The COVID-19 pandemic significantly increased the global burden of respiratory morbidity and mortality. In Spain, 2020 saw a 68.5% surge in deaths from respiratory diseases compared to 2019, largely due to COVID-19. This study aims to describe respiratory disease mortality in Spain from 2019 to 2022, focusing on the intersection of COVID-19, pre-existing respiratory conditions, and specific health determinants.
Materials and methodsWe analyzed mortality data from the Spanish National Institute of Statistics (INE), covering 102 causes of death, including tuberculosis, COVID-19, and lung cancer as respiratory-related conditions. The analysis considered absolute death counts and proportions by sex, age, and region, along with percentage changes in proportional mortality. Logistic regression models were used to identify factors potentially associated with COVID-19 and respiratory-specific mortality.
ResultsIn 2022, Spain reported 98,128 deaths from respiratory diseases, accounting for 21.1% of all deaths and ranking as the second leading cause of death after cardiovascular diseases. Although deaths due to COVID-19 decreased in 2021 and 2022, there was a notable rise in other respiratory causes, indicating a lasting post-pandemic impact. Factors linked to higher mortality included male gender, older age, being divorced, and residing in urban areas, with significant regional variability.
ConclusionsDespite overall mortality returning to pre-pandemic levels, this study highlights a significant increase in respiratory disease deaths in Spain in 2022 compared to 2019.
La pandemia de COVID-19 resaltó la gran carga de morbilidad y mortalidad respiratoria a nivel global. En 2020, España experimentó un aumento del 68,5% en las muertes por enfermedades respiratorias, principalmente asociadas a COVID-19, en comparación con 2019. Este estudio describe la mortalidad relacionada con enfermedades respiratorias en España desde 2019 hasta 2022, con un enfoque en la superposición entre COVID-19, condiciones respiratorias preexistentes y determinantes de salud.
Materiales y métodosSe utilizaron datos de mortalidad del Instituto Nacional de Estadística (INE) de España que cubren 102 causas de muerte, incluyendo tuberculosis, COVID-19 y cáncer de pulmón. El análisis abarcó conteos absolutos de muertes, proporciones por sexo, edad y regiones, así como el cambio porcentual en la mortalidad proporcional. Se emplearon modelos de regresión logística para identificar variables asociadas con la mortalidad por COVID-19 y enfermedades respiratorias.
ResultadosEn 2022, España registró 98,128 muertes atribuidas a enfermedades respiratorias, representando el 21,1% de todas las muertes, siendo la segunda causa principal de muerte después de las enfermedades cardiovasculares. Aunque las muertes por COVID-19 disminuyeron en 2021 y 2022, hubo un aumento en otras causas respiratorias, indicando un impacto persistente pospandemia. Se identificaron varios factores asociados con la mortalidad por enfermedades respiratorias, como el sexo masculino, la edad avanzada, el estado civil de divorciado y vivir en áreas urbanas, aunque con variabilidad regional.
ConclusionesAunque la mortalidad general volvió a los niveles previos a la pandemia, el estudio muestra un aumento significativo en las muertes por enfermedades respiratorias en España en 2022 en comparación con 2019.
Respiratory diseases are a major burden on global health, affecting all populations worldwide,1 so healthy lungs are integral to overall health.2 With the onset of the COVID-19 pandemic, already in the fifth year,3 increased attention has been focused on understanding and addressing the global burden of respiratory morbidity and mortality, targeting attention from other diseases that also have a considerable impact on society.4
In Spain, as in many other countries, the year 2020 was characterised by an unprecedented public health crisis that resulted in a 68.5% increase in deaths related to respiratory diseases, mostly attributed to COVID-195 compared to 2019. These excess deaths not only resulted in an overall decrease in life expectancy from 79.20 to 77.45 years,6,7 but also raised concerns about the persistence of this increase in the medium and long term, considering the complexity of the factors involved.8 However, the scope of respiratory diseases goes beyond the sphere of the COVID-19 pandemic. Previous reports, such as the reports by Heppe-Montero et al.,9 suggest that respiratory infections, such as those caused by the respiratory syncytial virus (RSV), influenza, among others, play a major role in driving population morbidity and mortality, especially in the elderly population. Furthermore, non-communicable diseases (NCDs) including respiratory diseases like COPD, have ranked among the leading causes of death in Spain,10 represent converging factors that demand attention in any comprehensive assessment of the burden of disease.
This study aims to evaluate respiratory-related mortality including tuberculosis, COVID-19 and lung cancer in Spain, focusing on the evolution between 2019 and 2022, and exploring if the percentage of respiratory-related deaths returned to pre-pandemic levels. Throughout these years, we will study the direct impact of COVID-19 in respiratory-related mortality, and possible changes in other respiratory causes of death. Further, we will examine variables associated higher mortality proportions.
Material and methodsThe study followed the STROBE guidance for observational research.11 Mortality data of residents in Spain between the years 2019 and 2022 were obtained from the National Institute of Statistics (INE), namely with the Short List of 102 causes of death based on ICD-10.12 A review and regrouping of causes was conducted expanding the category of “diseases of the respiratory system” (ICD J00-J99), with other respiratory diseases such as tuberculosis (ICD A15-A19, B90) and malignant tumours of the trachea, bronchi, and lung (ICD C33, C34). Further, the causes “COVID-19 virus identified” (ICD U07.1), “COVID-19 virus not identified (suspected)” (ICD U07.2) and “COVID-19 associated multisystemic inflammatory syndrome COVID-19” (ICD U10.9) were also included. Additional attention was given to specific respiratory causes of death, such as asthma, respiratory insufficiency, and other respiratory system diseases.
The analysis spanned four years from January 2019 to December 2022, with 2019, the year preceding the onset of COVID-19, serving as a reference year.
Mortality was described as absolute frequencies of deaths per year and proportional mortality by year, sex, age groups, and autonomous regions. We computed the percentage change in proportional mortality (share out of all-causes deaths) between the pre-pandemic year 2019 and the pandemic years 2020, 2021 and 2022 and compared each using Chi-square test or Fisher's exact test, whenever necessary (less than 5 expected observations), with statistical significance set at p<0.01. To discern variables associated with mortality, we used a logistic regression model using death counts for mortality attributed to COVID-19 (model 1) and for mortality attributed to respiratory cause (model 2) with available variables namely year, sex, autonomous regions, age range, municipal residence size, country aggregations, place of decease and marital status. The estimation of odds ratios (ORs) for both crude and multivariate, along with their corresponding 95% confidence intervals (CIs), was conducted with a threshold of p<0.01 to determine statistical significance. All data management and analyses were programmed using RStudio 2023.12.1+402.
