To study effectiveness and satisfaction with a virtual reality-based balance rehabilitation system (BioTrak) for patients with acquired brain injury (ABI).
Materials and methodsTen patients with chronic hemiparesis (chronicity>6 months) following an ABI completed a 20-session programme using the balance reaching-task module of the BioTrak system. All patients were assessed at baseline, at the end of treatment and one month later with the Berg Balance Scale (BBS), the Tinetti Performance-Oriented Mobility Assessment (POMA), and the computerised posturography tool NedSVE/IBV. The posturography study included analysis of sensory indexes, limits of stability and rhythmic weight shift. The usability study was conducted using an ad hoc questionnaire.
ResultsRepeated measures ANOVA showed a significant improvement in BBS (P<.01), TBS (P<.01), vestibular index (P<.05), and anterior–posterior weight shift (P<.05); a trend in the same direction was also found for medial lateral weight shift (P=.059). The post hoc analysis revealed significant improvement between the initial and final assessments for BBS, POMA and anterior–posterior weight shift control; gains remained a month after completing the programme. The system showed a high degree of usability in terms of presence, immersion and user-friendliness, and there was a significant absence of adverse effects.
ConclusionOur results confirm the utility of virtual reality systems for balance rehabilitation in this population. Usability data suggest that BioTrak could be adapted for use in multiple rehabilitation settings by a high number of patients.
Estudio de efectividad y satisfacción de un sistema de realidad virtual (BioTrak) para la rehabilitación del equilibrio en pacientes con daño cerebral adquirido (DCA).
Material y métodosDiez pacientes con una hemiparesia crónica (>6 meses) como secuela de un DCA participaron en un programa de 20 sesiones con el módulo de equilibrio mediante alcances del sistema BioTrak. Todos los pacientes fueron valorados al inicio, al final del tratamiento y un mes después de finalizar el mismo con la Berg Balance Scale (BBS) y la Tinetti Performance-Oriented Mobility Assessment (POMA), así como mediante la posturografía dinamométrica computarizada NedSVE/IBV. El estudio posturográfico incluyó el análisis de índices sensoriales, del desplazamiento rítmico del peso, así como de los límites de estabilidad. El estudio de usabilidad se realizó mediante un cuestionario elaborado ad hoc.
ResultadosUn ANOVA de medidas repetidas mostró una mejora significativa en BBS (p<0,01), POMA (p<0,01), índice vestibular (p<0,05), control rítmico antero-posterior (p<0,05) y una tendencia a la significación en el control medio-lateral (p=0,059). El análisis post hoc reveló mejoras significativas entre la valoración inicial y final en la BBS, la POMA y en control antero-posterior, que se mantuvieron al mes de completar el tratamiento. El sistema mostró un alto grado de usabilidad, tanto en aspectos positivos (presencia, inmersión, facilidad de uso) como por la ausencia de efectos adversos.
ConclusiónNuestros resultados confirman la validez de los sistemas de realidad virtual para la rehabilitación del equilibrio en esta población. Las características de usabilidad del sistema BioTrak permite la generalización del sistema a un alto número de pacientes y entornos.
Balance requires the simultaneous and continuous processing of data from multiple systems, including sensory information (visual, vestibular, and proprioceptive), cognitive integration (especially attention and executive functions), cerebellar function, and obviously, sensory and motor feedback.1 The complexity of this mechanism explains why postural imbalance is a common symptom in patients who have suffered acquired brain injury (ABI), since this disease is frequently associated with dysfunctions of the central and peripheral nervous systems, sensory organs, the musculoskeletal system, and other systems and structures.2 In addition to being highly prevalent, balance and postural control disorders are a frequent cause of falls and limit patients’ autonomy and independence in activities of daily life (ADL).3,4 Recovering balance is therefore one of the primary objectives of motor rehabilitation in patients with ABI.
