Headache is a common cause of medical consultations. We aim to analyse demographic characteristics of the first 2000 patients in our register, and the incidence of their different headaches coded according to the International Classification of Headache Disorders, second edition (ICHD-II)
Patients and methodsIn January 2008, a headache outpatient clinic was established in a tertiary hospital. Patients could be referred by general practitioners according to criteria established by prior consensus, as well as by general neurology or other specialty clinics. The following variables were prospectively collected for all patients; age, sex, referral source, complementary tests required, and the previously prescribed symptomatic or prophylactic therapies. All headaches were classified according to ICHD-II. When a patient fulfilled criteria for more than one type of headache, all of them were diagnosed and classified.
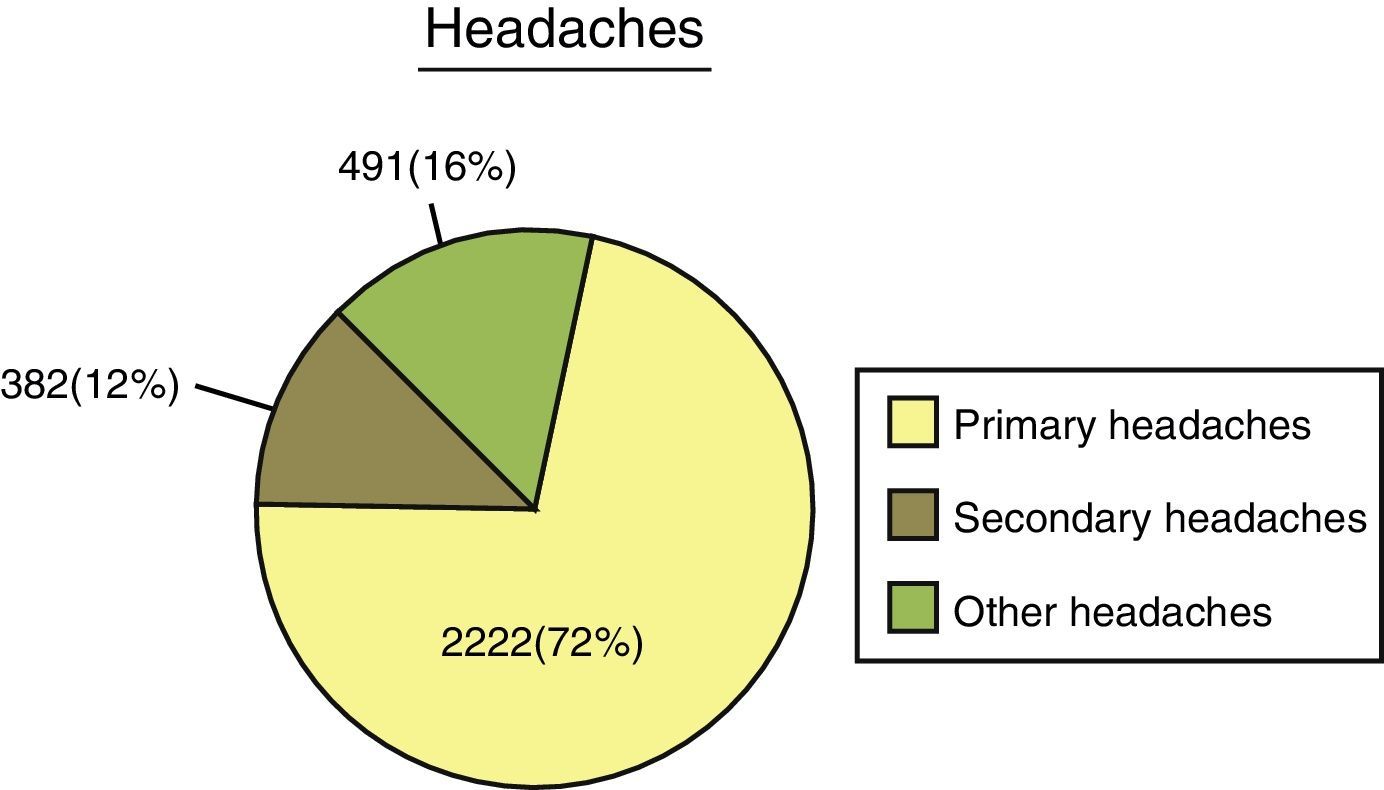
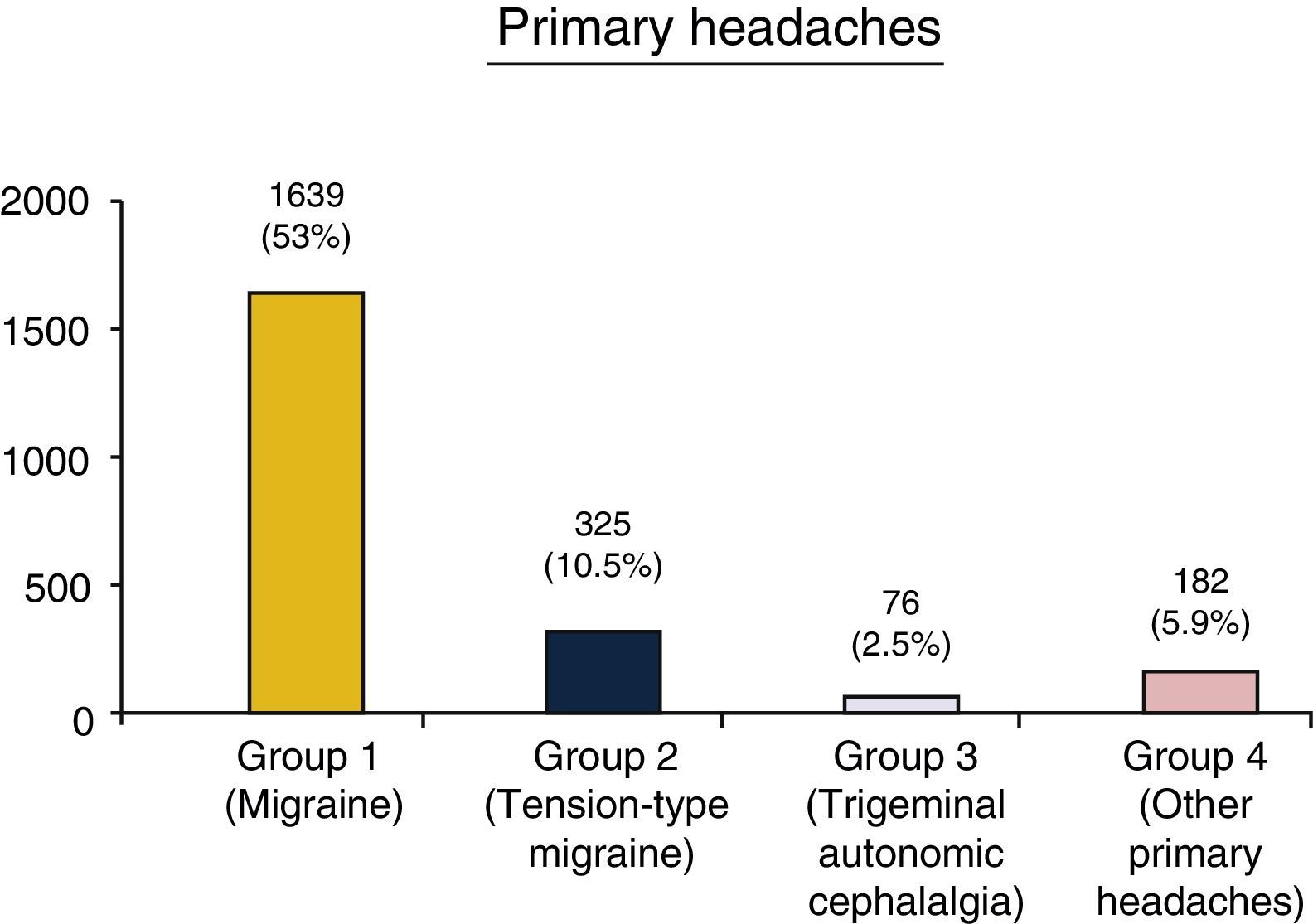
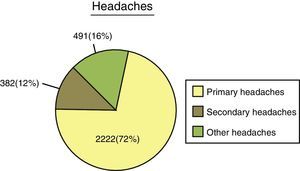
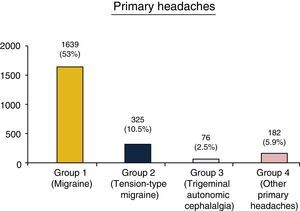
ResultsIn October 2012, 2000 patients (ratio women/men 2.59/1) had been seen in our headache clinic. The median age was 42 years (range, 11-94), 55.3% were referred from primary care, and 68.1% did