of sheath fluid were added to each well and the beads were resuspended for 5min on a plate shaker. The analysis was performed on the Luminex 200™ platform (Luminex Corporation). IL-6, TNF-α, IL-10, IL-2 and IL-4 serum concentrations were automatically calculated from standard curves. These concentrations were measured in duplicate in all patients. Serum concentrations of IL-6, TNF-α, IL-10, IL-2 and IL-4 were measured at the Department of Cytopathology of Attikon University Hospital being EN ISO 9001:2000 certified.
Statistical analysisCorrelations between pairs of variables were studied by linear regression analysis. Pearson correlation (r) was measured to estimate correlation between pairs comprising: two different cytokines (all possible pairs) and biochemical parameters, two different groups of patients (all possible pairs). The differences between HBV and HCV patients and the differences between patients and healthy controls were analyzed by means of hypothesis testing for the equality or not of the means. They were evaluated by means of Student t-test, and p values lower than 0.05 were considered significant.
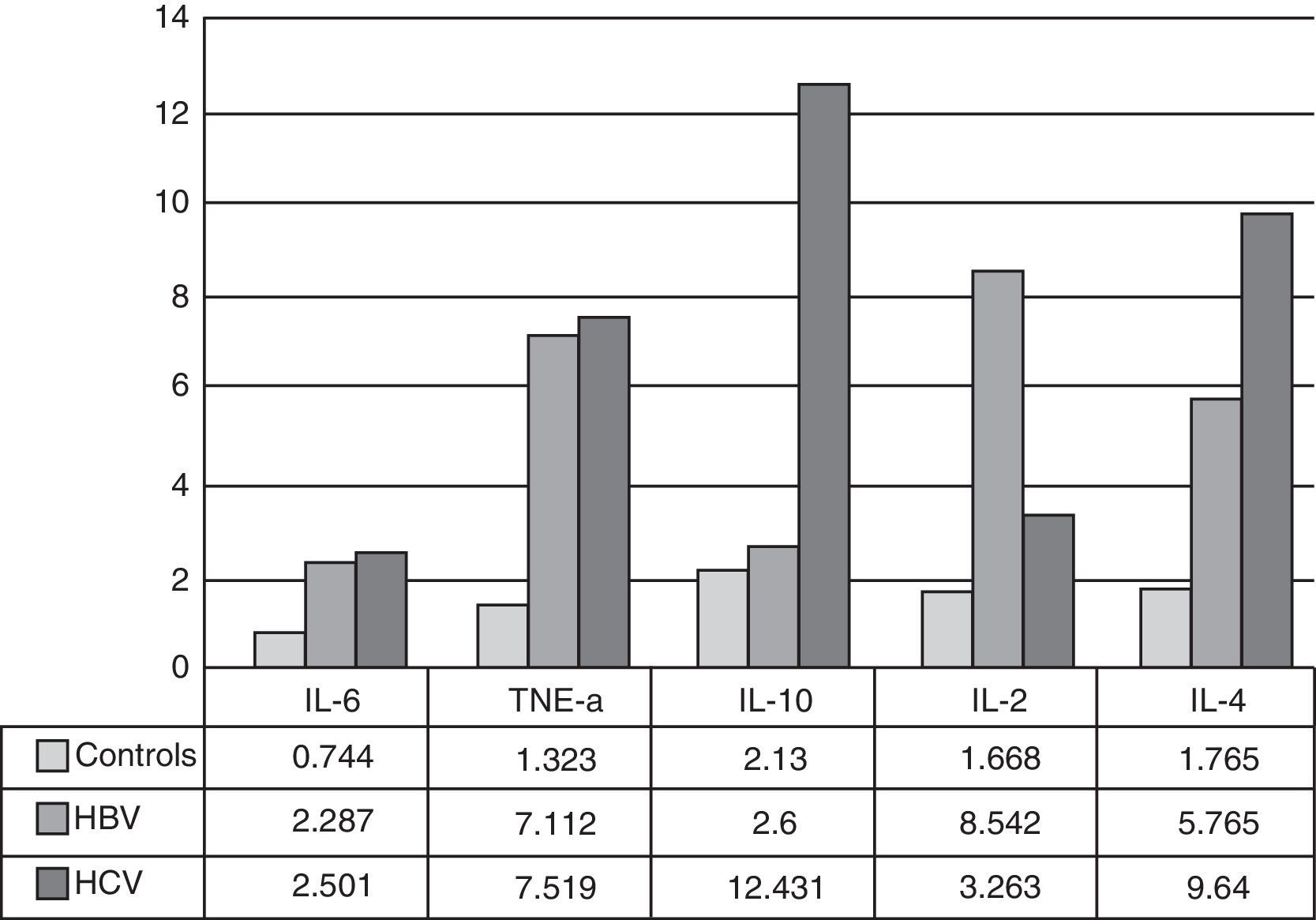
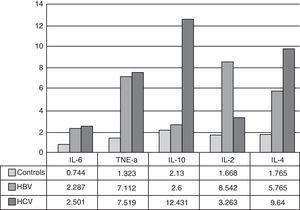
ResultsHealthy controlsIn healthy controls mean values were IL-6=0.744, TNF-α=1.323, IL-10=2.130, IL-2=1.668 and IL-4=1.765pg/mL respectively.
