The development of endovascular techniques has put Interventional Neuroradiology (INR) as the first-option treatment in the majority of vascular diseases of the central nervous system. Scientific societies in developed countries have created standard procedures for training and accreditation for a safe practice in these procedures.
DiscussionIn Spain, we are waiting for the development of the legislation on the accreditation for specialists which will establish the official formative model to achieve an accreditation in INR. Until this moment comes, it is necessary to establish standards that define desirable minimums for the formative period in INR. Radiology specialists as well as neurologists and neurosurgeons will have access to INR accreditation. Specific requirements for the hospitals that wish to offer this technique and training should also be defined.
ConclusionThe Spanish Group of Interventional Neuroradiology, the Spanish Society of Neuroradiology, the Spanish Group of Cerebrovascular Diseases, the Spanish Society of Neurology and the Spanish Society of Neurosurgery have approved the content of this document and will create a committee in order to put into practice the accreditation of formative centres and INR specialists.
El desarrollo de las técnicas endovasculares ha colocado a la Neurorradiología Intervencionista-Neurointervencionismo (NRI-NI) como una alternativa de primera elección para el tratamiento de gran parte de las enfermedades vasculares del sistema nervioso central. Al no disponer de programas formativos en NRI-NI normalizados, las sociedades científicas de los países desarrollados han creado estándares de formación y acreditación para la práctica segura de estos procedimientos.
DesarrolloEn España, estamos a la espera del desarrollo legislativo de las Áreas de Capacitación Específicas que establecerán el modelo formativo oficial para los especialistas que deseen formarse en NRI-NI. Hasta que llegue ese momento, se hace pertinente disponer de unos estándares que definan los mínimos deseables para el periodo formativo en NRI-NI al que puedan acceder especialistas no solo de la Radiología, sino también de la Neurocirugía, y la Neurología, así como los requisitos exigibles a los hospitales que realizan esta actividad y quieran impartir dicha formación.
ConclusionesPara poner en práctica la acreditación de centros formativos y la acreditación de los centros formadores y especialistas formados en NRI-NI, el Grupo Español de Neurorradiología Intervencionista (GENI), la Sociedad Española de Neurorradiología (SENR), el Grupo de Estudio de Enfermedades Cerebrovasculares (GEECV) de la Sociedad Española de Neurología (SEN) y el grupo experto en enfermedades vasculares de la Sociedad Española de Neurocirugía (SENEC), han aprobado el contenido de este documento de consenso y crearán un comité acreditador.
The term ‘Interventional Neuroradiology-Neurointervention’ (INR-NI) describes the array of diagnostic and therapeutic activities that have been developed in neurology and radiology for use in certain diseases affecting the nervous system, its meningeal and osteoarticular layers, and the cervicofacial region.
Well-developed INR-NI activities include endovascular techniques, which are now widely recognised for use in diagnosis and treatment of vascular diseases of the central nervous system.1–3
The advancement of endovascular techniques in the past 30 years has elevated INR-NI to the first choice treatment alternative for a long list of vascular diseases affecting the central nervous system.
In addition to endovascular techniques, INR-NI has developed percutaneous techniques for use in diagnosing and treating certain diseases in the craniocervical area and spinal column.
Given the lack of standardised INR-NI training programmes, medical societies in developed countries have been elaborating training and accreditation frameworks to certify professionals to practise these procedures. Minimum requirements for the length of training programmes, the theoretical and practical content of the programmes, and the requirements for hospitals intending to provide training have been established both in Europe4 and in the United States.5 There are more than 50 hospitals with INR-NI training programmes in the United States that demonstrate the interest by neuroradiologists, neurosurgeons, and neurologist in acquiring these techniques.6 These training activities and their results were analysed recently.7,8
In Spain, law 44/2003 for the regulation of health professions9 provides for the establishment of specific areas of accreditation (SAA); once these areas have been established legally, they will provide the frameworks for post-specialty medical training programmes with content pertinent to one or more specialties.
