Evaluating the impact of solid organ neoplasms (SON) and hematological neoplasms (HN) on mortality among RA patients in a nationwide study.
MethodsA retrospective, observational comparison of SON and HN-related deaths in RA patients and the general Spanish population was conducted (Spanish Hospital Discharge Database). Binary logistic regression analyzed the impact of RA on mortality risk from each neoplasm.
ResultsFrom 2016 to 2019, 139,531 neoplasm-related deaths were recorded, including 813 (0.6%) from RA patients. Patients with RA presented a lower mortality rate from SON (85.1% vs 91.2%, OR 0.99), mainly due to colorectal carcinoma (8% vs 10.6%, OR 0.67) and hepatocarcinoma (1% vs 2.7%, OR 0.44), but higher lung neoplasms risk (20.2% vs 18.6%, OR 1.31). HN-related deaths were also more prevalent in RA patients (14.9% vs 8.8%, OR 1.73), especially B and T/NK non-Hodgkin's lymphoma (6% vs 2.8%, OR 2.12) and myeloid leukemia (4.4% vs 2.3%, OR 1.92).
ConclusionRA patients might have a higher mortality risk from lung and hematologic neoplasms. Reducing immunosuppressive burden and developing early-detection programs should be primary goals in this population.
Evaluar el impacto de neoplasias de órgano sólido (NOS) y hematológicas (NH) en la mortalidad de pacientes con AR a nivel nacional.
MétodosEstudio observacional retrospectivo comparativo de muertes por NOS y NH en pacientes con AR versus población general española (Registro de Actividad de Atención Especializada). Se evaluó el impacto de la AR en cada neoplasia mediante regresión logística binaria.
ResultadosEntre 2016 y 2019, se registraron 139.531 muertes por neoplasias, 813 (0,6%) en pacientes con AR. Los pacientes con AR mostraron menor mortalidad por NOS (85,1% vs. 91,2%, OR 0,99), especialmente carcinoma colorrectal (8% vs. 10,6%, OR 0,67) y hepatocarcinoma (1% vs. 2,7%, OR 0,44), pero mayor riesgo de neoplasia pulmonar (20,2% vs. 18,6%, OR 1,31). Las muertes por NH fueron más frecuentes en AR (14,9% vs. 8,8%, OR 1,73), especialmente linfomas no Hodgkin B y T/NK (6% vs. 2,8%, OR 2,12) y leucemia mieloide (4,4% vs. 2,3%, OR 1,92).
ConclusiónLos pacientes con AR podrían tener un mayor riesgo de mortalidad por neoplasias pulmonares y hematológicas. La reducción de la carga inmunosupresora y el desarrollo de programas de detección temprana deben ser objetivos clave en esta población.
Rheumatoid arthritis (RA) is a persistent inflammatory multisystemic disorder of unknown cause and autoimmune origin, primarily targeting peripheral joints symmetrically, but also causing extra-articular symptoms.1 Patients with RA have a lower survival rate compared to the general population, primarily due to infections, interstitial lung disease or pulmonary hypertension, among others.1–3 Evidence supports that RA is linked to kidney disease, cardiovascular disease, and a higher overall incidence of cancer due to certain types of neoplasms.4 Considering this, our objective was to evaluate the impact of solid organ neoplasms (SON) and hematological neoplasms (HN) on mortality among RA patients in a nationwide study conducted in Spain, which has a population of 47 million.
Materials and methodsWe analyzed data from the Spanish Hospital Discharge Database (SNHDD), a publicly accessible registry managed by the Spanish Government, containing up to 20 discharge diagnoses per admission since January 1, 2016. We compared the proportion of deaths attributable to different neoplasm lineages among RA patients to those in the general Spanish population from 2016 to 2019.
Study populationAccording to the database structure, the primary diagnosis determined the reason for admission and, if applicable, the cause of death. All deaths attributed to neoplasms (coded from C.00 to D.49 in ICD-10-CM) were examined in this period. Patients with RA were identified according to the ICD-10 CM codes M05 and M06. Patients with any other autoimmune disease that could alter the risk of neoplasm in the AR population were excluded, including systemic lupus erythematosus (SLE) (M32), Sjögren's syndrome (M35) or systemic sclerosis (M34).4,5 The remaining non-RA patients were considered the control group.