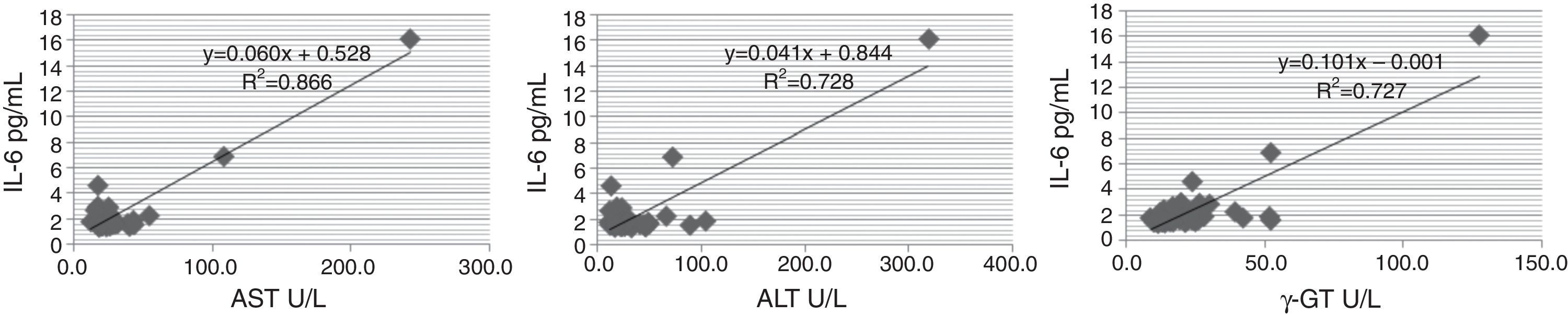
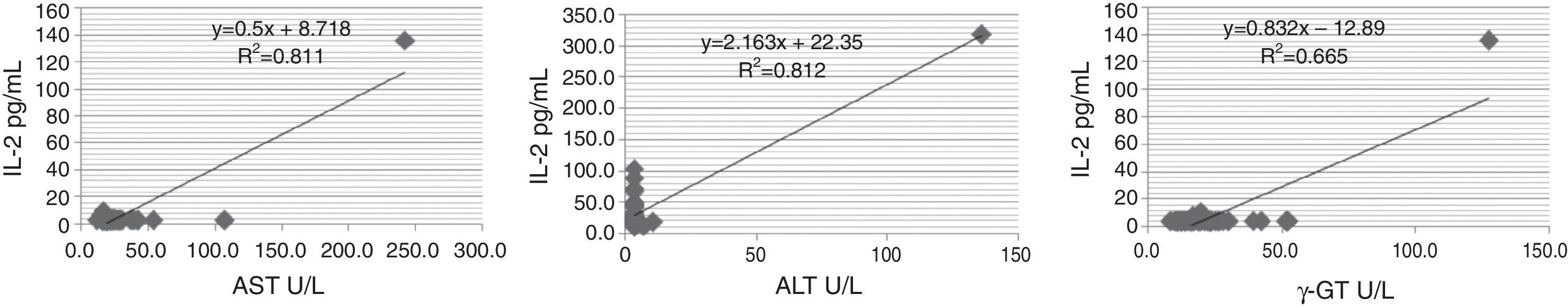
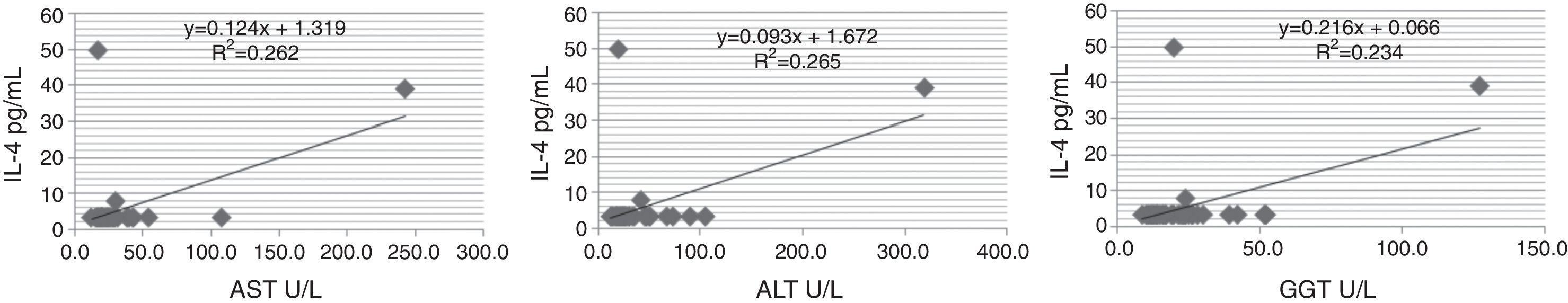
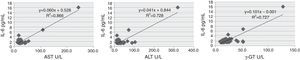
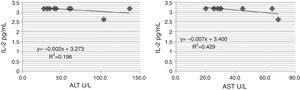
HBV patientsAST levels ranged from 11.6 to 242.4U/L (mean value 34.0), ALT levels ranged from 11.9 to 319.1U/L (mean value 41.2), ALP levels ranged from 36.4 to 116.5U/L (mean value 64.0), GGT levels ranged from 8.7 to 127.3U/L (mean value 24.9) and total bilirubin levels ranged from 0.35 to 10.77mg/dL (mean value 1.11). IL-6 levels ranged from 1.433 to 16.123pg/mL (mean 2.287). High positive correlation was observed between IL-6 levels on the one hand and AST (r=0.900), ALT (r=0.918) and GGT (r=0.853) on the other hand (Fig. 1). TNF-α levels ranged from 1.522 to 46.944pg/mL (mean 7.112). We did not observe any correlation between TNF-α levels and