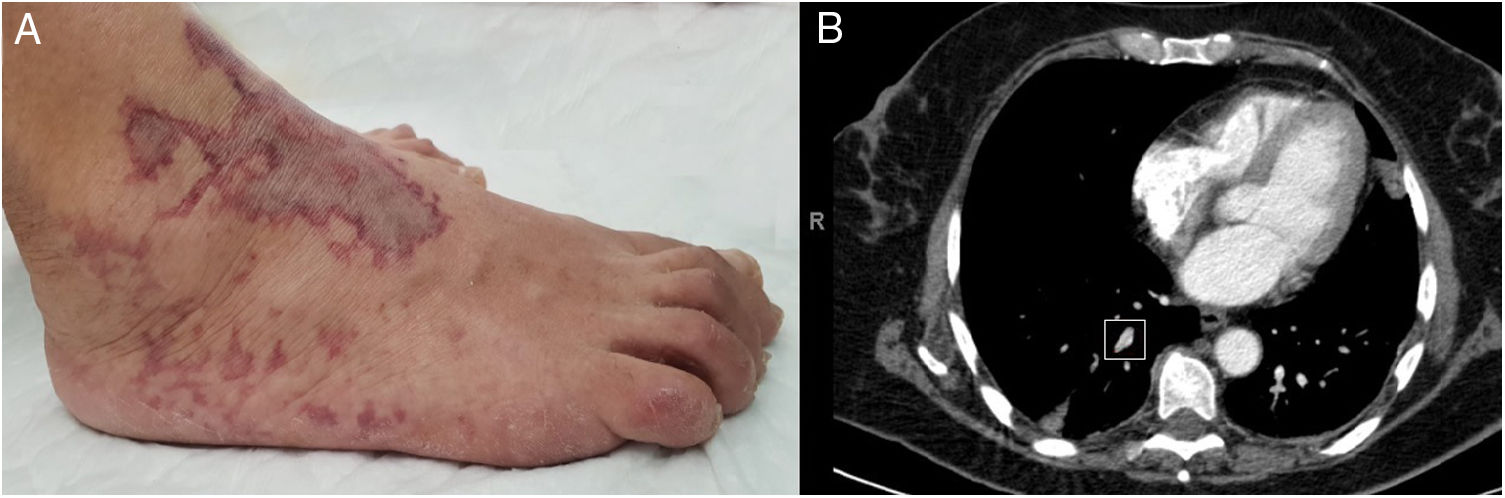
62-year-old woman, with no relevant medical history, admitted for bilateral pneumonia secondary to SARS-CoV-2 infection, who stayed 16 days in the intensive care unit (ICU) for severe respiratory failure requiring emergency orotracheal intubation due to desaturation, with subsequent gradual improvement. An inter-consultation with the dermatology department was carried out due to a 48 h-history of violaceous lesions with central areas of white atrophy and livedo-like morphology on the anterior aspect of the ankle and back of the right foot, partially painful to the touch (Fig. 1A). Two days before, the patient suffered from episodes of tachycardia and hypotension associated with a self-limited confusional state, so a transthoracic echocardiogram was performed, which was normal; a cranial CT showed no acute lesions, and a thoracic CT angiography showing an obstruction of the right apical segmental artery (Fig. 1B).
Complete blood tests were performed, with similar results to the previous ones, except elevation of d-dimers to 3571 ng/mL, serologies, urinalysis, and autoimmunity tests with antiphospholipid syndrome markers, as well as an expansion of the study of thrombotic vasculopathy with cryoglobulins and cold agglutinins, which were all negative. Two punch biopsies of the retiform lesions were also performed, showing only reticular livedo-type lesions, unfortunately without seeing the vascular thrombus due to its deep location.
Anticoagulation with enoxaparin at therapeutic doses and hydration with topical emollients was started with progressive improvement of the lesions, with subsequent discharge and follow-up in outpatient clinics.
Please cite this article as: Fulgencio-Barbarin J, Calleja-Algarra A, Morales-Raya C. Trombosis sistémica producida por COVID-19. Med Clin (Barc). 2020;155:278.