not require complementary tests. A total of 3095 headaches were recorded in these 2000 patients, of which 2222 (71.8%) were considered primary headaches, 382 (12.3%) secondary headaches including 117 (3.8%) corresponding to cranial neuralgias, 136 (4.3%) were unclassified headaches, and 238 (7.7%) were included in the Appendix to the ICHD-II. The most represented group was group 1 (migraine) accounting for 53% of all headaches.
ConclusionsThe characteristics of the first 2000 patients in our register were comparable to those previously described in other types of outpatient headache clinics. Migraine was the most frequent diagnosis, and secondary headaches were not as frequent in our series. Most headaches could be coded according to ICHD-II criteria.
Analizar las características demográficas de los 2.000 primeros pacientes del registro de una consulta monográfica de cefaleas (CMC), y la incidencia de los diferentes tipos de cefaleas codificadas según los criterios de la clasificación internacional de cefaleas, ii edición (CIC-II)
Pacientes y métodosEn enero de 2008 se estableció una CMC en un hospital terciario. Los pacientes podían ser derivados desde atención primaria en formato de alta resolución, la consulta general de neurología u otras especialidades. Se atendieron fuera de agenda a profesionales del centro o familiares. Recogimos prospectivamente en cada paciente la edad, el sexo, la vía de acceso a la consulta y los tratamientos sintomáticos o profilácticos prescritos con anterioridad. Las cefaleas fueron clasificadas de acuerdo a la CIC-II; cuando un paciente cumplía criterios para más de un tipo de cefalea todas eran diagnosticadas y clasificadas.
ResultadosEn octubre de 2012 2.000 pacientes (ratio mujeres/hombres: 2,59/1) habían sido incluidos. La mediana de edad de estos pacientes era de 42 años (rango: 11-94). El 55,3% fueron derivados desde atención primaria. Un 68,1% no requirió pruebas complementarias. Se codificaron 3.095 cefaleas; 2.222 (71,8%) primarias y 382 (12,3%) secundarias. Ciento diecisiete (3,8%) neuralgias craneales, 136 (4,3%) no clasificables y 238 (7,7%) incluidas en el apéndice de investigación de la CIC-II. El grupo más representado era el 1 (migraña) con un 53% del total de cefaleas.
ConclusionesLas características de nuestro registro son comparables a las descritas previamente en consultas monográficas de cefaleas. La migraña fue el diagnostico más habitual. Las cefaleas secundarias no son frecuentes en nuestra serie. La mayoría de las cefaleas pudieron ser codificadas por la CIC-II.