any of the biochemical markers. IL-10 levels were lower than 2.600pg/mL in all HBV patients. IL-2 levels ranged from 3.200 to 136.107pg/mL (mean 8.542). High positive correlation was observed between IL-2 levels on the one hand and AST (r=0.908), ALT (r=0.901) and GGT (r=0.815) on the other hand (Fig. 2). IL-4 levels ranged from 3.200 to 49.732pg/mL (mean 5.765). Positive correlation was observed between IL-4 levels and AST (r=0.512), ALT (r=0.515) and GGT (r=0.484) (Fig. 3).
Mean IL-6 and IL-4 levels were different in HBV patients than in healthy controls but these differences were not statistically significant. Statistically significant differences between HBV patients and healthy controls were observed in TNF-α and IL-2 levels (p<0.05).
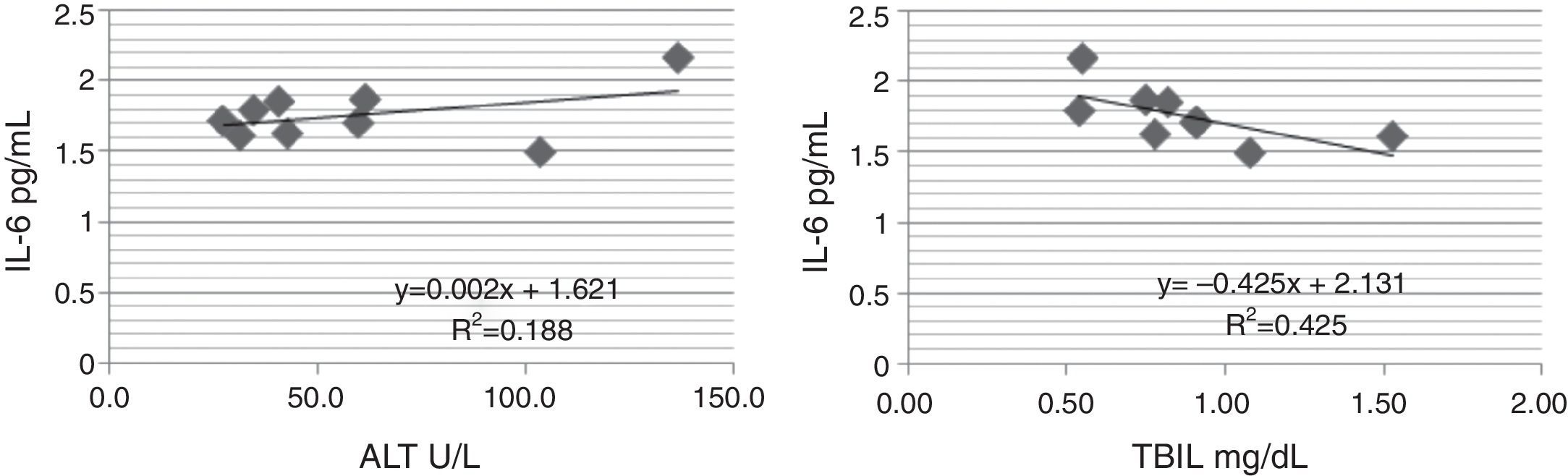
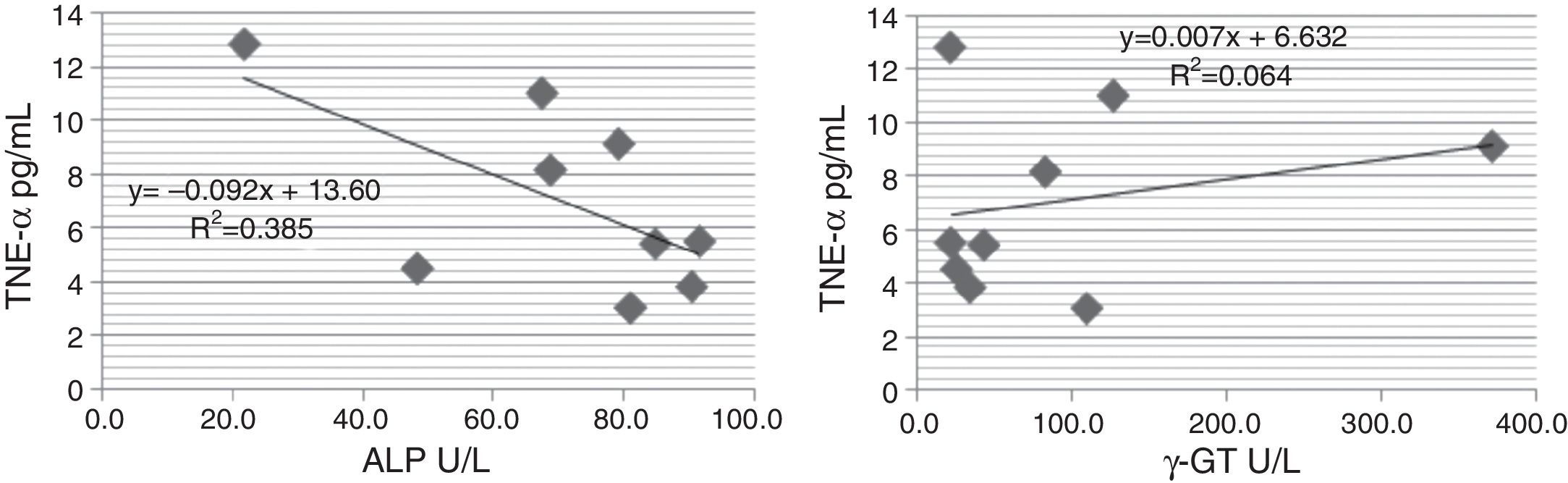
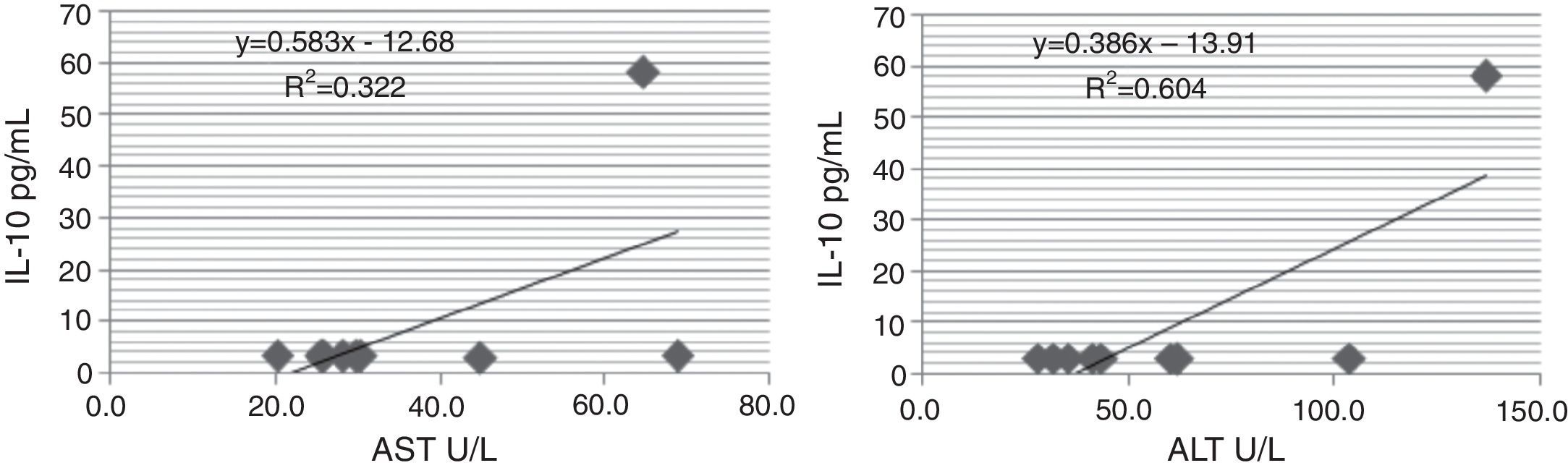