Variables and neoplasm-related deathsIn line with ICD-10-CM guidelines, neoplasm-related deaths were categorized as follows: malignant neoplasms encompassing solid organ malignancies (C00–C80), hematological malignancies (C81–C96), in situ neoplasms (D00–D09), benign solid organ neoplasms (D10D36 and D3A), and neoplasms with unknown or unspecified behavior (D37–D49), including both solid organ and hematological neoplasms. Finally, the main SON and HN lineages, and subsequent subclassifications, were considered apart.
Statistical analysisEpidemiological data and neoplasm death proportions between RA patients and the general population, were analyze. Binary logistic regression determined RA's impact on mortality risk from each neoplasm type, adjusting for age, gender, and tobacco and alcohol use. Analyses were conducted using SPSS version 26.0 (IBM, Spain).
EthicsThe research adheres to the principles outlined in the Declaration of Helsinki and received approval from the local research ethics committee. Data were shared in anonymized form, with all identifiable patient information removed.
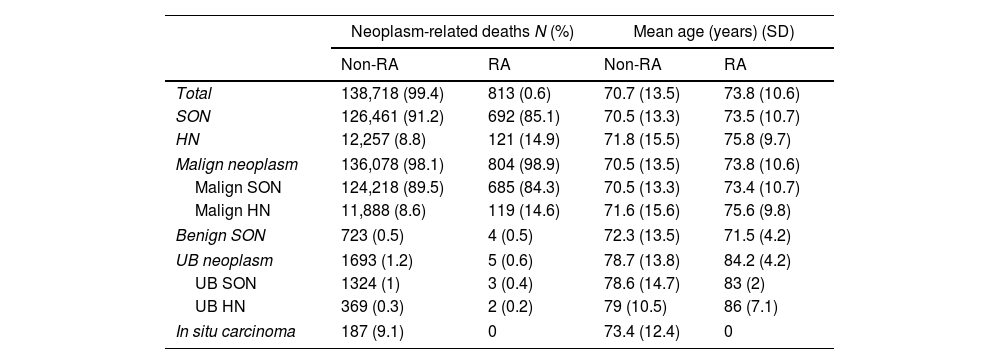
ResultsBetween 2016 and 2019, Spain had an average population of 46,704,229 individuals. During this period, 705,557 deaths were recorded in hospitals. Out of which, 139,531 (19.8%) were attributed to neoplasms, 813 with RA (0.6%) (Table 1).
Differences in neoplasm related deaths for RA patients and the general Spanish population for the period 2016–2019.
| Neoplasm-related deaths N (%) | Mean age (years) (SD) | |||
|---|---|---|---|---|
| Non-RA | RA | Non-RA | RA | |
| Total | 138,718 (99.4) | 813 (0.6) | 70.7 (13.5) | 73.8 (10.6) |
| SON | 126,461 (91.2) | 692 (85.1) | 70.5 (13.3) | 73.5 (10.7) |
| HN | 12,257 (8.8) | 121 (14.9) | 71.8 (15.5) | 75.8 (9.7) |
| Malign neoplasm | 136,078 (98.1) | 804 (98.9) | 70.5 (13.5) | 73.8 (10.6) |
| Malign SON | 124,218 (89.5) | 685 (84.3) | 70.5 (13.3) | 73.4 (10.7) |
| Malign HN | 11,888 (8.6) | 119 (14.6) | 71.6 (15.6) | 75.6 (9.8) |
| Benign SON | 723 (0.5) | 4 (0.5) | 72.3 (13.5) | 71.5 (4.2) |
| UB neoplasm | 1693 (1.2) | 5 (0.6) | 78.7 (13.8) | 84.2 (4.2) |
| UB SON | 1324 (1) | 3 (0.4) | 78.6 (14.7) | 83 (2) |
| UB HN | 369 (0.3) | 2 (0.2) | 79 (10.5) | 86 (7.1) |
| In situ carcinoma | 187 (9.1) | 0 | 73.4 (12.4) | 0 |
SD: standard deviation, RA: rheumatoid arthritis, SON: solid organ neoplasm, HN: hematological neoplasm, UB: uncertain behavior.
