This trial was designed to investigate the effects of the interleukin (IL)-1β, IL-1Ra, IL-2, IL-6, IL-10 gene polymorphisms on Behcet's disease (BD) occurrence and the association between the polymorphisms and the phenotype.
Materials and methodThe study population consisted of 71 patients and 70 age and gender-matched healthy subjects. Each of the participants had 2cc of blood withdrawn, which was placed into a whole blood tube, and the DNA was obtained using the NucleoSpin® Blood DNA Isolation kit. To display the band lengths, the products were amplified using the primary pairs of the interleukins investigated and developed in a 2% agarose gel.
ResultsThere were no significant differences between the groups with respect to the IL-1Ra, IL-1β, IL-2, IL-6 and the IL-10 gene polymorphism distributions. In the patient group the IL-1RN2 gene polymorphism was detected to be statistically correlated with the presence of articular involvement (p=0.0283) and the IL-1β gene polymorphism was statistically correlated with the presence of an ocular lesion (p=0.0178). The evaluation of the IL-2 gene polymorphism (p=0.0065) and IL-10 gene polymorphism (p=0.0483) distributions with respect to age of BD onset revealed a statistically significant distribution.
ConclusionThe statistical correlations between the articular involvement and IL-1RN, the ocular involvement and the IL-1β, and the age of disease onset and the IL-2 and IL-10 gene polymorphisms, detected for the first time in the literature, suggest that these polymorphisms could be statistically associated with the disease symptoms and used as prognostic factors.
Este estudio fue designado para investigar los efectos de los polimorfismos genéticos de interleucina (IL)-1β, IL-1Ra, IL-2, IL-6 e IL-10 en la ocurrencia de la enfermedad de Behcet (EB) y la asociación entre los polimorfismos y el fenotipo.
Materials y métodoLa población de estudio consistió en 71 pacientes y 70 sujetos sanos emparejados por edad y sexo. A cada participante se le extrajeron 2cc de sangre y el ADN se obtuvo usando el kit NucleoSpin® Blood DNA Isolation. Para mostrar las longitudes de las bandas, los productos fueron amplificados usando los primeros pares de las IL investigadas y se desarrollaron en un gel de agarosa al 2%.
ResultadosNo hubo diferencias significativas entre los grupos en relación con las distribuciones de los polimorfismos genéticos de IL-1Ra, IL-1β, IL-2, IL-6 e IL-10. En el grupo de pacientes, el polimorfismo genético de IL-1RN2 detectado se correlacionó estadísticamente con la presencia de afección articular (p=0,0283), y el polimorfismo genético de IL-1β se correlacionó estadísticamente con la presencia de lesión ocular (p=0,0178). La evaluación de la distribución del polimorfismo genético de IL-2 (p=0,0065) e IL-10 (p=0,0483) en relación con la edad de inicio de la EB reveló una distribución estadísticamente significativa.
ConclusiónLa correlación estadística entre afección articular e IL-1RN, afección ocular e IL-1β, y la edad de inicio de la enfermedad y los polimorfismos genéticos de IL-2 e IL-10, detectados por primera vez en la literatura médica, evidencian que estos polimorfismos se asociaron estadísticamente a los síntomas de la enfermedad y se podrían usar como factores pronósticos.
Behcet's disease (BD) is a progressive disorder with a course involving exacerbations and remissions, which affects all the systems, and basically results from vasculitic inflammation. While the worldwide prevalence ranges between 0.07 and 42/10,000, it is most commonly observed in Turkey.1 The geographic distribution of BD reveals the contribution of the genetic factors to the pathogenesis.2 The etiology is not clearly understood; however, the occurrence of the disease has been attributed to several causes, including infectious agents, vascular endothelial pathologies, immunologic and environmental factors, hormones and clotting factors.3,4 Cytokine-producing cells were reported to be involved in the disease immunopathogenesis, and the cytokines were reported to be significantly involved in the occurrence and course of the disease.5,6 The studies on etiopathogenesis reported results, establishing an association between the cytokine genes such as IL-l A and β, IL-8, IL-12, IL-10, the gene polymorphisms, which are significantly involved in the gene polymorphisms, and BD.7–9 However, the literature data on the correlations between the gene polymorphisms and the disease progression and the phenotype is very limited.