In 2007, the Spanish Group of Interventional Neuroradiology (GENI) and the Spanish Society of Neuroradiology (SENR) proposed the creation of an SAA for Interventional Neuroradiology (INR) and submitted the application to the Spanish Ministry of Health by means of the National Committee on Radiodiagnostics, and with the approval of the National Committees on Neurosurgery and Neurology (Fig. 1).
Regulations pursuant to that Royal Decree and regulating specialised healthcare training by establishing core curriculum and by creating and expanding SAAs are still being drafted. The perspective of the neurological sciences is that, since SAAs have not yet been implemented legally, it would be prudent to define guidelines spelling out the minimum requirements for an INR-NI training programme that would be open to neurosurgeons and neurologists as well as to radiologists. These guidelines would also list requirements applicable to the hospitals performing INR-NI techniques and intending to offer the training programme.
Individuals and hospitals will be able to obtain INR-NI accreditation based on these standards, which are endorsed by the GENI and the SENR and reflect the ability of these pertinent medical societies to provide specialist training. The accreditation programme proposed here is intended not as a means to an official diploma, but as a more or less temporary stopgap measure to meet the need for objective certification of training.
The reality is that modern healthcare requires guidelines indicating the minimum standards that must be implemented to guarantee better quality care with less variability in clinical practice.
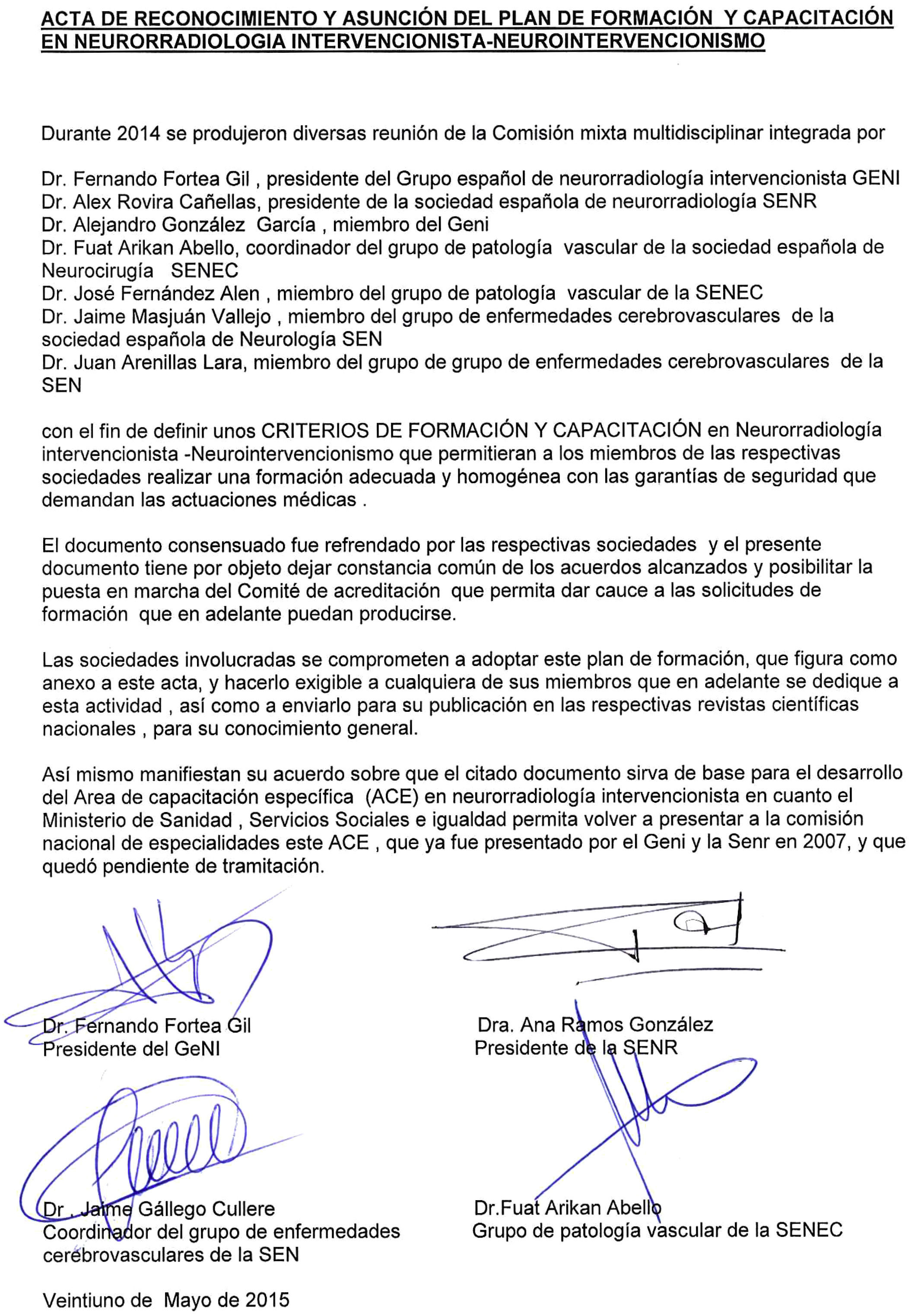
In order to provide a means of accrediting INR-NI capability for teaching centres and specialists alike, the medical societies endorsing this consensus statement will formally approve its content in writing. They will also create an accrediting body whose composition and functions are specified in Appendix 1.
Requirements for a healthcare training setting- 1.
Training in INR-NI involves gaining proficiency in percutaneous and/or endovascular access techniques that can be used to treat certain diseases of the central nervous system, bulbospinal territory, and head and neck. This training is intended to complement pre-existing knowledge and abilities in neuroradiologists, neurosurgeons, and neurologists wishing either to acquire such competencies or certify and accredit them if they have already been acquired.