When examining neoplasm-related deaths in RA patients versus the general Spanish population, several differences emerged. In RA patients, 85.1% of neoplasm-related deaths were linked to SON, compared to 91.2% in the general population. By contrast, 14.9% were associated with hematologic neoplasms (HN), compared to 8.8% in the broader population. Additionally, the average age of rheumatoid arthritis patients who died from neoplasms (73.8 vs 70.7), HN (75.8 vs 71.8), and SON (73.5 vs 70.5) was higher. Given these disparities, a more nuanced examination, accounting for specific HN and SON subtypes was conducted
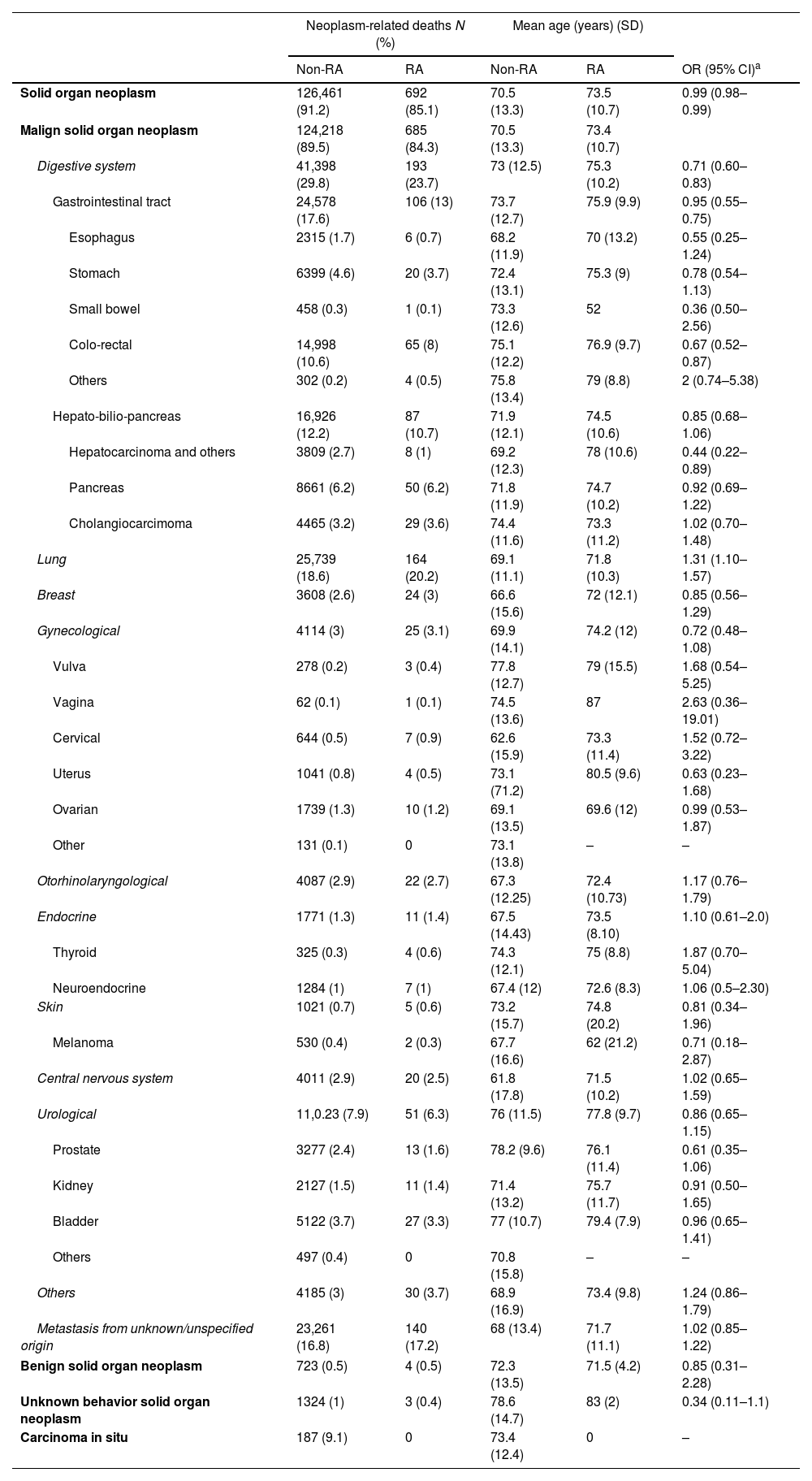
Solid organ neoplasmsThe analysis confirmed that RA patients presented a lower mortality rate from SON (85.1% vs 91.2%, OR=0.99, 95% CI 0.98–0.99) than the general Spanish population (Table 2). This was attributable to a lower proportion of deaths from malignant digestive system neoplasms (23.7% vs 29.8%, OR=0.71, 95% CI 0.60–0.83), related to hepatocarcinoma (1% vs 2.7%, OR=0.44, 95% CI 0.22–0.89) and to colorectal neoplasms (8% vs 10.6%, OR=0.67, 95% CI 0.52–0.87). By contrast, RA was associated with a higher mortality risk from lung neoplasms (20.2% vs 18.6%, OR=1.31, 95% CI 1.10–1.57).
Difference in solid organ neoplasm related deaths for RA patients and the general Spanish population by lineage.
| Neoplasm-related deaths N (%) | Mean age (years) (SD) | ||||
|---|---|---|---|---|---|
| Non-RA | RA | Non-RA | RA | OR (95% CI)a | |
| Solid organ neoplasm | 126,461 (91.2) | 692 (85.1) | 70.5 (13.3) | 73.5 (10.7) | 0.99 (0.98–0.99) |