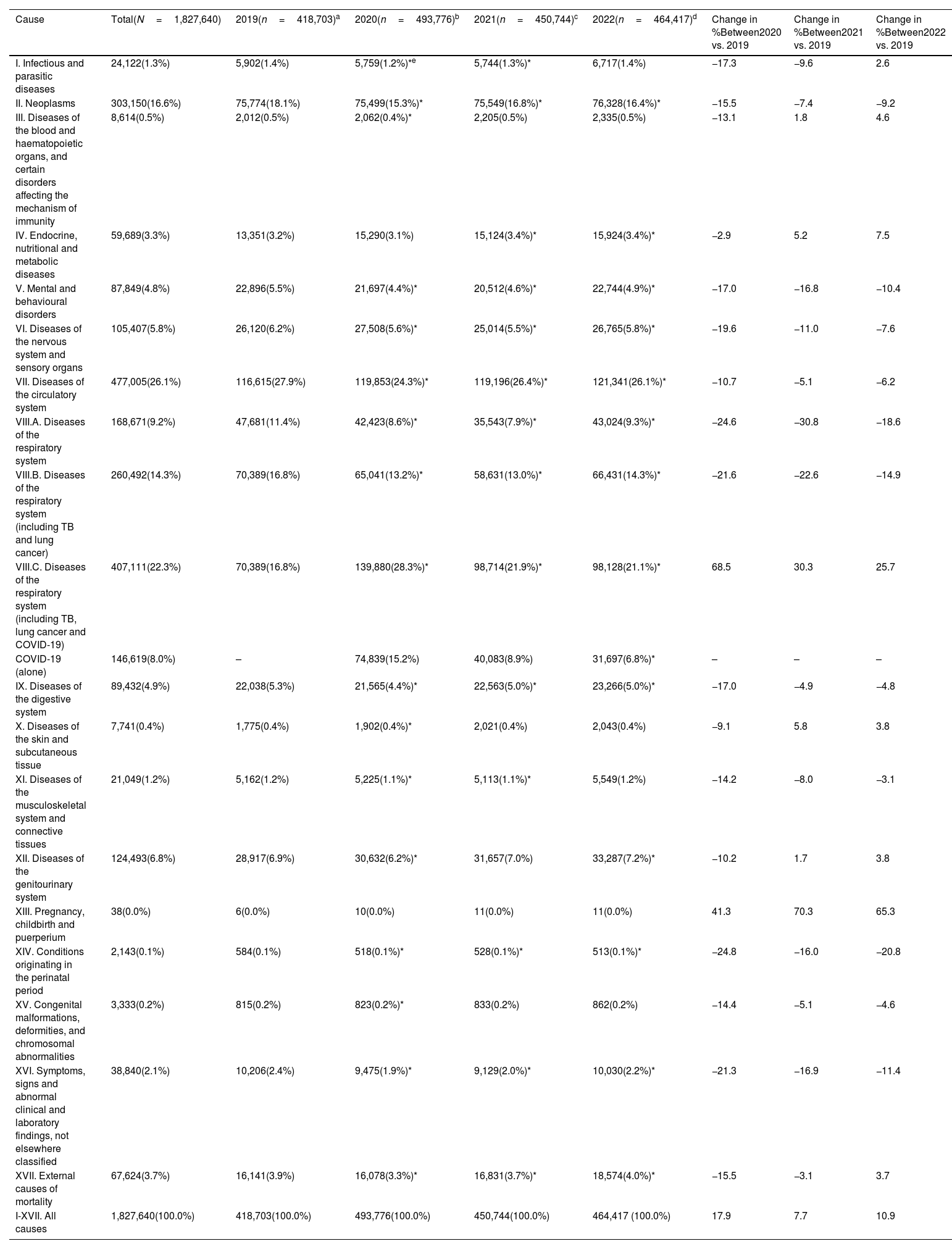
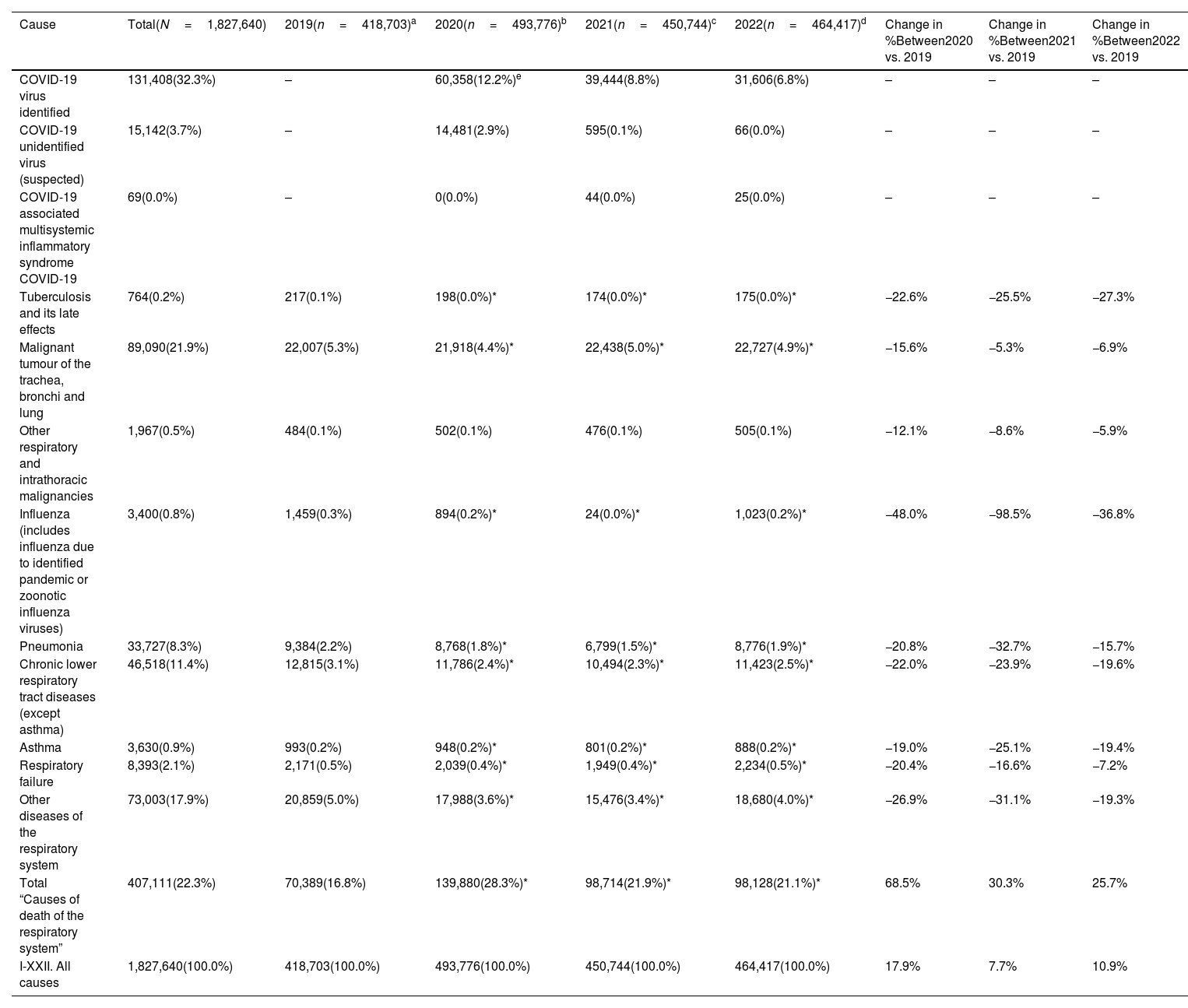
ResultsIn Spain in 2019, a total of 418,703 deaths were recorded (Table 1). Upon closer examination, it was found that respiratory diseases accounted for 70,389 of these deaths, representing 16.8% of the country's proportional mortality. Contrastingly, the situation shifted in 2022, with a total of 464,471 total deaths recorded, including 31,697 attributed to COVID-19. Upon examination of specific causes, all respiratory diseases accounted for 98,128 deaths, constituting 21.1% of Spain's proportional mortality. The 25.7% increase in 2022 was lower than the increases observed in earlier years (2020: 68.5%, 2021: 30.3%) (Table 1). When removing COVID-19 as a cause of death, there was a relative decrease from the 70,389 deaths in 2019, with a decrease of −21.6% in 2020, −22.6% in 2021 and −14.9% in 2022.