Headache is the most frequent reason for neurological consultation and one of the most common for primary care consultations. Even so, epidemiological studies show that a significant percentage of people experiencing headache never seek medical advice.1–3
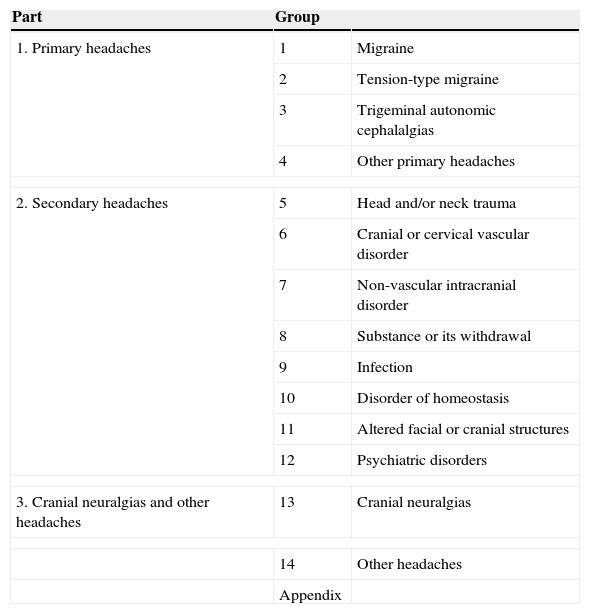
Headache can have a significant impact on the patients’ quality of life, leading to high direct and indirect financial costs.1,4 The second edition of the International Classification of Headache Disorders (ICHD-II)5 helps doctors assign the appropriate diagnosis for each patient, which is essential for managing headache patients correctly. This classification includes 14 groups divided into 3 sections plus an appendix (Table 1).
International Classification of Headache Disorders, second edition
| Part | Group | |
|---|---|---|
| 1. Primary headaches | 1 | Migraine |
| 2 | Tension-type migraine | |
| 3 | Trigeminal autonomic cephalalgias | |
| 4 | Other primary headaches | |
| 2. Secondary headaches | 5 | Head and/or neck trauma |
| 6 | Cranial or cervical vascular disorder | |
| 7 | Non-vascular intracranial disorder | |
| 8 | Substance or its withdrawal | |
| 9 | Infection | |
| 10 | Disorder of homeostasis | |
| 11 | Altered facial or cranial structures | |
| 12 | Psychiatric disorders | |
| 3. Cranial neuralgias and other headaches | 13 | Cranial neuralgias |
| 14 | Other headaches | |
| Appendix | ||
The aim of our study is to analyse the demographic characteristics of the first 2000 patients registered in a specialist headache clinic (SHC) and the incidence of their different headache types classified according to ICHD-II criteria.
Patients and methodsThe SHC was set up in our tertiary hospital in January 2008. Following a one-stop clinic model, patients could be referred by primary care according to previously agreed and established criteria. The clinic also accepts referrals from the general neurology department in especially complex cases or those needing interventions with therapeutic instruments (anaesthetic blocks or botulinum toxin injections), as well as in-hospital referrals by other medical specialities. After being made aware that the new SHC was operational, hospital employees immediately requested appointments for themselves, family members, and friends.
We prospectively registered SHC patients’ demographic characteristics, referring department, complementary tests ordered by the neurologist in charge of the SHC (A.L.G.), and symptomatic and preventive treatments applied before the patient was seen at the SHC.
All headaches were coded according to ICHD-II criteria. When a patient met criteria for more than one headache type, all types were diagnosed and coded.
ResultsAs of October 2012, 2000 patients (1444 women and 556 men with a ratio of 2.59:1) had been attended in the SHC. Mean age in our series at the time of first consultation in the SHC was 42 years (range 11-94). Most of our patients (1105, 55.3%) were referred by primary care. Five hundred and two (25.1%) were referred to the SHC by the general neurology department and 232 (11.6%) by other specialities, mainly neurosurgery. One hundred and sixty-one (8.1%) of the cases were the patients with staff connections that we mentioned before.