In our trial, based on the fact that BD is a chronic inflammatory disease, we assessed the association between the primary mediators of inflammation, the interleukin-1 beta (IL-1β) from the interleukin-1 cytokine family, the interleukin-1 receptor antagonist (IL-1Ra), a physiological antagonist of the IL-1β, the interleukin 2 (IL-2), functioning as the control center in the inflammatory pathway, the pro-inflammatory IL-6 and anti-inflammatory IL-10 gene polymorphisms, and BD. In addition, considering that the effects of polymorphisms on the disease symptoms, such as ocular lesion, erythema nodosum, and the age of onset were being evaluated for the first time, we aimed at providing a further contribution to the literature and a new point of view for the treatment and follow-up of patients.
Materials and methodSeventy-one patients, including 36 females and 35 males, who were diagnosed with BD based on the International Behcet's disease Study Group diagnostic criteria,10 were included in the trial. At enrollment into the trial, the presence or absence of active or inactive major aphthae, genital ulcer, superficial venous thrombosis, erythema nodosum, uveitis, progressive central nervous system (CNS) lesions, progressive vasculitis, arthritis and BD-associated epididymitis findings was not taken into consideration. Only the establishment of the diagnosis based on the study group criteria was considered adequate. The control group consisted of age- and gender-matched healthy individuals (35 females and 35 males) with no chronic renal failure, coronary artery disease, vasculitic lesions, diabetes mellitus, hypertension, liver parenchymal disease, acute infections or chronic inflammatory disease. Consent was obtained from the Ethics Committee to conduct the trial.
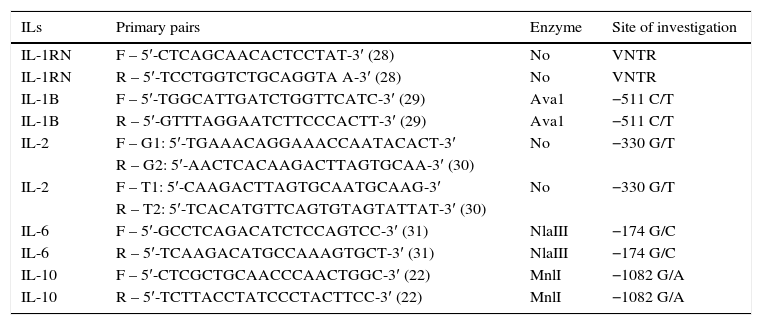
Genetic methodTwo cc's of blood was withdrawn from all the participants into a whole blood tube and the DNA was obtained, using the NucleoSpin® Blood DNA Isolation kit. The products, amplified using the primary pairs, presented in the table below, were developed in a 2% agarose gel to display the band lengths11 (Table 1).
The primary pairs used for the amplification of the investigated interleukins.