Frequency of deaths according to ICD-10-CM categories, proportional mortality (%) and percent change by causes of death in Spain in 2019–2022.
| Cause | Total(N=1,827,640) | 2019(n=418,703)a | 2020(n=493,776)b | 2021(n=450,744)c | 2022(n=464,417)d | Change in %Between2020 vs. 2019 | Change in %Between2021 vs. 2019 | Change in %Between2022 vs. 2019 |
|---|---|---|---|---|---|---|---|---|
| I. Infectious and parasitic diseases | 24,122(1.3%) | 5,902(1.4%) | 5,759(1.2%)*e | 5,744(1.3%)* | 6,717(1.4%) | −17.3 | −9.6 | 2.6 |
| II. Neoplasms | 303,150(16.6%) | 75,774(18.1%) | 75,499(15.3%)* | 75,549(16.8%)* | 76,328(16.4%)* | −15.5 | −7.4 | −9.2 |
| III. Diseases of the blood and haematopoietic organs, and certain disorders affecting the mechanism of immunity | 8,614(0.5%) | 2,012(0.5%) | 2,062(0.4%)* | 2,205(0.5%) | 2,335(0.5%) | −13.1 | 1.8 | 4.6 |
| IV. Endocrine, nutritional and metabolic diseases | 59,689(3.3%) | 13,351(3.2%) | 15,290(3.1%) | 15,124(3.4%)* | 15,924(3.4%)* | −2.9 | 5.2 | 7.5 |
| V. Mental and behavioural disorders | 87,849(4.8%) | 22,896(5.5%) | 21,697(4.4%)* | 20,512(4.6%)* | 22,744(4.9%)* | −17.0 | −16.8 | −10.4 |
| VI. Diseases of the nervous system and sensory organs | 105,407(5.8%) | 26,120(6.2%) | 27,508(5.6%)* | 25,014(5.5%)* | 26,765(5.8%)* | −19.6 | −11.0 | −7.6 |
| VII. Diseases of the circulatory system | 477,005(26.1%) | 116,615(27.9%) | 119,853(24.3%)* | 119,196(26.4%)* | 121,341(26.1%)* | −10.7 | −5.1 | −6.2 |
| VIII.A. Diseases of the respiratory system | 168,671(9.2%) | 47,681(11.4%) | 42,423(8.6%)* | 35,543(7.9%)* | 43,024(9.3%)* | −24.6 | −30.8 | −18.6 |
| VIII.B. Diseases of the respiratory system (including TB and lung cancer) | 260,492(14.3%) | 70,389(16.8%) | 65,041(13.2%)* | 58,631(13.0%)* | 66,431(14.3%)* | −21.6 | −22.6 | −14.9 |
| VIII.C. Diseases of the respiratory system (including TB, lung cancer and COVID-19) | 407,111(22.3%) | 70,389(16.8%) | 139,880(28.3%)* | 98,714(21.9%)* | 98,128(21.1%)* | 68.5 | 30.3 | 25.7 |
| COVID-19 (alone) | 146,619(8.0%) | – | 74,839(15.2%) | 40,083(8.9%) | 31,697(6.8%)* | – | – | – |
| IX. Diseases of the digestive system | 89,432(4.9%) | 22,038(5.3%) | 21,565(4.4%)* | 22,563(5.0%)* | 23,266(5.0%)* | −17.0 | −4.9 | −4.8 |
| X. Diseases of the skin and subcutaneous tissue | 7,741(0.4%) | 1,775(0.4%) | 1,902(0.4%)* | 2,021(0.4%) | 2,043(0.4%) | −9.1 | 5.8 | 3.8 |
| XI. Diseases of the musculoskeletal system and connective tissues | 21,049(1.2%) | 5,162(1.2%) | 5,225(1.1%)* | 5,113(1.1%)* | 5,549(1.2%) | −14.2 | −8.0 | −3.1 |
| XII. Diseases of the genitourinary system | 124,493(6.8%) | 28,917(6.9%) | 30,632(6.2%)* | 31,657(7.0%) | 33,287(7.2%)* | −10.2 | 1.7 | 3.8 |
| XIII. Pregnancy, childbirth and puerperium | 38(0.0%) | 6(0.0%) | 10(0.0%) | 11(0.0%) | 11(0.0%) | 41.3 | 70.3 | 65.3 |
| XIV. Conditions originating in the perinatal period | 2,143(0.1%) | 584(0.1%) | 518(0.1%)* | 528(0.1%)* | 513(0.1%)* | −24.8 | −16.0 | −20.8 |
| XV. Congenital malformations, deformities, and chromosomal abnormalities | 3,333(0.2%) | 815(0.2%) | 823(0.2%)* | 833(0.2%) | 862(0.2%) | −14.4 | −5.1 | −4.6 |
| XVI. Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 38,840(2.1%) | 10,206(2.4%) | 9,475(1.9%)* | 9,129(2.0%)* | 10,030(2.2%)* | −21.3 | −16.9 | −11.4 |
| XVII. External causes of mortality | 67,624(3.7%) | 16,141(3.9%) | 16,078(3.3%)* | 16,831(3.7%)* | 18,574(4.0%)* | −15.5 | −3.1 | 3.7 |
| I-XVII. All causes | 1,827,640(100.0%) | 418,703(100.0%) | 493,776(100.0%) | 450,744(100.0%) | 464,417 (100.0%) | 17.9 | 7.7 | 10.9 |
Examining the causes of respiratory-related deaths in 2022, a decrease was observed compared to those recorded in 2019 (Table 2). There was a relative reduction in specific causes, the top three most significant decrease were −36.8% due to influenza, −27.3% due to tuberculosis, and 19.6% due to chronic diseases of the lower respiratory tract (excluding asthma).