| Malign solid organ neoplasm | 124,218 (89.5) | 685 (84.3) | 70.5 (13.3) | 73.4 (10.7) | |
| Digestive system | 41,398 (29.8) | 193 (23.7) | 73 (12.5) | 75.3 (10.2) | 0.71 (0.60–0.83) |
| Gastrointestinal tract | 24,578 (17.6) | 106 (13) | 73.7 (12.7) | 75.9 (9.9) | 0.95 (0.55–0.75) |
| Esophagus | 2315 (1.7) | 6 (0.7) | 68.2 (11.9) | 70 (13.2) | 0.55 (0.25–1.24) |
| Stomach | 6399 (4.6) | 20 (3.7) | 72.4 (13.1) | 75.3 (9) | 0.78 (0.54–1.13) |
| Small bowel | 458 (0.3) | 1 (0.1) | 73.3 (12.6) | 52 | 0.36 (0.50–2.56) |
| Colo-rectal | 14,998 (10.6) | 65 (8) | 75.1 (12.2) | 76.9 (9.7) | 0.67 (0.52–0.87) |
| Others | 302 (0.2) | 4 (0.5) | 75.8 (13.4) | 79 (8.8) | 2 (0.74–5.38) |
| Hepato-bilio-pancreas | 16,926 (12.2) | 87 (10.7) | 71.9 (12.1) | 74.5 (10.6) | 0.85 (0.68–1.06) |
| Hepatocarcinoma and others | 3809 (2.7) | 8 (1) | 69.2 (12.3) | 78 (10.6) | 0.44 (0.22–0.89) |
| Pancreas | 8661 (6.2) | 50 (6.2) | 71.8 (11.9) | 74.7 (10.2) | 0.92 (0.69–1.22) |
| Cholangiocarcimoma | 4465 (3.2) | 29 (3.6) | 74.4 (11.6) | 73.3 (11.2) | 1.02 (0.70–1.48) |
| Lung | 25,739 (18.6) | 164 (20.2) | 69.1 (11.1) | 71.8 (10.3) | 1.31 (1.10–1.57) |
| Breast | 3608 (2.6) | 24 (3) | 66.6 (15.6) | 72 (12.1) | 0.85 (0.56–1.29) |
| Gynecological | 4114 (3) | 25 (3.1) | 69.9 (14.1) | 74.2 (12) | 0.72 (0.48–1.08) |
| Vulva | 278 (0.2) | 3 (0.4) | 77.8 (12.7) | 79 (15.5) | 1.68 (0.54–5.25) |
| Vagina | 62 (0.1) | 1 (0.1) | 74.5 (13.6) | 87 | 2.63 (0.36–19.01) |
| Cervical | 644 (0.5) | 7 (0.9) | 62.6 (15.9) | 73.3 (11.4) | 1.52 (0.72–3.22) |
| Uterus | 1041 (0.8) | 4 (0.5) | 73.1 (71.2) | 80.5 (9.6) | 0.63 (0.23–1.68) |