Recently acquired knowledge about plasticity in both healthy and injured brains has completely changed strategies for recovering deficits resulting from an ABI. Today, doctors unanimously accept that patients’ recovery (and not only motor recovery) following brain injury will be more effective where there is early and intensive therapy focused on the task being recovered.5 In addition, we know that results are even more favourable on the functional level if training includes specific sensory feedback.6 This simple and yet revolutionary approach has quickly been assimilated by new technologies. It is especially present in systems allowing researchers to design rehabilitation programmes that are true to the principles of brain plasticity (repetition and task specificity in a natural, rich, and motivating environment). Virtual reality-based systems are a good example; their use in the area of neurorehabilitation is increasing, and they deliver clearly beneficial results.7–10
In the last few decades, researchers have shown a mounting interest in developing virtual reality-based motor rehabilitation systems for the treatment of different brain pathologies. There are several studies examining virtual reality-based systems specifically designed for upper limb rehabilitation.11,12 However, fewer studies have been able to demonstrate the clinical efficacy of these programmes for restoring other functions such as balance or gait in hemiparetic patients.13–15
With regard to the virtual reality-based rehabilitation of postural control and balance, multiple programmes have been developed that create virtual realities with 2D graphics16 and 3D graphics17,18 using different devices: haptic systems,19 head-mounted devices,20 CAVE systems,21 and others. Our study group has participated in other recent lines of work, which provide clinical content for tools (commercial gaming consoles) that make use of postural control for game-playing purposes.22,23 Although a wide variety of devices are available, most neurorehabilitation departments prefer conventional therapies due to the difficulties of installing equipment in clinical settings, the consequences of postural control training for the patient's safety, or usability problems specific to balance training. At most, professionals may use rehabilitation programmes associated with posturography systems.24–26
From a therapeutic viewpoint, there is still a marked need for virtual reality-based rehabilitation systems that could easily be installed in a clinical setting and would be sufficiently specific and flexible enough for use in all clinical stages of conditions underlying ABI. BioTrak is a virtual reality-based rehabilitation programme which includes 3 modules specifically designed for the motor, cognitive, and psychosocial rehabilitation of patients with different neurological lesions. In its motor rehabilitation module for balance, BioTrak provides 2 different treatment approaches by including dynamic reaching and weight shifting tasks on a pressure platform. This study specifically reports the data regarding satisfaction with and efficacy of the standing and reaching balance exercises in patients with ABI.
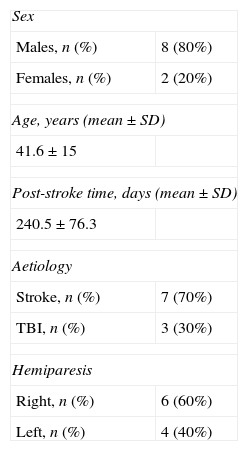
Materials and methodsParticipantsA total of 120 patients with ABI, treated between January and July 2011 in a department specialising in their condition, were eligible to participate in this study according to the criteria listed below. All included patients had to present hemiparesis due to ABI, a stable clinical state, an adequate cognitive level (score on the Mini Mental State Examination≥24),27 a degree of spasticity score below 3 according to the Ashworth Scale,28 and ability to perform dynamic standing balance as defined in the Brunnel Balance Assessment (BBA) (section 3, level 9).29 The exclusion criteria were as follows: (a) unilateral neglect syndrome; (b) ataxia and/or other cerebellar symptoms; (c) Severe visual problems that would hinder interaction with the system, and (d) comprehension deficits that would interfere with proper task completion. Table 1 lists patients’ clinical and demographic characteristics.
Experimental protocolEquipmentThe device includes a PC, a 47-in panoramic screen, and a tracking system (optical, electromagnetic, or using depth sensors like those used in the Kinect™ device)21 allowing the individual to interact with the virtual setting. The optical tracking system used here has 3 cameras that detect the subject's position with the help of reflective markers placed on specific parts of the body (ankle, wrist, shoulders or head depending on the task) so as to transfer his/her position to the virtual reality setting. In addition, Biotrack includes a patient management module that allows the therapist to enter new patients, design personalised work sessions, and check patient progress by analysing results.