Frequency of deaths, proportional mortality (%) and percent change by specific diseases of the respiratory system in Spain in 2019–2022.
| Cause | Total(N=1,827,640) | 2019(n=418,703)a | 2020(n=493,776)b | 2021(n=450,744)c | 2022(n=464,417)d | Change in %Between2020 vs. 2019 | Change in %Between2021 vs. 2019 | Change in %Between2022 vs. 2019 |
|---|---|---|---|---|---|---|---|---|
| COVID-19 virus identified | 131,408(32.3%) | – | 60,358(12.2%)e | 39,444(8.8%) | 31,606(6.8%) | – | – | – |
| COVID-19 unidentified virus (suspected) | 15,142(3.7%) | – | 14,481(2.9%) | 595(0.1%) | 66(0.0%) | – | – | – |
| COVID-19 associated multisystemic inflammatory syndrome COVID-19 | 69(0.0%) | – | 0(0.0%) | 44(0.0%) | 25(0.0%) | – | – | – |
| Tuberculosis and its late effects | 764(0.2%) | 217(0.1%) | 198(0.0%)* | 174(0.0%)* | 175(0.0%)* | −22.6% | −25.5% | −27.3% |
| Malignant tumour of the trachea, bronchi and lung | 89,090(21.9%) | 22,007(5.3%) | 21,918(4.4%)* | 22,438(5.0%)* | 22,727(4.9%)* | −15.6% | −5.3% | −6.9% |
| Other respiratory and intrathoracic malignancies | 1,967(0.5%) | 484(0.1%) | 502(0.1%) | 476(0.1%) | 505(0.1%) | −12.1% | −8.6% | −5.9% |
| Influenza (includes influenza due to identified pandemic or zoonotic influenza viruses) | 3,400(0.8%) | 1,459(0.3%) | 894(0.2%)* | 24(0.0%)* | 1,023(0.2%)* | −48.0% | −98.5% | −36.8% |
| Pneumonia | 33,727(8.3%) | 9,384(2.2%) | 8,768(1.8%)* | 6,799(1.5%)* | 8,776(1.9%)* | −20.8% | −32.7% | −15.7% |
| Chronic lower respiratory tract diseases (except asthma) | 46,518(11.4%) | 12,815(3.1%) | 11,786(2.4%)* | 10,494(2.3%)* | 11,423(2.5%)* | −22.0% | −23.9% | −19.6% |
| Asthma | 3,630(0.9%) | 993(0.2%) | 948(0.2%)* | 801(0.2%)* | 888(0.2%)* | −19.0% | −25.1% | −19.4% |
| Respiratory failure | 8,393(2.1%) | 2,171(0.5%) | 2,039(0.4%)* | 1,949(0.4%)* | 2,234(0.5%)* | −20.4% | −16.6% | −7.2% |
| Other diseases of the respiratory system | 73,003(17.9%) | 20,859(5.0%) | 17,988(3.6%)* | 15,476(3.4%)* | 18,680(4.0%)* | −26.9% | −31.1% | −19.3% |
| Total “Causes of death of the respiratory system” | 407,111(22.3%) | 70,389(16.8%) | 139,880(28.3%)* | 98,714(21.9%)* | 98,128(21.1%)* | 68.5% | 30.3% | 25.7% |
| I-XXII. All causes | 1,827,640(100.0%) | 418,703(100.0%) | 493,776(100.0%) | 450,744(100.0%) | 464,417(100.0%) | 17.9% | 7.7% | 10.9% |
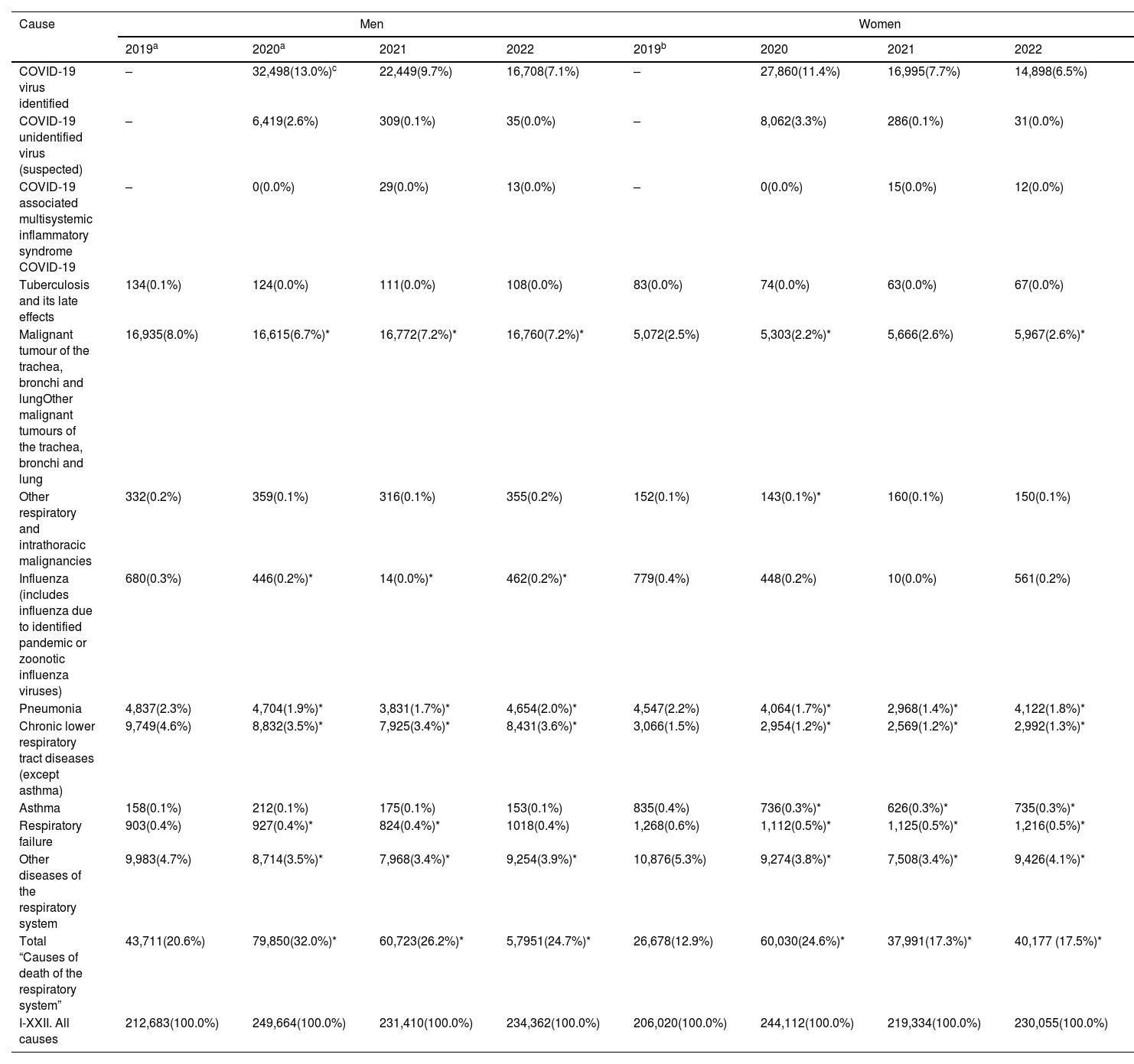
In 2022, proportional mortality from diseases of the respiratory system were higher in men (24.7%) than in women (17.5%). For specific causes, the proportional mortality was substantially higher in women due to asthma, respiratory failure, and other diseases of the respiratory system (Table 3 and e.Fig. 1). The highest mortality associated with respiratory diseases occurred in people aged 50 and above, peaking at 12.2% in the age range of 70–79 years due to the COVID-19 (e.Fig. 1 and e.Table 2).
Frequency of deaths and percentage of mortality by diseases of the respiratory system in 2019–2022 in Spain, by sex.