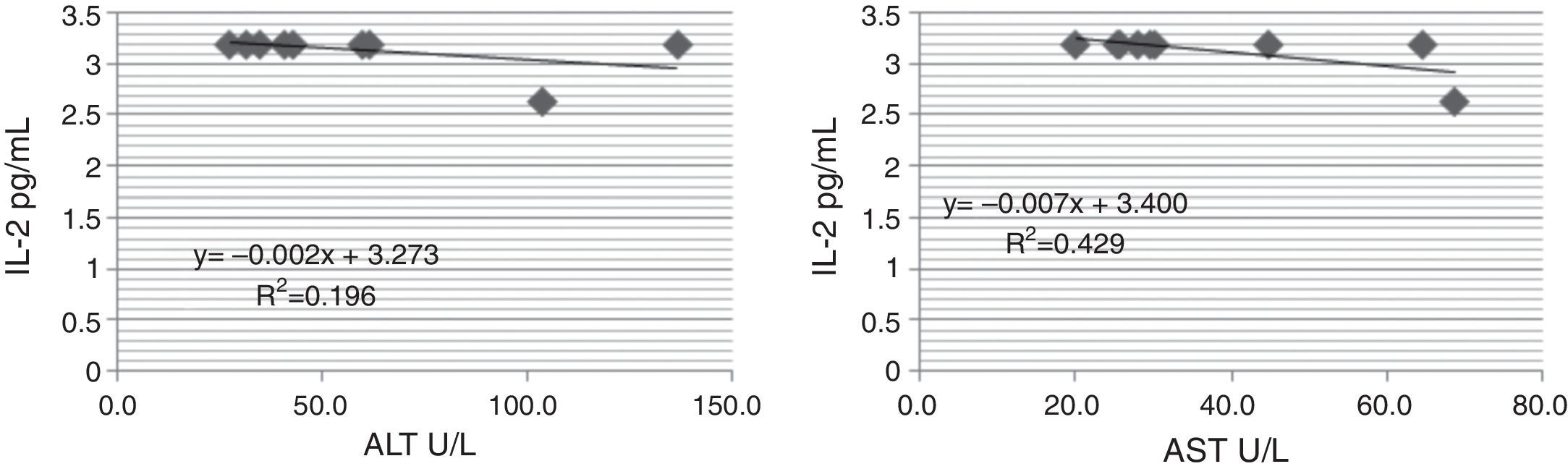
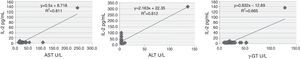
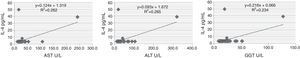
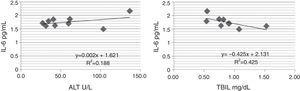
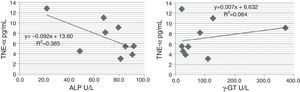
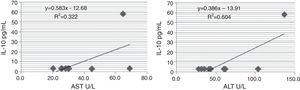
HCV patientsAST levels ranged from 20.2 to 68.8U/L (mean value 38.9), ALT levels ranged from 27.6 to 136.6U/L (mean value 64.0), ALP levels ranged from 21.7 to 91.5U/L (mean value 67.8), GGT levels ranged from 21.7 to 371.6U/L (mean value 111.9) and total bilirubin levels ranged from 0.54 to 1.53mg/dL (mean value 0.90). IL-6 levels ranged from 1.447 to 12.029pg/mL (mean 2.501). Positive correlation was observed between IL-6 levels and ALT (r=0.436), as well as between IL-6 levels and total bilirubin (r=−0.654) (Fig. 4). TNF-α levels ranged from 2.676 to 15.353pg/mL (mean 7.519). A trend of positive correlation between TNF-α levels and γ-GT (r=0.254) and a trend of negative correlation between TNF-α levels and total bilirubin levels (r=−0.250) were observed too. Significant negative correlation was also observed between TNF-α levels and ALP levels (r=−0.622 (Fig. 5). IL-10 levels ranged from 2.851 to 79.614pg/mL (mean 12.431). IL-10 levels were correlated positively with AST (r=0.565), ALT (r=0.777) and negatively with total bilirubin (r=−0.404) (Fig. 6). IL-2 levels ranged from 2.627 to 4.759pg/mL (mean 3.263). A trend of negative correlation between IL-2 levels and total bilirubin (r=−0.257) was observed. Negative correlation was also observed between IL-2 and AST (r=−0.656) and ALT (r=−0.642) (Fig. 7). IL-4 levels ranged from 3.209 to 83.705pg/mL (mean 9.640). No correlation of IL-4 levels with any of the biochemical parameters was observed.