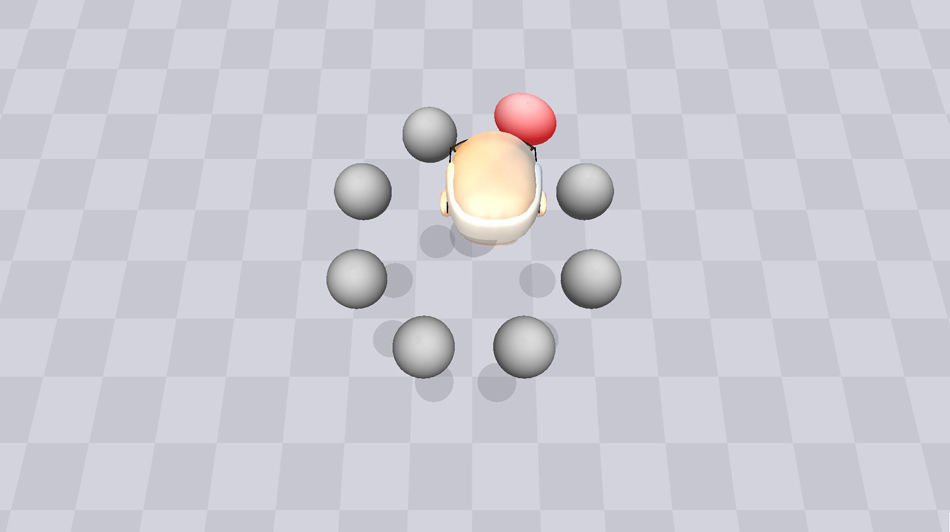
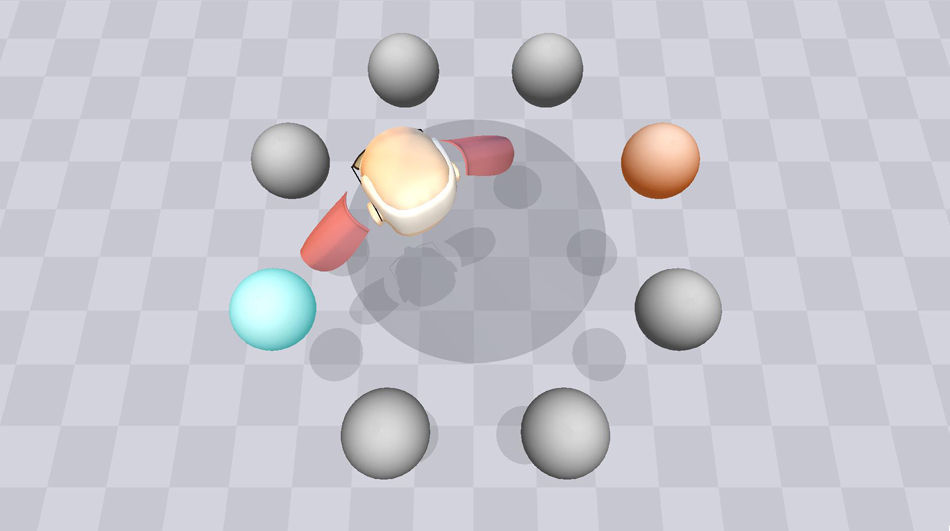
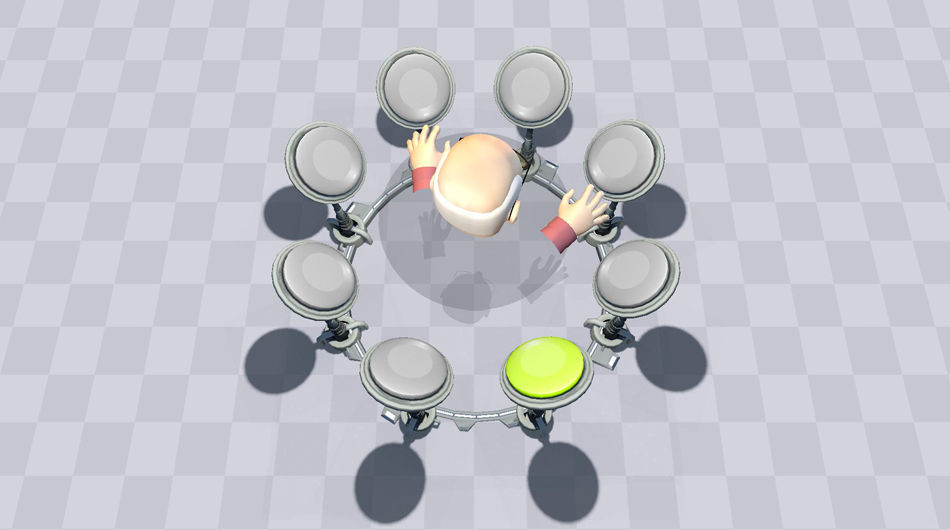
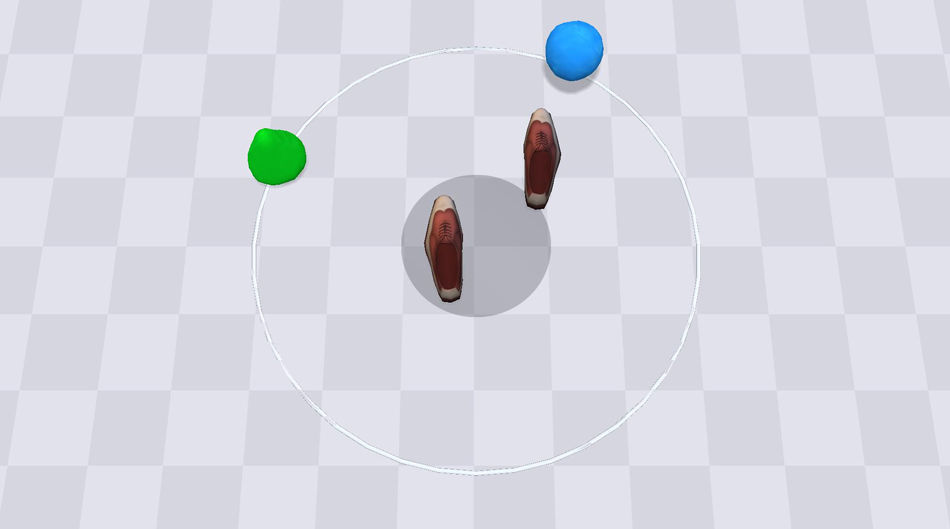
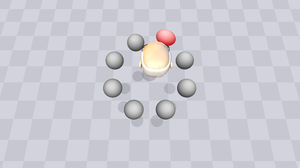
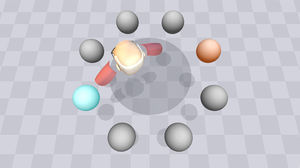
Balance rehabilitation by means of reaching tasks in BioTrak places the patient in a 3D virtual reality setting where he/she performs a series of movements in order to reach virtual items appearing nearby. The exercise offers a third-person view, which enables the subject to accurately identify his/her position and movements. In order to facilitate task comprehension and enhance the sensation of being in a virtual world, the setting and the avatar are simple and intuitive, even for patients with underlying cognitive problems. This module includes different increasingly complex exercises that can be performed in 2 positions: sitting (Figs. 1–3) and standing (Fig. 4). Sitting exercises are used for controlling the head and trunk, whereas standing exercises improve static and dynamic balance, postural control, and weight shifting tasks. All exercises are designed in line with the principles of motor learning. They are repetitive, intensive, motivating, adjustable with regard to difficulty, and orientated to specific tasks.
The system software allows therapists to personalise training sessions by selecting different exercises and programming their duration, resting time, and number of repetitions. Likewise, the difficulty of each exercise may be adjusted by using a series of parameters, such as distance at which virtual items appear, time they remain visible, their size, their location compared to that of the subject, and the number of other virtual items in the setting at the same time. In order to facilitate and streamline daily sessions, the therapist may recur to the system's predefined and adjustable series of levels of difficulty.
ProcedureAll patients included in this study received between 3 and 5 one-hour sessions per week of combined conventional physiotherapy and BioTrak training. The treatment protocol for BioTrak included a total of 20 sessions, 20minutes long, consisting of 3 six-minute exercises, with 2-minute breaks between exercises.