| Cause | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| 2019a | 2020a | 2021 | 2022 | 2019b | 2020 | 2021 | 2022 | |
| COVID-19 virus identified | – | 32,498(13.0%)c | 22,449(9.7%) | 16,708(7.1%) | – | 27,860(11.4%) | 16,995(7.7%) | 14,898(6.5%) |
| COVID-19 unidentified virus (suspected) | – | 6,419(2.6%) | 309(0.1%) | 35(0.0%) | – | 8,062(3.3%) | 286(0.1%) | 31(0.0%) |
| COVID-19 associated multisystemic inflammatory syndrome COVID-19 | – | 0(0.0%) | 29(0.0%) | 13(0.0%) | – | 0(0.0%) | 15(0.0%) | 12(0.0%) |
| Tuberculosis and its late effects | 134(0.1%) | 124(0.0%) | 111(0.0%) | 108(0.0%) | 83(0.0%) | 74(0.0%) | 63(0.0%) | 67(0.0%) |
| Malignant tumour of the trachea, bronchi and lungOther malignant tumours of the trachea, bronchi and lung | 16,935(8.0%) | 16,615(6.7%)* | 16,772(7.2%)* | 16,760(7.2%)* | 5,072(2.5%) | 5,303(2.2%)* | 5,666(2.6%) | 5,967(2.6%)* |
| Other respiratory and intrathoracic malignancies | 332(0.2%) | 359(0.1%) | 316(0.1%) | 355(0.2%) | 152(0.1%) | 143(0.1%)* | 160(0.1%) | 150(0.1%) |
| Influenza (includes influenza due to identified pandemic or zoonotic influenza viruses) | 680(0.3%) | 446(0.2%)* | 14(0.0%)* | 462(0.2%)* | 779(0.4%) | 448(0.2%) | 10(0.0%) | 561(0.2%) |
| Pneumonia | 4,837(2.3%) | 4,704(1.9%)* | 3,831(1.7%)* | 4,654(2.0%)* | 4,547(2.2%) | 4,064(1.7%)* | 2,968(1.4%)* | 4,122(1.8%)* |
| Chronic lower respiratory tract diseases (except asthma) | 9,749(4.6%) | 8,832(3.5%)* | 7,925(3.4%)* | 8,431(3.6%)* | 3,066(1.5%) | 2,954(1.2%)* | 2,569(1.2%)* | 2,992(1.3%)* |
| Asthma | 158(0.1%) | 212(0.1%) | 175(0.1%) | 153(0.1%) | 835(0.4%) | 736(0.3%)* | 626(0.3%)* | 735(0.3%)* |
| Respiratory failure | 903(0.4%) | 927(0.4%)* | 824(0.4%)* | 1018(0.4%) | 1,268(0.6%) | 1,112(0.5%)* | 1,125(0.5%)* | 1,216(0.5%)* |
| Other diseases of the respiratory system | 9,983(4.7%) | 8,714(3.5%)* | 7,968(3.4%)* | 9,254(3.9%)* | 10,876(5.3%) | 9,274(3.8%)* | 7,508(3.4%)* | 9,426(4.1%)* |
| Total “Causes of death of the respiratory system” | 43,711(20.6%) | 79,850(32.0%)* | 60,723(26.2%)* | 5,7951(24.7%)* | 26,678(12.9%) | 60,030(24.6%)* | 37,991(17.3%)* | 40,177 (17.5%)* |
| I-XXII. All causes | 212,683(100.0%) | 249,664(100.0%) | 231,410(100.0%) | 234,362(100.0%) | 206,020(100.0%) | 244,112(100.0%) | 219,334(100.0%) | 230,055(100.0%) |
Regional disparities were observed, with some autonomous regions experiencing a more pronounced impact on overall mortality, respiratory-related mortality, and specific respiratory diseases (e.Table 1). Asturias stood out with mortality due to the COVID-19 virus identified (42.0%), the Basque Country with tuberculosis (0.4%), malignant tumour of the trachea, bronchi, and lung (27.8%), influenza (2.1%), and asthma (2.1%), the Canary Islands with pneumonia (13.1%), the Balearic Islands with chronic lower respiratory tract diseases (14.7%), Melilla with respiratory failure (6.0%), and Galicia with other diseases of the respiratory system (26.2%). Andalusia was the autonomous regions with the highest proportional mortality in 2022 due to respiratory causes.