Mean IL-6, and IL-2 levels were different in HCV patients than in healthy controls but these differences were not statistically significant. Statistically significant differences between HCV patients and healthy controls were observed in TNF-α, IL-10 and IL-4 levels (p<0.05).
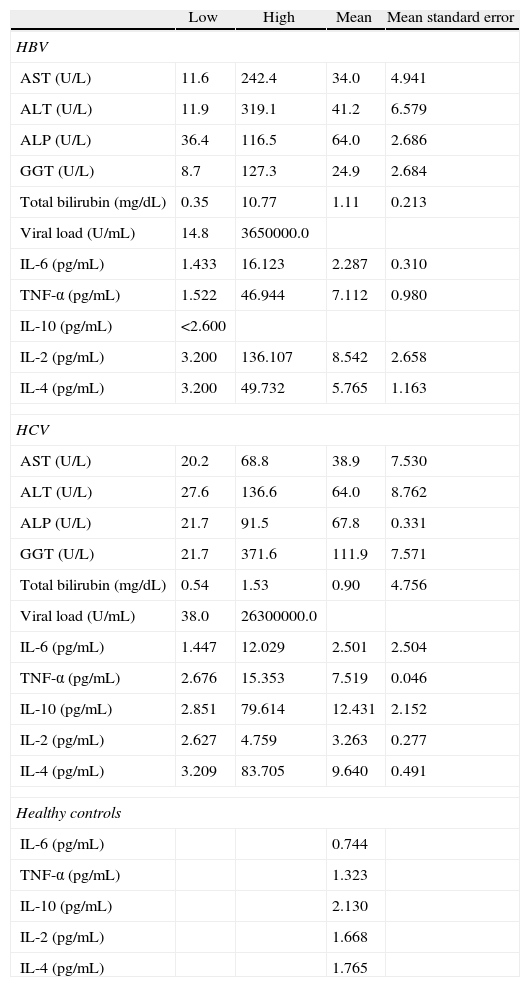
Statistically significant differences between HBV and HCV patients were observed in IL-2 and IL-10 levels (p<0.05). All study measurements are summarized in Table 1.