Sessions were completed in an equipped area of the gymnasium under the supervision of the lead physiotherapist. On the first day of treatment, all included patients were informed about the exercise dynamic, watched an exercise demonstration, and completed a training session in order to become acquainted with the use of the device. During the initial session, participants started at the lowest level of difficulty. Levels of difficulty were increased in subsequent sessions according to patients’ results. Adjustments were made by either the therapist or the system itself, which automatically increases the level of difficulty each time the patient successfully finishes the exercise with an error rate ≤2%.
Assessment protocolAll patients were studied using the assessment protocol described in the following section at the beginning (Vi) and the end of Biotrak programme (Vf), and one month after treatment (Vf+1m). During that last month, patients continued with conventional physiotherapy.
The assessment protocol for the Biotrak balance module for standing and reaching included the Berg Balance Scale (BBS)30 and the Tinetti Performance-Oriented Mobility Assessment (POMA),31 which measure the static and dynamic balance as an individual completes different functional movements. Likewise, all patients were assessed using a NEDSVE/IBV dynamometric platform.32 This device combines static posturography assessment with dynamic tests and provides a global index evaluating the patient's balance. The dynamometric platform has 4 strain gauge sensors that allow researchers to analyse the action–reaction forces by transforming them into electric signals. The system lets researchers quantify the limits of the patient's stability and offers 3 sensory indexes (visual, proprioceptive, and vestibular) which provide information about the effect of each of these systems on the subject's balance. The posturography system records a variable corresponding to rhythmic weight shift, which quantifies the patient's ability to move his/her centre of gravity laterally (medial–lateral control) and from front to back (anterior–posterior control). All system indexes are shown as percentages (%); results other than 100% reflect discrepancies with respect to normal values from a normative group adjusted for the patient's age and height. According to system specifications, a discrepancy of 5% is permitted with respect to normative group values as the normal value threshold. A discrepancy of 15% is permitted for the stability limits and rhythmic and directional control. Therefore, the lower the value of each index, the greater the degree of impairment. The balance study was performed without any type of assistance in all cases.
All patients completed a usability questionnaire at the end of the treatment protocol, in order to record their subjective impressions of the virtual experience. The questionnaire included 8 questions scored on a scale of 1 to 5. This ad hoc questionnaire was prepared based on the Short Feedback Questionnaire (SFQ)33 model and adapted to the characteristics of the system. The first 6 questions referred to the interest level, the feeling of being part of the setting (presence), the perception of the setting as real (immersion), the perception of success (feedback) and control over the situation, and overall understanding of the feedback generated by the system. The 7th question examined the degree of comfort during the virtual experience, as well as any potential adverse effects (dizziness, disorientation, eye discomfort, etc.). The 8th question analysed the perceived difficulty of completing the task and using the hardware. Scores for each question were adjusted so that high total scores would reflect a greater degree of usability and a lower number of adverse effects.
Statistical analysisQuantitative variables were measured using descriptive statistics (mean+SD), whereas qualitative measurements were analysed using frequency distributions. We used repeated measures ANOVA (time effect) with a post hoc analysis (Bonferroni) to compare the 3 evaluation times (Vi, Vf, and Vf+1) to determine whether significant differences were present between the study variables at those times. All statistical analyses were carried out using SPSS software, version 15 for Mac (SPSS Inc., Chicago, USA).
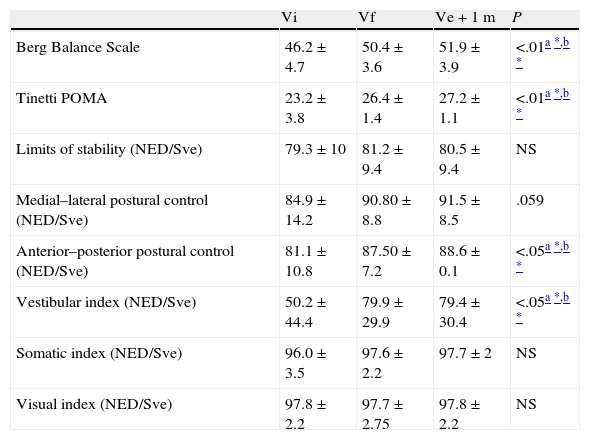
ResultsLongitudinal analysisTable 2 shows the means±standard deviations of the motor scales (BBS and POMA) and the parameters obtained from dynamic posturography corresponding to Vi, Vf, and Vf+1 month. Repeated measures ANOVA for time effect analysis showed a significant improvement in scores on both the BBS (P<.01) and the POMA (P<.01). Likewise, the parameters obtained from posturography analysis demonstrated significant improvements on the vestibular index (P<.05) and in anterior–posterior control (P<.05), and a tendency towards statistical significance in medial–lateral control (P=.059) The post hoc analysis revealed significant improvements between Vi and Vf on the BBS, the POMA, and anterior–posterior control. These benefits remained present 1 month after completing the BioTrak protocol. We observed no statistically significant improvements in any of the study variables when comparing Vf and Vf+1m scores.