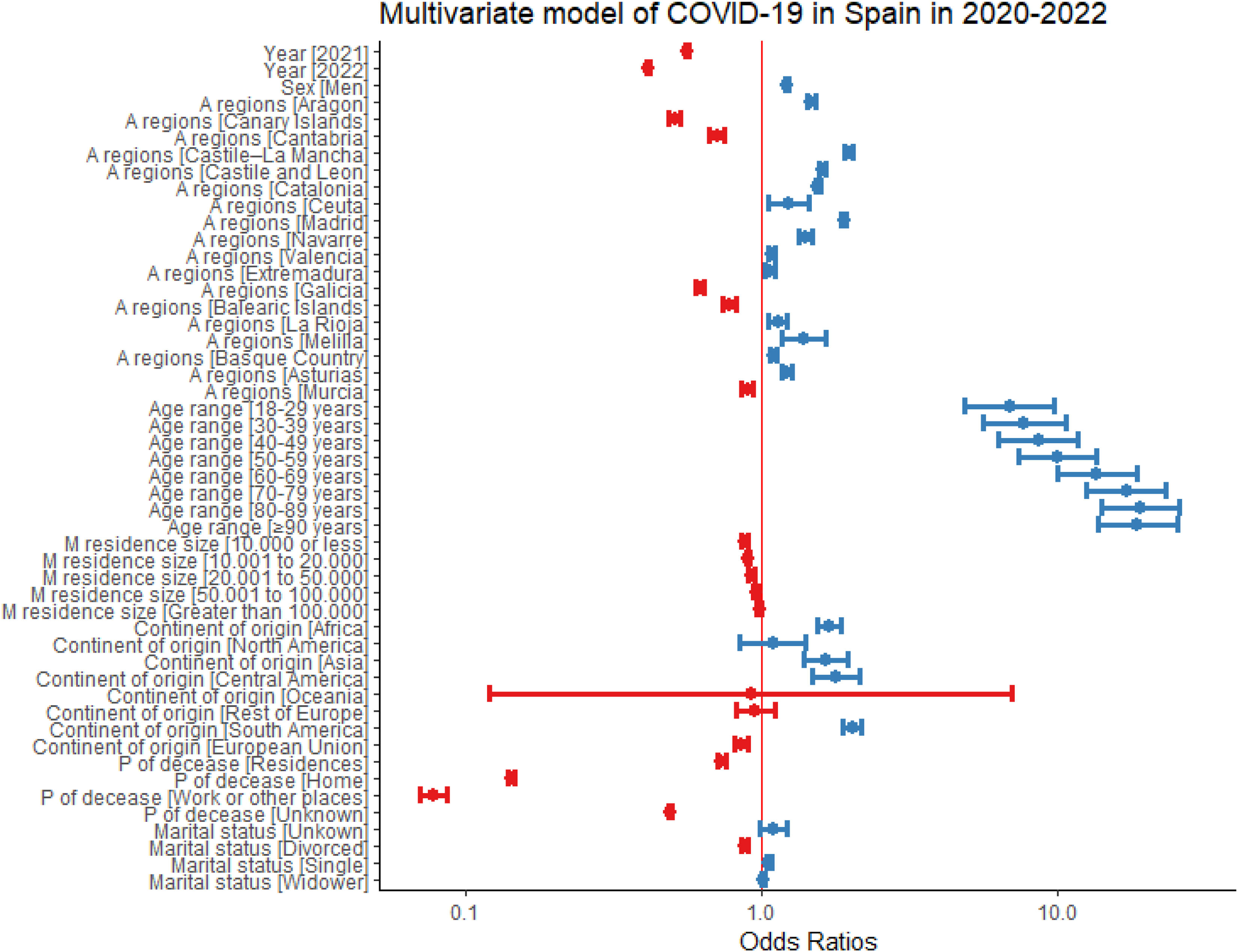
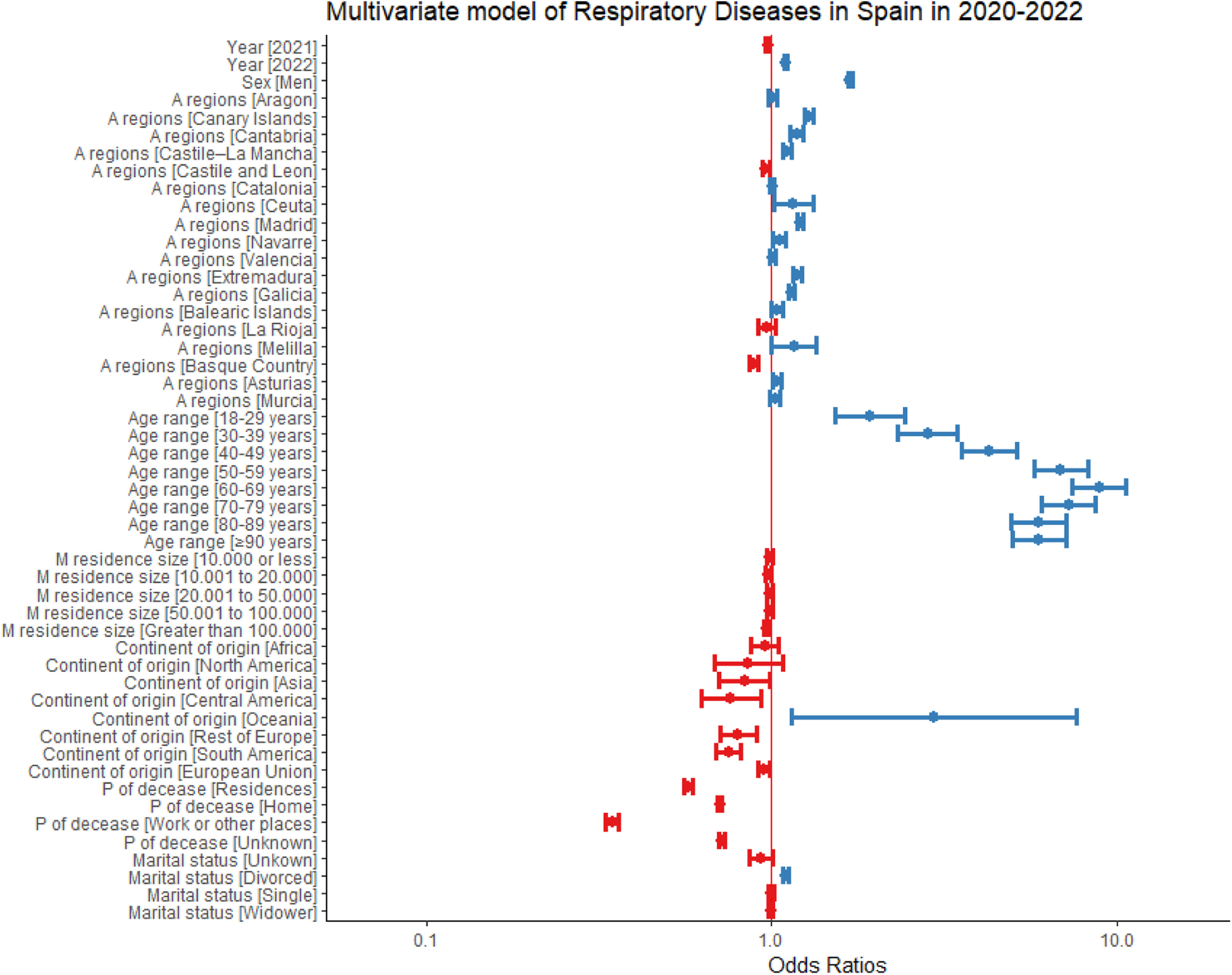
In the multivariate logistic regression analysis, direct associations of certain factors for mortality from respiratory diseases (excluding COVID-19) were confirmed, such as male sex (OR: 1.69, [IC95%: 1.67–1.71]), advanced age (OR: 8.86, [IC95%:7.43–10.7]) up to the sixties, and residing in specific autonomous regions and cities, such as Madrid (OR: 1.20, [IC95%: 1.18–1.23]). Additionally, an inverse association was observed in smaller municipalities, despite significant geographical variability (e.Table 3). Further, those at hospitals had an excess proportional mortality for respiratory diseases, as well as divorced marital status (e.Table 3 and Fig. 1). When we restricted the analysis to COVID diseases, male sex, advanced age, municipality size, and place of death direct associations were confirmed, and an inverse association was observed in residing in European Union countries (e.Table 4 and Fig. 2).