| Ovarian | 1739 (1.3) | 10 (1.2) | 69.1 (13.5) | 69.6 (12) | 0.99 (0.53–1.87) |
| Other | 131 (0.1) | 0 | 73.1 (13.8) | – | – |
| Otorhinolaryngological | 4087 (2.9) | 22 (2.7) | 67.3 (12.25) | 72.4 (10.73) | 1.17 (0.76–1.79) |
| Endocrine | 1771 (1.3) | 11 (1.4) | 67.5 (14.43) | 73.5 (8.10) | 1.10 (0.61–2.0) |
| Thyroid | 325 (0.3) | 4 (0.6) | 74.3 (12.1) | 75 (8.8) | 1.87 (0.70–5.04) |
| Neuroendocrine | 1284 (1) | 7 (1) | 67.4 (12) | 72.6 (8.3) | 1.06 (0.5–2.30) |
| Skin | 1021 (0.7) | 5 (0.6) | 73.2 (15.7) | 74.8 (20.2) | 0.81 (0.34–1.96) |
| Melanoma | 530 (0.4) | 2 (0.3) | 67.7 (16.6) | 62 (21.2) | 0.71 (0.18–2.87) |
| Central nervous system | 4011 (2.9) | 20 (2.5) | 61.8 (17.8) | 71.5 (10.2) | 1.02 (0.65–1.59) |
| Urological | 11,0.23 (7.9) | 51 (6.3) | 76 (11.5) | 77.8 (9.7) | 0.86 (0.65–1.15) |
| Prostate | 3277 (2.4) | 13 (1.6) | 78.2 (9.6) | 76.1 (11.4) | 0.61 (0.35–1.06) |
| Kidney | 2127 (1.5) | 11 (1.4) | 71.4 (13.2) | 75.7 (11.7) | 0.91 (0.50–1.65) |
| Bladder | 5122 (3.7) | 27 (3.3) | 77 (10.7) | 79.4 (7.9) | 0.96 (0.65–1.41) |
| Others | 497 (0.4) | 0 | 70.8 (15.8) | – | – |
| Others | 4185 (3) | 30 (3.7) | 68.9 (16.9) | 73.4 (9.8) | 1.24 (0.86–1.79) |
| Metastasis from unknown/unspecified origin | 23,261 (16.8) | 140 (17.2) | 68 (13.4) | 71.7 (11.1) | 1.02 (0.85–1.22) |
| Benign solid organ neoplasm | 723 (0.5) | 4 (0.5) | 72.3 (13.5) | 71.5 (4.2) | 0.85 (0.31–2.28) |
| Unknown behavior solid organ neoplasm | 1324 (1) | 3 (0.4) | 78.6 (14.7) | 83 (2) | 0.34 (0.11–1.1) |
| Carcinoma in situ | 187 (9.1) | 0 | 73.4 (12.4) | 0 | – |
SD: standard deviation, RA: rheumatoid arthritis, OR: odds ratio, CI: confidence interval.