| ILs | Primary pairs | Enzyme | Site of investigation |
|---|---|---|---|
| IL-1RN | F – 5′-CTCAGCAACACTCCTAT-3′ (28) | No | VNTR |
| IL-1RN | R – 5′-TCCTGGTCTGCAGGTA A-3′ (28) | No | VNTR |
| IL-1В | F – 5′-TGGCATTGATCTGGTTCATC-3′ (29) | Ava1 | −511 C/T |
| IL-1В | R – 5′-GTTTAGGAATCTTCCCACTT-3′ (29) | Ava1 | −511 C/T |
| IL-2 | F – G1: 5′-TGAAACAGGAAACCAATACACT-3′ | No | −330 G/T |
| R – G2: 5′-AACTCACAAGACTTAGTGCAA-3′ (30) | |||
| IL-2 | F – T1: 5′-CAAGACTTAGTGCAATGCAAG-3′ | No | −330 G/T |
| R – T2: 5′-TCACATGTTCAGTGTAGTATTAT-3′ (30) | |||
| IL-6 | F – 5′-GCCTCAGACATCTCCAGTCC-3′ (31) | NlaIII | −174 G/C |
| IL-6 | R – 5′-TCAAGACATGCCAAAGTGCT-3′ (31) | NlaIII | −174 G/C |
| IL-10 | F – 5′-CTCGCTGCAACCCAACTGGC-3′ (22) | MnlI | −1082 G/A |
| IL-10 | R – 5′-TCTTACCTATCCCTACTTCC-3′ (22) | MnlI | −1082 G/A |
The collected data was assessed using SPSS for Windows 12.0 and EPI INFO 6. The ages were expressed as mean±standard deviation. The chi-square or chi-square Fisher's exact tests were used for inter-group comparison. In case there was an observed value<25 in the 2×2 tables, the Yates continuity correction was performed and if any cell was a ‘0′ value, no analysis was performed. OR and 95% confidence interval of OR were calculated under the assumption of all other variables (e.g., gender, age, BMI, etc.) were fixed. p<0.05 was considered to indicate a statistically significant difference.
ResultsCharacteristics of the patient groupThe BD group consisted of 35 males (49.3%) and 36 females (50.7%), between 16 and 61 years of age (mean age: 37.8±1.0). All patients had oral aphthae and genital ulcers. The pathergy test result was positive in 66 of the cases, and 47 patients had articular involvement. Other clinical characteristics of patient group listed in Table 2.
Demographic and clinical characteristics of patient group.
| Clinical characteristics | Male | Female | Total | |||
|---|---|---|---|---|---|---|
| Positive n (%) | Negative n (%) | Positive n (%) | Negative n (%) | Positive n (%) | Negative n (%) | |
| Oral aphta | 35 (100.0) | 0 (0.0) | 36 (100.0) | 0 (0.0) | 71 (100.0) | 0 (0.0) |
| Genital ulcer | 35 (100.0) | 0 (0.0) | 36 (100.0) | 0 (0.0) | 71 (100.0) | 0 (0.0) |
| Pathery test results | 34 (97.1) | 1 (2.9) | 32 (88.9) | 4 (11.1) | 66 (93.0) | 5 (7.0) |
| Articular involvement | 22 (63.0) | 13 (37.0) | 25 (69.4) | 11 (30.6) | 47 (66.2) | 24 (33.8) |
| Lesions | ||||||
| Ocular | 12 (34.3) | 23 (65.7) | 25 (69.4) | 11 (30.6) | 37 (52.1) | 34 (47.9) |
| Erythema nodosum | 12 (34.3) | 23 (65.7) | 13 (36.1) | 23 (63.9) | 25 (35.2) | 46 (64.8) |
| Acneiform eruption | 7 (20.0) | 28 (80.0) | 10 (27.8) | 26 (72.2) | 17 (23.9) | 54 (76.1) |
| GIS involvementa | 9 (25.7) | 26 (74.3) | 4 (11.1) | 32 (88.9) | 13 (18.3) | 58 (81.7) |
| CNS involvementb | 5 (14.3) | 30 (85.7) | 7 (19.4) | 29 (80.6) | 12 (16.9) | 59 (83.1) |
| CVS involvementc | 2 (5.7) | 33 (94.3) | 3 (8.3) | 33 (91.7) | 5 (7.0) | 66 (93.0) |
The ratio of allele polymorphisms did not vary significantly between the groups. The patient group showed less polymorphism in the IL-1 RN2 allele than the control group (χ2=4.082; p=0.043) (Table 3).