Changes in clinical and posturographic variables (repeated measure ANOVA with Bonferroni correction) between initial and final BioTrak training sessions and 1 month after the final session.
| Vi | Vf | Ve+1m | P | |
| Berg Balance Scale | 46.2±4.7 | 50.4±3.6 | 51.9±3.9 | <.01a*,b* |
| Tinetti POMA | 23.2±3.8 | 26.4±1.4 | 27.2±1.1 | <.01a*,b* |
| Limits of stability (NED/Sve) | 79.3±10 | 81.2±9.4 | 80.5±9.4 | NS |
| Medial–lateral postural control (NED/Sve) | 84.9±14.2 | 90.80±8.8 | 91.5±8.5 | .059 |
| Anterior–posterior postural control (NED/Sve) | 81.1±10.8 | 87.50±7.2 | 88.6±0.1 | <.05a*,b* |
| Vestibular index (NED/Sve) | 50.2±44.4 | 79.9±29.9 | 79.4±30.4 | <.05a*,b* |
| Somatic index (NED/Sve) | 96.0±3.5 | 97.6±2.2 | 97.7±2 | NS |
| Visual index (NED/Sve) | 97.8±2.2 | 97.7±2.75 | 97.8±2.2 | NS |
NS: not significant; Vi: initial evaluation; Vf: final evaluation; Vf+1m: evaluation 1 month after end of treatment.
On a clinical level, 3 of the 4 patients who required support for safe walking indoors at the beginning of the treatment (quadruple cane tip) could walk unaided.
UsabilityAccording to the scores from the usability questionnaire, patients described the experience as pleasant (3.7±0.9), felt ‘present’ during the virtual experience (4.1±0.8), and perceived the setting as realistic (3.7±1.1). In addition, participants showed good understanding of the feedback provided by the system (4.4±0.9) and a good level of control over the situation (3.63±0.84). In general, they described their performance as successful (3.7±0.8) and they did not experience serious difficulties in completing tasks (3.5±1) or using the device (4±1). None of the participants experienced adverse effects (eye discomfort, dizziness, nausea, etc.) while completing the virtual tasks.
DiscussionAccording to our results, BioTrak is an effective and user-friendly tool for balance rehabilitation in patients with ABI. The system's clinical effectiveness is supported by the fact that most patients included in the standing-reaching balance rehabilitation module improved their scores on the motor scales used in this study. Likewise, the posturography study showed improvements in dynamic postural control mechanisms and in the vestibular system, which is responsible for maintaining balance. In addition, if patients continue with a traditional rehabilitation programme, the improvements observed at the end of this virtual programme seem to endure over time.