| Low | High | Mean | Mean standard error | |
| HBV | ||||
| AST (U/L) | 11.6 | 242.4 | 34.0 | 4.941 |
| ALT (U/L) | 11.9 | 319.1 | 41.2 | 6.579 |
| ALP (U/L) | 36.4 | 116.5 | 64.0 | 2.686 |
| GGT (U/L) | 8.7 | 127.3 | 24.9 | 2.684 |
| Total bilirubin (mg/dL) | 0.35 | 10.77 | 1.11 | 0.213 |
| Viral load (U/mL) | 14.8 | 3650000.0 | ||
| IL-6 (pg/mL) | 1.433 | 16.123 | 2.287 | 0.310 |
| TNF-α (pg/mL) | 1.522 | 46.944 | 7.112 | 0.980 |
| IL-10 (pg/mL) | <2.600 | |||
| IL-2 (pg/mL) | 3.200 | 136.107 | 8.542 | 2.658 |
| IL-4 (pg/mL) | 3.200 | 49.732 | 5.765 | 1.163 |
| HCV | ||||
| AST (U/L) | 20.2 | 68.8 | 38.9 | 7.530 |
| ALT (U/L) | 27.6 | 136.6 | 64.0 | 8.762 |
| ALP (U/L) | 21.7 | 91.5 | 67.8 | 0.331 |
| GGT (U/L) | 21.7 | 371.6 | 111.9 | 7.571 |
| Total bilirubin (mg/dL) | 0.54 | 1.53 | 0.90 | 4.756 |
| Viral load (U/mL) | 38.0 | 26300000.0 | ||
| IL-6 (pg/mL) | 1.447 | 12.029 | 2.501 | 2.504 |
| TNF-α (pg/mL) | 2.676 | 15.353 | 7.519 | 0.046 |
| IL-10 (pg/mL) | 2.851 | 79.614 | 12.431 | 2.152 |
| IL-2 (pg/mL) | 2.627 | 4.759 | 3.263 | 0.277 |
| IL-4 (pg/mL) | 3.209 | 83.705 | 9.640 | 0.491 |
| Healthy controls | ||||
| IL-6 (pg/mL) | 0.744 | |||
| TNF-α (pg/mL) | 1.323 | |||
| IL-10 (pg/mL) | 2.130 | |||
| IL-2 (pg/mL) | 1.668 | |||
| IL-4 (pg/mL) | 1.765 | |||
Chronic hepatitis B and C are characterized by inflammatory liver disease of variable severity and increased risk of developing cirrhosis, liver failure and hepatocellular carcinoma. Hepatitis B virus (HBV) and hepatitis C virus (HCV) are hepatotropic, noncytopathic viruses and liver injury induced by both viruses is mainly mediated by the host immune response against the virus infected cells and by the production of inflammatory cytokines.18 Changes in various cytokine activities that occur during the inflammatory response against these viruses are responsible for variable degree of liver damage.15,19,20 In this study we examined the serum levels of IL-6, TNF-α, IL-10, IL-2 and IL-4 in patients with chronic hepatitis B or C. Moreover, we examined correlations between serum levels of these cytokines with biochemical markers of liver disease and we compared cytokine levels between each patients type and healthy controls, as well as between HBV and HCV patients (Fig. 8).
IL-6 is a pleiotropic cytokine that exerts its complex biological activities through different mechanisms.21,22 Elevated levels of IL-6 have been associated with morbidity and disease activity in a variety of chronic diseases23,24 as well as in chronic hepatitis, liver cirrhosis and hepatocellular carcinoma.25–28 In our study IL-6 levels in HBV patients were significantly different than in healthy controls, in particular 2.287pg/mL compared to 0.787pg/mL. IL-6 levels were also significantly different in HCV patients and in particular 2.501pg/mL compared to 0.787pg/mL. However, neither the difference between HBV and HCV patients nor the difference between each type of patients and healthy controls was statistically significant. IL-6 was positively correlated with AST, ALT and GGT in HBV patients. Positive correlation of IL-6 levels with serum ALT levels in HBV patients have also been reported in other studies.11,13,29–31 In HCV patients IL-6 was positively correlated with ALT and negatively with total bilirubin. The positive correlation with transaminase levels in both patient groups is suggesting that IL-6 levels are closely related with liver inflammation status.32–34
In liver physiology TNF-α has a dual effect due to its capacity to induce both hepatocyte cell death and hepatocyte proliferation.35,36 Circulating TNF-α levels increase during HBV and HCV infection and they are associated with severity of hepatic inflammation, fibrosis, and liver injury. Moreover, they are also elevated in patients with HCC.37–41 In our study, the concentration of TNF-α in the sera of HBV and HCV patients was higher than in the control group, and this difference was statistically significant in both groups (p<0.05). There was no statistically significant difference between the two groups of patients. Serum TNF-α levels were not significantly correlated with serum ALT and AST activities neither in HBV nor in HCV infected patients. Such results have also been reported by other authors and it is concluded that measurement of TNF-α levels reflects liver injury despite normal levels of liver enzymes.20,42–46 Elevated serum TNF-α levels have been observed by other researchers even in patients with mild liver inflammation, indicating that this cytokine could be used as a predictor of liver inflammation.47