Comparison of polymorphic allele distribution.
| Allele | Patient (n=142) | Control (n=140) | Test statistics | |||||
|---|---|---|---|---|---|---|---|---|
| Present n (%) | Absent n (%) | Present n (%) | Absent n (%) | χ2 | P | OR | 95% CI for OR | |
| IL-1 RN | ||||||||
| IL-1 RN1 | 119 (83.8) | 23 (16.2) | 109 (77.9) | 31 (22.1) | 1.610 | 0.205 | 1.47 | 0.81–2.68 |
| IL-1 RN2 | 16 (11.3) | 126 (88.7) | 28 (20.0) | 112 (80.0) | 4.082 | 0.043 | 0.51 | 0.26–0.99 |
| IL-1 RN3 | 5 (3.5) | 137 (96.5) | 1 (0.7) | 139 (99.3) | a | 0.088 | 5.07 | 0.59–43.99 |
| IL-1 RN4 | 2 (1.4) | 140 (98.6) | 1 (0.7) | 139 (99.3) | a | 1.000 | 1.99 | 0.18–22.15 |
| IL-1β | ||||||||
| IL-1β T/IL-1β C | 69 (48.6) | 73 (51.4) | 78 (55.7) | 62 (44.3) | 1.433 | 0.231 | 0.75 | 0.47–1.20 |
| IL-2 | ||||||||
| IL-2 T/IL-2 G | 79 (55.6) | 63 (44.4) | 70 (50.0) | 70 (50.0) | 0.898 | 0.343 | 1.25 | 0.79–2.00 |
| IL-6 | ||||||||
| IL-6 G/IL-6 C | 65 (45.8) | 77 (54.2) | 71 (50.7) | 69 (49.3) | 0.689 | 0.407 | 0.82 | 0.51–1.31 |
| IL-10 | ||||||||
| IL-10 A/IL-10 G | 98 (69.0) | 44 (31.0) | 99 (70.7) | 41 (29.3) | 0.097 | 0.756 | 0.92 | 0.55–1.53 |
In the patient group, individuals with ocular involvement had a statistically significantly higher IL-1β T/IL-1β C ratio than individuals without ocular involvement (χ2=5.615; p=0.018). Patients with ocular involvement had OR=2.35 times higher risk of having IL-1β T/IL-1β C than patients without ocular involvement. The presence or absence of ocular involvement did not have a significant effect on other allele polymorphisms.
In the patient group, individuals with an age of onset >24 had a higher ratio of IL-2 T/IL-2 G (χ2=8.461; p=0.004, OR: 3.25) and IL-10 A/IL-10 G (χ2=4.736; p=0.030, OR: 2.68), than individuals with an age of onset <24. The age of onset did not have a significant effect on other allele polymorphisms.
The presence or absence of erythema nodosum did not have a significant effect on allele polymorphisms.
In the patient group, individuals with articular involvement had a higher ratio of IL-1 RN2 (p=0.013, OR: 8.93) IL-1 RN3 (p=0.004) than individuals without articular involvement. Articular involvement did not have a significant effect on the other allele polymorphisms (Table 4).
Comparison of polymorphic allele distribution in patient group for additional findings.