Balance and postural control disorders are some of the most common and functionally limiting deficits occurring after an ABI.34 These problems may persist for years and have a significant impact on the patient's quality of life.4 Although in recent years we have begun to have access to different VR programmes focusing on the recovery of motor abilities lost after brain injury, there are few studies at present that show those programmes to be effective for balance rehabilitation.13–15,17 Additionally, the results obtained from these systems are unlikely to be applicable to the overall population due to the small sample size and the limitations of the studies’ experimental design. In the same way, any interpretation of the results from our study should consider the specific characteristics of our sample and the lack of a control group. Nevertheless, the improvements resulting from treatment with BioTrak, and the continued presence of those improvements a month after ending treatment, confirm the benefits of this type of system. The clinical relevance of these results is even greater when we consider post-stroke times in our sample. In fact, the mean increases in both the BBS and POMA scores are slightly lower than the minimum detectable changes published for these scales in patients with acute-phase neurological disease and in samples of healthy subjects.35–37
Treatment with BioTrak also yielded obvious improvement in scores from the posturography analysis, which is consistent with patients’ clinical improvement. The initial analysis showed the pattern classically described in hemiparetic patients: clear decrease in the stability limits mainly affecting the paretic side, a decrease in the information provided by the vestibular afferents caused by an increased burden on visual afferents, and an overall decrease in rhythmic and directional control scores.38,39 BioTrak was able to improve the vestibular index and the rhythmic control scores; the latter reached the lower range of the normal level. The lack of detectable improvement in the stability limits may be related to specificity of the training task and the fact that it is similar to rhythmic control exercises and not to weight shift exercises without reaching tasks.
Very few studies have been dedicated to the neurophysiological basis underlying clinical improvements observed with some such training programmes, and even fewer investigate the changes in brain plasticity these programmes foster in patients with an acquired lesion. Researchers recently described a sensorimotor cortex reorganisation phenomenon coinciding with the clinical improvements detected in a sample of stroke patients who had completed a virtual reality motor rehabilitation programme.40 Recent studies on motor recovery following brain injury highlight the importance of a series of basic learning principles that guarantee maximum therapeutic efficacy for any technique.5 BioTrak complies with all of these basic motor learning principles, and delivers early and intensive therapy adapted to the patient's needs. Given that several studies highlight the functional advantage of task-specific motor training,41,42 BioTrak is currently including a ‘natural’ setting in which the patient can perform tasks similar to those occurring in daily life. As a result, acquired motor improvements will benefit patients in their day-to-day activities.
BioTrak combines the benefits of other balance training systems using cutting-edge technologies, including feedback posturography,43 and the use of virtual reality-based strategies employed in gaming consoles, such as the Wii Balance Board.22,23 Biotrak's versatility and the specificity of both its design and content are additional advantages. Based on the above, BioTrak covers the full spectrum of balance rehabilitation activities, from the initial recovery phases that focus on postural control over the head and trunk in a seated position, to more advanced phases in which patients perform standing dynamic balance exercises that involve simultaneous management of several items. BioTrak allows the therapist to personalise sessions for each patient (intensity/difficulty levels, type of task, resting, working time, etc.) according to their needs and abilities in each phase of rehabilitation. The system's design, unlike that of entertainment systems with non-clinical software (game consoles), also enables easy interaction between the patient, system, and therapist. An added benefit is that BioTrak provides a highly motivating activity according to the results from the usability study. None of the subjects in our study reported adverse effects, and all described BioTrak as tool that increases the subject's active participation during the recovery process. In addition, contrary to other more complex systems, BioTrak is a low-cost tool that can easily be used in any clinical setting due to its versatile tracking system. It also achieves levels of presence and immersion similar to those of other devices that are much more invasive.
For future lines of research, it may be advisable to increase the sample size and include a control group in order to check system efficacy by comparing it with conventional rehabilitation. Our results provide clinical evidence of the benefits perceived by patients with balance problems due to an ABI after an intensive one-month training programme with BioTrak. It is an effective, reliable, clinically useful, low-cost tool that follows the principles of motor learning and covers the full spectrum of balance rehabilitation exercises for patients with ABI.
FundingThe current study received funding from the Spanish Centre for the Development of Industrial Technology (TEREHA project, IDI-20110844) and partial funding from the Spanish Ministry of Education and Science, Project Game teen (TIN2010-20187), Project Consolider-C (SEJ2006-14301/PSIC), CIBER de Fisiopatología de la Obesidad y Nutrición (an ISCIII initiative), and the PROMETEO Programme for Excellence (Valencian Regional Government, Council for Education, 2008-157).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Lloréns R, et al. BioTrak: análisis de efectividad y satisfacción de un sistema de realidad virtual para la rehabilitación del equilibrio en pacientes con daño cerebral. Neurología. 2013;28:268–75.