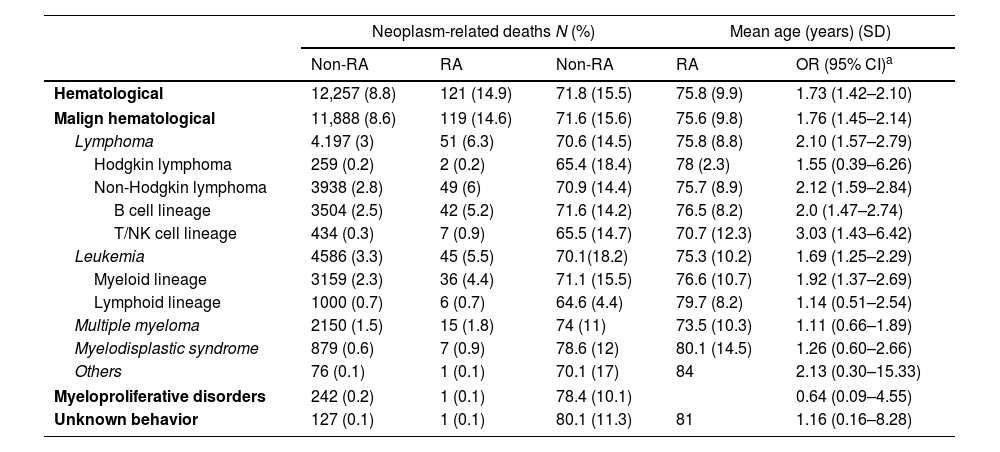
Individuals with RA exhibited a heightened mortality risk from HN compared to the general Spanish populace (14.9% vs 8.8%, OR=1.73, 95% CI 1.42–2.10) (Table 3). This difference was primarily because of deaths from non-Hodgkin lymphoma (6% vs 2.8%, OR=2.12, 95% CI 1.59–2.84), encompassing both B cell (5.2% vs 2.5%, OR=2, 95% CI 1.47–2.74) and T/NK cell lineages (0.9% vs 0.3%, OR=3.03, 95% CI 1.43–6.42), as well as both acute and chronic leukemia (5.5% vs 3.3%, OR=1.69, 95% CI 1.25–2.29), particularly myeloid lineage (4.4% vs 2.3%, OR=1.92, 95% CI 1.37–2.69).
Differences in Hematological neoplasm related deaths for RA patients and the general Spanish population by lineage.
| Neoplasm-related deaths N (%) | Mean age (years) (SD) | ||||
|---|---|---|---|---|---|
| Non-RA | RA | Non-RA | RA | OR (95% CI)a | |
| Hematological | 12,257 (8.8) | 121 (14.9) | 71.8 (15.5) | 75.8 (9.9) | 1.73 (1.42–2.10) |
| Malign hematological | 11,888 (8.6) | 119 (14.6) | 71.6 (15.6) | 75.6 (9.8) | 1.76 (1.45–2.14) |
| Lymphoma | 4.197 (3) | 51 (6.3) | 70.6 (14.5) | 75.8 (8.8) | 2.10 (1.57–2.79) |
| Hodgkin lymphoma | 259 (0.2) | 2 (0.2) | 65.4 (18.4) | 78 (2.3) | 1.55 (0.39–6.26) |
| Non-Hodgkin lymphoma | 3938 (2.8) | 49 (6) | 70.9 (14.4) | 75.7 (8.9) | 2.12 (1.59–2.84) |
| B cell lineage | 3504 (2.5) | 42 (5.2) | 71.6 (14.2) | 76.5 (8.2) | 2.0 (1.47–2.74) |
| T/NK cell lineage | 434 (0.3) | 7 (0.9) | 65.5 (14.7) | 70.7 (12.3) | 3.03 (1.43–6.42) |
| Leukemia | 4586 (3.3) | 45 (5.5) | 70.1(18.2) | 75.3 (10.2) | 1.69 (1.25–2.29) |
| Myeloid lineage | 3159 (2.3) | 36 (4.4) | 71.1 (15.5) | 76.6 (10.7) | 1.92 (1.37–2.69) |
| Lymphoid lineage | 1000 (0.7) | 6 (0.7) | 64.6 (4.4) | 79.7 (8.2) | 1.14 (0.51–2.54) |
| Multiple myeloma | 2150 (1.5) | 15 (1.8) | 74 (11) | 73.5 (10.3) | 1.11 (0.66–1.89) |
| Myelodisplastic syndrome | 879 (0.6) | 7 (0.9) | 78.6 (12) | 80.1 (14.5) | 1.26 (0.60–2.66) |
| Others | 76 (0.1) | 1 (0.1) | 70.1 (17) | 84 | 2.13 (0.30–15.33) |
| Myeloproliferative disorders | 242 (0.2) | 1 (0.1) | 78.4 (10.1) | 0.64 (0.09–4.55) | |
| Unknown behavior | 127 (0.1) | 1 (0.1) | 80.1 (11.3) | 81 | 1.16 (0.16–8.28) |
SD: standard deviation, RA: rheumatoid arthritis, OR: odds ratio, CI: confidence interval.