| Allele | Polymorphic allele | Test statistics | ||||||
|---|---|---|---|---|---|---|---|---|
| Present n (%) | Absent n (%) | Present n (%) | Absent n (%) | χ2 | p | OR | 95% CI for OR | |
| Ocular involvement (+) (n=48) | Ocular involvement (–) (n=94) | |||||||
| IL-1 RN1 | 44 (91.7) | 4 (8.3) | 76 (80.9) | 18 (19.1) | 2.967 | 0.085 | 2.65 | 0.85–8.27 |
| IL-1 RN2 | 3 (6.3) | 45 (93.8) | 13 (13.8) | 81 (86.2) | 1.826 | 0.177 | 0.42 | 0.11–1.54 |
| IL-1 RN3 | 1 (2.1) | 47 (97.9) | 4 (4.3) | 90 (95.7) | a | 0.663 | 0.48 | 0.05–4.41 |
| IL-1 RN4 | 0 (0.0) | 48 (100.0) | 2 (2.1) | 92 (97.9) | a | 0.549 | N/A | N/A |
| IL-1β T/IL-1β C | 30 (62.5) | 18 (37.5) | 39 (41.5) | 55 (58.5) | 5.615 | 0.018 | 2.35 | 1.15–4.80 |
| IL-2 T/IL-2 G | 27 (56.3) | 21 (43.8) | 52 (55.3) | 42 (44.7) | 0.011 | 0.916 | 1.04 | 0.52–2.09 |
| IL-6 G/IL-6 C | 24 (50.0) | 24 (50.0) | 53 (56.4) | 41 (443.6) | 0.522 | 0.470 | 0.77 | 0.39–1.55 |
| IL-10 A/IL-10 G | 34 (70.8) | 14 (29.2) | 64 (68.1) | 30 (31.9) | 0.112 | 0.738 | 1.14 | 0.53–2.43 |
| Age of onset (<24) (n=40) | Age of onset (>24) (n=102) | |||||||
| IL-1 RN1 | 35 (87.5) | 5 (12.5) | 84 (82.4) | 18 (17.6) | 0.561 | 0.454 | 1.50 | 0.52–4.36 |
| IL-1 RN2 | 3 (7.5) | 37 (92.5) | 13 (12.7) | 89 (87.3) | 0.791 | 0.374 | 0.56 | 0.15–2.06 |
| IL-1 RN3 | 1 (2.5) | 39 (97.5) | 4 (3.9) | 98 (96.1) | 0.171 | 0.679 | 0.63 | 0.07–5.80 |
| IL-1 RN4 | 1 (2.5) | 39 (97.5) | 1 (1.0) | 101 (99.0) | a | 0.485 | 2.59 | 0.16–42.43 |
| IL-1β T/IL-1β C | 16 (40.0) | 24 (60.0) | 53 (52.0) | 49 (48.0) | 1.645 | 0.200 | 0.62 | 0.29–1.30 |
| IL-2 T/IL-2 G | 30 (75.0) | 10 (25.0) | 49 (48.0) | 53 (52.0) | 8.461 | 0.004 | 3.25 | 1.44–7.33 |
| IL-6 G/IL-6 C | 22 (55.0) | 18 (45.0) | 43 (42.2) | 59 (57.8) | 1.909 | 0.167 | 1.68 | 0.80–3.50 |
| IL-10 A/IL-10 G | 33 (82.5) | 7 (17.5) | 65 (63.7) | 37 (36.3) | 4.736 | 0.030 | 2.68 | 1.08–6.67 |
| Erythema nodosum (+) (n=50) | Erythema nodosum (–) (n=92) | |||||||
| IL-1 RN1 | 46 (92.0) | 4 (8.0) | 73 (79.3) | 19 (20.7) | 3.820 | 0.051 | 2.99 | 0.96–9.36 |
| IL-1 RN2 | 4 (8.0) | 46 (92.0) | 12 (13.0) | 80 (87.0) | 0.824 | 0.364 | 0.58 | 0.18–1.90 |
| IL-1 RN3 | 0 (0.0) | 52 (100.0) | 5 (5.4) | 87 (94.6) | a | 0.159 | N/A | N/A |
| IL-1 RN4 | 0 (0.0) | 52 (100.0) | 2 (2.2) | 90 (97.8) | a | 0.535 | N/A | N/A |
| IL-1β T/IL-1β C | 25 (50.0) | 25 (50.0) | 44 (47.8) | 48 (52.2) | 0.061 | 0.804 | 1.09 | 0.55–2.17 |
| IL-2 T/IL-2 G | 30 (60.0) | 20 (40.0) | 49 (53.3) | 43 (46.7) | 0.596 | 0.440 | 1.32 | 0.66–2.65 |
| IL-6 G/IL-6 C | 25 (50.0) | 25 (50.0) | 40 (43.5) | 50 (56.5) | 0.555 | 0.456 | 1.30 | 0.65–2.59 |