IL-10 plays an anti-inflammatory role in the immune system because it inhibits the production of proinflammatory cytokines and limits T cell activation and differentiation.48-52 Due to its immunoregulatory action, it has been assumed that inadequate levels of IL-10 can determine long-term escape of pathogens from immune control and give rise to persistent infections.53,54 In our study IL-10 levels in all HBV patients were very low. Song et al. have reported low IL-10 levels in HBV patients with no association with clinical progression of the infection.55 Our finding is in contrast to many studies which have reported elevated IL-10 levels in HBV patients.11,13,15 IL-10 levels in HCV patients were statistically different from healthy controls (p<0.05). There are contradictory reports in the literature about IL-10 levels in chronic HCV patients. Some authors have reported decreased levels of IL-10, while others have elevated levels, higher than healthy controls.13,15,48–50,56,57 In our study, IL-10 levels were positively correlated with AST and ALT levels and negatively with total bilirubin. Increase of serum AST and ALT concentrations constitutes a reliable marker of necroinflammatory activity. Therefore, we can conclude that the elevated levels of IL-10 in our HCV patients reflect the degree of necroinflammation.56,58
- •
IL-2 exerts a wide spectrum of effects on the immune system. In our study IL-2 levels in HBV patients were higher than in healthy controls and this difference was statistically significant (p<0.05). In HCV patients, IL-2 levels were different than in healthy controls, in particular 3.263pg/mL compared to 1.668pg/mL but this difference was not statistically significant. IL-2 levels were significantly different between HBV and HCV patients (p<0.05). High positive correlation was observed between IL-2 levels and AST, ALT and GGT in HBV patients, suggesting that IL-2 expression correlates with the degree of necroinflammation.11,13,59-64 In HCV patients we observed a negative correlation between IL-2 and AST (r=−0.656) and between IL-2 and ALT (r=−0.642). Our findings agree with previous studies that reported a negative correlation between ALT levels and IL-2 expression in chronic HCV patients who had persistently normal serum transaminase levels. In these patients the progression of the disease is absent or very slow.65,66
IL-4 has a suppressive effect on HBV gene expression. Thus, it plays an important and complex role in regulating the expression of viral genes and in the innate defense mechanism in liver.67–69 There are contradictory reports about IL-4 levels in chronic hepatitis patients. Some authors have reported lower levels of IL-4 in HCV patients, while others significantly elevated such levels.44,45,56,70,71 In our study the concentration of IL-4 in the sera of HBV and HCV patients was different than in the healthy controls. In particular IL-4 mean levels were 5.765pg/mL in HBV patients and 9.640pg/mL in HCV patients compared to 1.765pg/mL in healthy controls, but only in HCV patients this difference was statistically significant (p<0.05). Positive correlation was observed between IL-4 levels and AST, ALT and GGT suggesting that IL-4 expression correlates with the degree of necroinflammation. In HCV patients correlation of IL-4 levels with any of the biochemical parameters was not observed.
Our study revealed a positive significant correlation between IL-6, IL-2 and IL-4 levels on one hand and GGT levels on the other hand in HBV patients. Such a correlation in HCV patients was observed only with TNF-α. Rise of GGT levels indicates hepatocytic dysfunction or obstruction of extra-hepatic bile duct. In HCV patients we also observed such a positive correlation between TNF-α levels and ALP. In conditions affecting the liver, damaged liver cells release increased amounts of ALP into the blood, indicating liver damage. In HBV patients, correlation of total bilirubin levels with any of the cytokines was not observed. Such a correlation was observed only in HCV patients between total bilirubin on one hand and IL-6, TNF-α, IL-10 and IL-2 on the other hand. Bilirubin is a breakdown product of hemoglobin and is usually measured to screen for jaundice caused by liver or gall bladder dysfunction. To our knowledge, such correlations are reported in very few studies. As a general remark we can argue that such correlations reflect the degree of activity of the inflammatory process in the liver, as also stated by other researchers.72–74
ConclusionsCytokines play an important role in defending the host against HBV and HCV, but they have also been implicated in the hepatocellular injury seen in the majority of chronically infected patients. Persistent infection modifies the balance between different cytokine, leading to prolonged inflammation, necrosis, fibrosis and chronic liver disease. This study evaluated the serum cytokine levels (IL-6, TNF-α, IL-10, IL-2 and IL-4) of chronic hepatitis B or C patients. HBV patients showed statistically significant difference in TNF-α and IL-2 levels, versus healthy controls. HCV patients showed statistically significant difference in TNF-α, IL-10 and IL-2 levels versus healthy controls. IL10 and IL-2 levels were significantly different between HBV and HCV patients. Correlations of cytokine levels with biochemical markers of liver disease were also observed. Additional studies on a large number of patients may be required to observe the changes of cytokine activities.
Conflict of interestThe authors declare no conflict of interest.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.