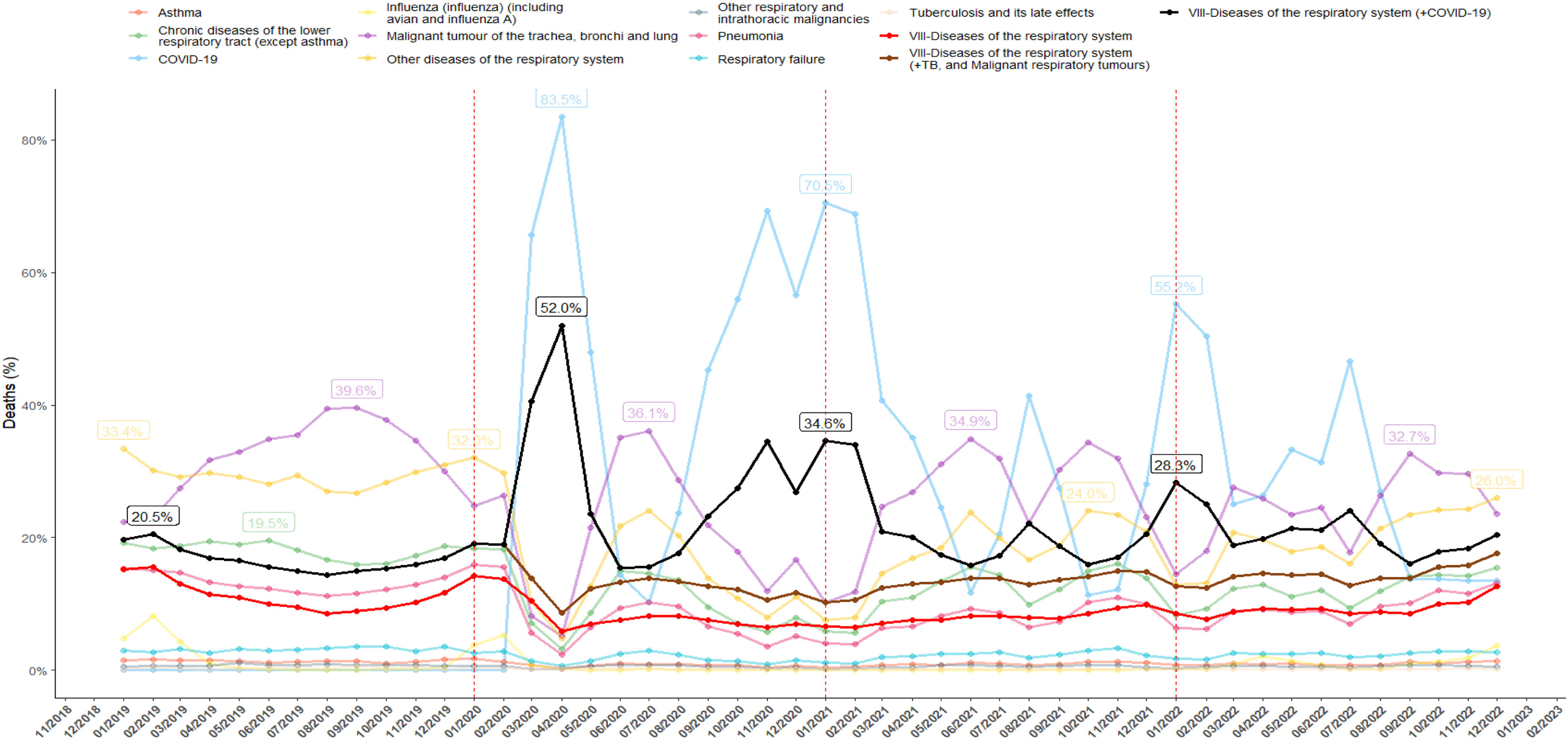
The trend in proportional mortality from respiratory system diseases for specific causes is illustrated, along with the combined trend for respiratory causes, encompassing tuberculosis, malignant respiratory tumours, and COVID-related diseases (black line) (Fig. 3). Additionally, alternative combined respiratory causes are represented: one exclude COVID-related diseases from the combination (brown line), while the other exclude tuberculosis, malignant respiratory tumours and COVID-related and diseases (red line). The usual seasonality with a peak of respiratory mortality in the winter was disrupted in 2020, given the first two pandemic waves. Despite spontaneous peaks and some variability occurring between winter and summer months, the seasonality of respiratory diseases attempts to recover, with the difference between peaks and valleys being less distinct in the year 2022.