| IL-10 A/IL-10 G | 34 (68.0) | 15 (32.0) | 64 (69.6) | 28 (30.4) | 0.037 | 0.847 | 0.93 | 0.44–1.95 |
| Articular involvement (+) (n=94) | Articular involvement (–) (n=48) | |||||||
| IL-1 RN1 | 79 (84.0) | 15 (16.0) | 40 (83.3) | 8 (16.7) | 0.012 | 0.914 | 1.05 | 0.41–2.69 |
| IL-1 RN2 | 15 (16.0) | 79 (84.0) | 1 (2.1) | 47 (97.9) | 6.118 | 0.013 | 8.92 | 1.14–69.75 |
| IL-1 RN3 | 0 (0.0) | 94 (100.0) | 5 (10.4) | 43 (89.6) | a | 0.004 | N/A | N/A |
| IL-1 RN4 | 0 (0.0) | 94 (100.0) | 2 (4.2) | 46 (95.8) | a | 0.113 | N/A | N/A |
| IL-1β T/IL-1β C | 45 (47.9) | 49 (52.1) | 24 (50.0) | 24 (50.0) | 0.058 | 0.810 | 0.92 | 0.46–1.84 |
| IL-2 T/IL-2 G | 51 (54.3) | 43 (45.7) | 28 (58.3) | 20 (41.7) | 0.214 | 0.644 | 0.85 | 0.42–1.71 |
| IL-6 G/IL-6 C | 39 (41.5) | 55 (58.5) | 26 (54.2) | 22 (45.8) | 2.057 | 0.151 | 0.60 | 0.30–1.21 |
| IL-10 A/IL-10 G | 65 (69.1) | 29 (30.9) | 33 (68.8) | 15 (31.3) | 0.002 | 0.961 | 1.02 | 0.48–2.16 |
N/A, not available.
The results of this trial show that, while the polymorphism distributions in the IL-1β, IL-2, IL-6, IL-1Ra and IL-10 genes of the Behcet patients do not exhibit a difference relative to the control group, there are certain effects on the clinical involvement and the age of disease onset. The previous trials have investigated the association of these gene polymorphisms with BD and revealed controversial results.5–9,12 However, the literature includes a very limited data on the correlations between these gene polymorphisms and the clinical involvements and the age of onset of the disease. In our trial, we detected the differences in the IL-1RN2 allele, IL-1β gene polymorphism distribution, and the IL-1 and IL-10 gene polymorphism distributions in patients with articular involvement, ocular involvement, and the age of disease onset, respectively.
BD is a progressive disease with a course of remissions and exacerbations, which affects all the systems including articular, pulmonary, gastrointestinal, cardiac, vascular and neurologic involvements. It usually has an onset between the age of 30 and 40 years.3–5 The incidence of the disease among males and females is equal, considering the overall population, even if it varies between the countries.13 The mean age was 37.8±1.0 in our trial and the female to male ratio was 1.01. While all the patients had an oral aphthae and genital ulcers, 66%, 33.8%, 18.3%, 16.9% and 7% of the patients had articular involvement, ocular involvement, GIS involvement, CNS involvement and CVS involvement, respectively. These are similar to those reported in the literature.