Literature has frequently addressed the heightened risk of neoplasm development among RA patients, recognizing that this population is more vulnerable to various forms of cancer.4,6,7 However, previous studies have often fallen short in thoroughly quantifying the specific increase in risk associated with different types of neoplasms and, more importantly, it's subsequent impact on mortality. Additionally, there has been a lack of comprehensive classification and analysis of the various neoplasms that predominantly affect RA patients.8
To this respect, this nationwide study assesses that RA patients face a higher mortality risk from hematological neoplasms (HN), particularly non-Hodgkin lymphoma and leukemia, as well as from lung cancer. While other studies have shown that these neoplasms do indeed present a higher incidence in RA patients, mortality figures were not always confirmed.4,6,7,9 The large population size of our study, combined with the ability to describe mortality risk after adjustment in the general population, lends strength to our findings. Therefore, autoimmunity, B-cell and interleukin-6 inflammatory pathway hyperactivation, direct tissue injury or chronic inflammation, along with baseline immunosuppressive burden, seem to directly lead to a long-term higher mortality risk from malignancy in RA population.1,8,9
Conversely, our study showed that RA patients might exhibit lower mortality from other solid organ neoplasms (SON), especially colorectal neoplasms and hepatocarcinoma, this is likely due to better therapeutic adherence and follow-up within the Spanish public healthcare system, as described in previous reports.5,7 The use of non-steroidal anti-inflammatory drugs has also been proposed as a potential mechanism.7,8 Nevertheless, the continued monitoring of RA patients during their management could also partially explain the later age at which they die from these conditions.
Given the aforementioned observations, future research should delve into the underlying mechanisms that contribute to these differential outcomes. Understanding these processes could lead to the development of personalized medical approaches that improve the prognosis of RA patients and address the specific risks associated with different types of neoplasms.8,10
Despite following and including STROBE recommendations, several limitations exist. First, the observed relations should be interpreted from a descriptive perspective, and not strictly causal. The study lacked detailed data on disease progression, clinical features, histopathology, and immunosuppressive treatments, weakening further conclusions. Besides, focusing on hospital admissions introduced selection bias and limited analysis ability. However, the evaluation relied on categorical variables like deaths from specific conditions, less prone to misclassification. Accurate RA prevalence assessment in the databases was unfeasible, preventing precise calculations of neoplasm rates, risks, or incidences. Comparisons were limited to death estimates, indicating proportions and death risks rather than absolute risk ratios. This approach may slightly affect the estimated death risks for different neoplasms in RA patients.
In conclusion, this data highlights that individuals with rheumatoid arthritis (RA) might face a significantly increased risk of death from hematologic neoplasms (HN), particularly from non-Hodgkin lymphoma and leukemia, as well as lung cancer. It is important to study the baseline increase in the risk of cancer in RA patients to understand how treatments might affect specific neoplasms incidence. This addresses the necessity for tailored strategies aimed at mitigating the immunosuppressive effects associated with RA treatments and enhancing early detection of these malignancies.
EthicsThe research followed the Declaration of Helsinki guidelines and obtained approval from the local ethics committee (PI 162/24). Data were anonymized to remove identifiable patient information. Informed consent was considered unnecessary under Spanish law and the study's protocol.
FundingNone.
Conflict of interestThe authors declare no financial conflicts of interest or personal relationships that could bias the findings reported in this paper.
Data availabilityData accessible upon request.