Time series (by calendar month) of proportional mortality (%) by each cause, and in total, of diseases of the respiratory system between 2019 and 2022. The mortality percentage appear in the peak periods of each cause within the year and only if they exceed the national average for respiratory causes in that specific year. TB: tuberculosis; Malignant respiratory tumours include malignant tumour of the trachea, bronchi and lung and other respiratory and intrathoracic malignancies.
This study demonstrates that although overall mortality has gradually decreased towards pre-pandemic levels, our study highlights an observable significant increase in deaths due to respiratory diseases in Spain in 2022 compared to 2019. The effects of COVID-19 appear to have influenced mortality and health trends, as reflected in Spain's statistics.13 National demographic and population features such as an aging population and high rates of smoking,14 combined with the presence of COVID-19,15,16 seem to have contributed to the observed increase in respiratory deaths since 2020. It is estimated that the impact of COVID-19, directly and indirectly, in Spain has reduced life expectancy by almost two years,6,7 albeit with marked disparities among autonomous regions. However, it is important to interpret these relationships descriptively rather than causally, as causal inferences require further investigation and consideration of additional factors.
Before the pandemic, respiratory diseases were already a significant burden of morbidity and mortality. The Global Burden of Diseases, Injuries, and Risk Factors (GBD) study, which concluded that out of the 50.5 million deaths worldwide in 1990, around 9.5 million were attributed to pneumonia, tuberculosis, chronic obstructive pulmonary disease (COPD), and lung cancer17 Moreover, estimates projected for 2020 indicated that respiratory diseases would be the third leading cause of death worldwide.17 Not only was this prediction fulfilled, but since 2020, the combined figures of tuberculosis, lung cancer, and COVID-19 place respiratory diseases as the second leading cause of mortality in Spain, representing 28.3%, 21.9%, and 21.1% of deaths in the three years, respectively.
Since the onset of the COVID-19 outbreak, there has been a substantial disruption in the dynamics of global public health strategies, along with significant challenges for healthcare professionals and governments. The pandemic scenario needed strategic decision-making to address the situation, and there is a growing concern about the future consequences that reported increased prevalence of conditions such as depressive and anxiety disorders,18 and cardiometabolic diseases,19 among others will have in the aftermath of COVID-19-related mortality. This phenomenon should not only be seen as a challenge but also as an opportunity for better preparation for future pandemics (strengthening infrastructure, enhancing disease surveillance systems, and fostering interdisciplinary collaboration), and addressing the growing challenge of chronicity or changes in mortality causes.20
In parallel, COVID-19 quickly rose to prominence as a leading cause of mortality in Spain, surpassing other previously significant conditions. This shift in the distribution of mortality causes coincided with an observable increase in deaths because of respiratory diseases, with increases of 68.5% and 30.3% in the first and second pandemic years, respectively, compared to the pre-pandemic period.4,5 In 2022, although there was a 25.7% increase in respiratory causes, it was less pronounced, allowing other causes of mortality to experience increases compared to the pre-pandemic year. Factors that likely contribute to this decrease in COVID-19 mortality very likely were the high vaccination rates of the general population, the emergence of viral variants with lower pathogenicity, and improved clinical efficacy of treatments against severe forms of COVID-19.21 However, our results suggest that, respiratory mortality has not yet returned to pre-pandemic levels, highlighting the ongoing need for respiratory disease management and prevention strategies.
Another relevant finding is the difference in proportional mortality among different autonomous regions, revealing an increase in mortality in specific areas, with Madrid, Catalonia, and Castile-La Mancha standing out. Differences in regional healthcare policies likely contributed to variations in incidence and mortality rates, highlighting their effectiveness.22 Additionally, multivariate analysis confirms the influence of known COVID-19 individual risk factors in these autonomous regions, such as advanced age, municipality size, marital status or place of death. In line with previous reports,23,24 our analyses reported greater odds of death among elders residing in care homes when compared to population in other places (such as home, work or other places). This result underscores the importance of considering specific protection and care strategies in nursing homes to reduce morbidity and mortality of this vulnerable population.25
Finally, this study makes a valuable contribution to the current debate on the classification of causes of death.26 The underestimation of respiratory-related mortality statistics is attributed to the overlap of symptoms and determinants, as well as the chronic nature of many respiratory diseases. For example, it is acknowledged that many patients with chronic respiratory diseases, such as COPD or asthma, die with these conditions, not necessarily because of them.27,28 This poses a clinical challenge in accurately assigning the cause of death to respiratory diseases, given the lack of specificity of respiratory symptoms and signs compared to other significant causes of illness and death, such as cardiovascular or oncological causes. This study highlights the importance of continually improving the standardised coding of death certificates to reflect the burden of respiratory diseases and guide more effective and specific public health strategies more accurately. In the future, addressing these challenges will be crucial in ensuring accurate mortality data and enhancing the development of targeted interventions and policies aimed at reducing the impact of respiratory diseases on public health.
Beyond the above mentioned strengths, a number of limitations must be discussed, particularly in the context of the validity of COVID-19 death certificates. The challenges associated with accurately attributing the cause of death extend beyond respiratory diseases, encompassing the complexities involved in certifying deaths related to infectious diseases during the peak of a pandemic wave, such as COVID-19. The unique clinical presentations and comorbidities associated with viral infections can further complicate the precise determination of the primary cause of death. Substitution of causes of death and premature mortality of individuals with brittle, severe conditions, likely plays a role as well.
On the other hand, the use of data representing the entire population rather than a random sample means that traditional statistical measures, such as standard errors and confidence intervals, may not fully capture the true uncertainty. The global uncertainty might be greater than what is quantified by these statistical measures, as the error could potentially go in any direction. It is essential to consider that while statistical inference techniques are commonly applied, the interpretation of these results should account for the fact that we are working with the entire population rather than a sample.
In conclusion, despite overall mortality largely returning to pre-pandemic levels, our study reveals a persistent impact of COVID-19 on respiratory disease deaths in Spain, with a 25.7% increase in 2022 compared to 2019. Additionally, COVID-19 has had an indirect impact on altering the distribution of causes of death (highlighting the population burden of respiratory diseases in Spain), depleting resources, and causing delays in screening and monitoring services for non-respiratory diseases.
Ethical approvalThis is not necessary, as the work does not involve the use of patient or human subjects data.
FundingThis research project has not received total or partial funding from any pharmaceutical or practice-related company. Therefore, there are no conflicts of interest regarding project management, data analysis, writing process, approval of any version of the submitted manuscript, or the decision to publish.
Declaration of competing interestThe authors declare no conflicts of interest that could be considered to directly or indirectly influence the content of the manuscript.
The authors would like to extend their gratitude to Estefanía Conde for her assistance in the translation of this article.