Due to the increased inflammation occurring in BD the polymorphisms, or the mutations of the genes involved in the mechanism of inflammation, are considered to be potentially effective in the development of the disease. The studies on etiopathogenesis reported results, establishing an association between several cytokine genes and the gene polymorphisms significantly involved in the immune response, and the BD; and a hypothesis was developed that these could have an important role in the onset and course of the disease.5–9,12 We did not detect a correlation between the IL-1β gene polymorphism and the presence of BD in our trial. This result suggests that the gene polymorphism, indicated in the inflammation occurring in BH, is not involved in the vasculitic inflammation that occurs during the disease. Similar to the trials reported in the literature, no difference was demonstrated in the IL-2 and IL-6 gene polymorphism between the BD and control groups, and this result suggested that it had no effect on the BD occurrence or clinical involvements.14,15
In our trial, we investigated the association between the IL-10 gene polymorphism and detected no statistically significant differences between the groups. In a trial by Wallace et al. in different ethnical groups, similar results were obtained.4 While a study by Dilek et al. reported that the IL-10 gene polymorphism could increase the host sensitivity for BD, another trial detected no difference between the patients and the controls, similar to our trial.16,27 Another noticeable point in our trial was that among cases of BD, 21 of the 26 patients with IL-6 GG polymorphism that possessed a high proinflammatory activity also had IL-10 GG polymorphism, a type of polymorphism with a lower anti-inflammatory efficacy. Future studies may investigate this haplotype in larger series, thereby establishing a more scientific basis for this clinical course that is in favor of inflammation.
The studies on the association between ocular involvement and gene polymorphism are very limited. In trial by Aydın et al., 45 of the 80 patients investigated were detected to have an eye lesion and no significant association with the IL-1β gene polymorphism could be demonstrated in these patients.14 A trial by Kotter et al. detected that the serum IL1Ra levels increased following treatment with an anti-inflammatory agent in BD patients with ocular involvement.17 While we failed to observe a correlation between the IL-2 gene polymorphism and the ocular involvement, the results were found to be statistically significant when the IL-1β gene polymorphism was assessed for ocular involvement.
There was a significant correlation between the IL-2 and IL-10 gene polymorphisms and the age of disease onset in our trial. This was considered to result from the high level of the IL-2 T allele, which was more effective in inflammation, and the failure of the IL-10 G polymorphism to prevent inflammation; and the potential involvement of this in the occurrence of the disease relatively at a smaller age was thus considered. We could not find any studies in the literature that supported or contradicted our finding. This parameter needs to be investigated in larger patient series to support this finding.
Considering the articular involvement, the patients with articular involvement were observed to show a difference in the IL-1RN2 allele. This resulted in the implication that the more potent IL-1RN2 allele did not prevent the articular involvement. In literature studies on patients with lupus erythematosus, rheumatoid arthritis and chronic inflammatory rheumatoid disease with articular involvement, IL-1RN2 gene was reported to be statistically significant.18–21 While we failed to find an article investigating the relevant gene polymorphism and the articular involvement in BH in the literature, the IL-1 RN2 gene polymorphisms could be involved in the occurrence of articular involvement in BD, given the other diseases with articular involvement.
In conclusion, we attempted to demonstrate the impact of certain cytokine gene polymorphisms on the occurrence of BD, and also the association of the polymorphisms and the phenotype. Based on our findings, the allele distribution of these polymorphisms between the patients and controls is not statistically significant. Thus, while we can conclude that these polymorphisms are not associated with BD, there's still a need for a more extensive trial, which would investigate the cytokine haplotypes that increase the inflammation tendency, and those that prevent the occurrence of inflammation. The statistically significant correlations between the articular involvement and IL-1RN, the ocular involvement and the IL-1β, and the age of disease onset and the IL-2 and IL-10 gene polymorphisms suggest that these polymorphisms could be associated with the disease symptoms. Given the incidence of the polymorphisms, studies involving larger numbers of patients and controls are required to reach a clear conclusion.
Study limitationsThe patients included in the study were a small group of individuals visiting the internal medicine outpatient clinic, which makes it difficult to extend the present findings to the general population. The study's sample size was adequate to provide sufficient statistical power. Our findings need to be confirmed and validated in much larger studies, using appropriate reclassification statistics, to provide value to existing risk scores.
Conflict of interestsThe authors declare no conflict of interest.