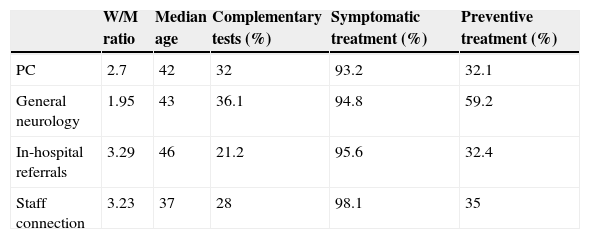
No additional tests were considered necessary in 1367 patients (68.1%). Previous symptomatic treatment was reported for 94.3% of the patients while only 37.5% had received some kind of prophylactic treatment. Table 2 shows a comparison for these variables among the 4 groups of patients classified by route of referral. The most interesting discovery, although one that might be expected in this analysis, is that highest rate of previous preventive treatment was recorded for patients referred by the general neurology department.
Comparison of the different variables according to referral source
| W/M ratio | Median age | Complementary tests (%) | Symptomatic treatment (%) | Preventive treatment (%) | |
|---|---|---|---|---|---|
| PC | 2.7 | 42 | 32 | 93.2 | 32.1 |
| General neurology | 1.95 | 43 | 36.1 | 94.8 | 59.2 |
| In-hospital referrals | 3.29 | 46 | 21.2 | 95.6 | 32.4 |
| Staff connection | 3.23 | 37 | 28 | 98.1 | 35 |
PC: primary care; W: woman; M: man.
These 2000 patients were diagnosed with 3095 headaches; 2222 (71.8%) were classified as primary headaches (groups 1 to 4 of the ICHD-II), and 382 as secondary headaches (groups 5 to 12) (Fig. 1). One hundred and seventeen (3.8%) were classified as cranial neuralgias (group 13), 136 were considered unclassifiable (group 14), and 238 (7.7%) were included in the ICHD-II appendix.
Regarding primary headaches, 1639 or 53% of the total were included in group 1 (migraine). A total of 325 (10.5%) were classified as group 2 (tension-type headache), 76 (2.5%) as group 3 (trigeminal autonomic cephalalgias), and 182 (5.9%) as group 4 (other primary headaches) (Fig. 2).
Incidence of secondary headaches was low in our series. We can highlight the 31 headaches (1% of the total) included in group 5, headache attributed to head and/or neck trauma; and the 306 headaches (9.9%) included in group 8, headache attributed to substance or its withdrawal. Fewer headaches were included in group 6 (headache attributed to cranial or cervical vascular disorder, 10 cases, 0.3%), group 10 (headache attributed to disorder of homeostasis, 2 cases, 0.1%), and group 11 (headache or facial pain attributed to facial or cranial structures, 16 cases, 0.6%).
DiscussionHeadache is an important healthcare problem which affects all age groups, from children to adults. Ninety percent of the population has experienced a headache at one time or another.6 According to the literature, the overall prevalence of headache is approximately 50%,7–11 with the highest incidence in middle-aged individuals.
Quality of life of these patients is considerably decreased, depending on the number of episodes and their frequency and intensity. Both direct and indirect costs of migraine are significant in Spain and other European countries.12 Headaches also have an impact on family and social relationships and result in school and work absenteeism.4,13,14 The Global Burden of Disease Study 2010, published by WHO,15 indicates that the 2 main primary headaches, tension-type headache and migraine, are the second and the third most prevalent diseases in the world. Furthermore, migraine, the most incapacitating type of headache, is ranked seventh out of all disease-related causes of disability worldwide.16
Therefore, designing headache care systems appropriately6,17 is essential for achieving early and accurate diagnoses that let doctors select an appropriate treatment for each case, thus minimising the impact of headache.4
Demographic characteristics in our series (with a female-to-male ratio of 2.5:1 and median ages in the fifth decade) are comparable with those reported by other hospital-based studies.18–21
The route of referral could be one of the factors explaining the differences in the results from the various specialist clinics or headache units.22,23 Our SHC was designed following a mixed model based mainly on cooperation with primary care. Cases of special complexity were also referred to the SHC by the general neurology department and other departments. The comparison in Table 2 shows that patients’ demographic characteristics are similar, regardless of their route of referral. As one might expect, the percentage of patients who had already received preventive treatment was higher among those referred by neurology clinics. In any case, our primary care doctors use preventive therapies more frequently than was previously described by studies conducted in general neurology clinics in Spain.24 This may be due to the continuing education initiative that was launched at the same time as the SHC was established.
The extent to which patients with connections affect overall care has received little study, except in summaries of typical risks in that situation,25 and articles on VIP management.26 Given the high prevalence of headaches and the age of our hospital staff, we surmised that many of our co-workers would request care in our SHC, whether for themselves or for close relatives, ever since the unit was launched. As we are aware of this increased patient volume, we verified whether these patients would in any case have been referred to our SHC by primary care. This is indeed the case: 81.5% of our patients with connections would have met the referral criteria proposed for primary care. This indicates that our staff acted responsibly, without engaging in undue consumption of the resources to which they enjoy easy access.
The percentage of patients for whom additional tests and procedures were ordered by our SHC was slightly higher than 30%. We should highlight that patients referred by the general neurology department or other departments had frequently undergone a prior neuroimaging scan (primary care doctors cannot request neuroimaging scans in our system). Also, according to the established referral protocol, analytical studies including erythrocyte sedimentation rate (ESR) are performed in cases of new onset of headache in patients older than 50. The message we would like to convey to primary care doctors is that the percentage of significant intracranial lesions in headache patients is very low, and this rate is even lower in cases with normal neurological examination results.27
Since the ICHD-II establishes that all headache types must be diagnosed in patients presenting multiple types of headache,5 it is not surprising that we coded 3095 headaches in 2000 patients. This combination of diagnoses has been observed in other studies conducted in healthcare models similar to our own.28
Although tension-type headache accounts for the largest percentage of total headaches in population-based studies, studies conducted in primary care28 and in general neurology clinics29 show higher rates for migraine.
Migraine is the most frequently assigned diagnosis in our series, which is in line with most studies conducted in specialist clinics or headache units.19,20,30–32 The reason for the high prevalence of tension-type headache in population-based studies, and its tendency to decrease at more specialised levels of care, is probably that headache has a lower impact on these patients, and many will not seek medical attention.7–11,14,33 Even so, the percentage of tension-type headache is lower in our series than in previous studies in similar healthcare models. The generalisation of the concept of chronic migraine, assuming this to be the diagnosis of a patient with daily, or almost daily, dull pain with frequent migraine attacks, leads doctors to stop contemplating the possible diagnosis of tension-type headache associated with migraine in this type of patients.34,35
Lastly, regarding primary headaches, presence of group 3 (trigeminal autonomic cephalalgia), and group 4 (other primary headaches) in our series is comparable with rates previously described in this type of headache unit.31,32,36 Incidence of secondary headache is low in our series, as in previous studies.8,18–20 Most headaches were included in group 8, i.e. headache attributed to substance or its withdrawal, a very well-known entity in our setting.37
Nearly 4% of our patients’ headaches corresponded to cranial neuralgias and more than 7% were proposed entities included in the ICHD-II appendix. Lastly, just over 4% of the headaches were included in group 14 (unspecified or unclassifiable headaches).
In conclusion, characteristics of the first 2000 patients from a register kept by a specialised headache clinic are comparable with those previously described in this type of healthcare model. The percentage of secondary headaches is low, with the exception of headaches attributed to medication overuse, and the most common entity is migraine. Most headaches in our patients could be coded according to ICHD-II criteria.
FundingThis study has received no funding of any kind.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Pedraza MI, Mulero P, Ruíz M, de la Cruz C, Herrero S, Guerrero AL. Características de los 2.000 primeros pacientes registrados en una consulta monográfica de cefaleas. Neurología. 2015;30:208–213.
Partially presented in poster format at the 23rd Congress of the European Neurological Society, Barcelona, June 2013.