- 2.
Training programmes must ensure trainees’ knowledge of the diseases that may be diagnosed or treated using percutaneous or endovascular access techniques, and they must follow a single syllabus that specialists will be required to complete in full.
- 3.
Once the training activities have been completed, the accredited specialist must be able to perform, as a member of an INR team, the procedures pertaining to this area of knowledge.
- 4.
A new INR-NI team will include, at the very least, a specialist with accredited INR-NI training and more than 5 years of experience, a licensed nurse experienced in setting up for INR-NI techniques, and an available anaesthesiology/reanimation specialist. During procedures, the team will also require a second licensed nurse to provide specific tools and to support the anaesthetist.
- 5.
The hospitals aiming to provide INR-NI training must be accredited to provide specialist training in the fields of radiology, neurosurgery, and neurology; they must also have the resources and clinical activity specified in Appendix 2.
The training programme must last a minimum of 2 years and may be extended to 3 years at the most for candidates with deficiencies in their prior training. It must also be presented in a hospital accredited for training residents (MIR).
The training programme must provide the theoretical basis and the clinical experience necessary to address the full array of clinical knowledge in INR-NI. Before the trainee may assume the responsibility of performing a neurointerventional procedure, he or she must acquire or certify a foundation of clinical and neuroradiological knowledge.
Candidates must have completed their residency cycle (MIR) in a related area: radiology, neurosurgery, or neurology.
- a.
Itinerary for candidates trained in radiology:
- •
Candidates without 9 months of previous training in neuroradiology must complete that training in full, including imaging techniques (MRI, CT) and invasive diagnostic tests, until they are certified as having performed a minimum of 100 diagnostic cerebral angiographies.
- •
They will spend a total of 6 months on rotation in the neurology department, with a special emphasis on the stroke, neurosurgery, and intensive care units.
- •
In any case, they must complete a minimum of 18 months of advanced specific training in INR-NI techniques.
- •
- b.
Itinerary for candidates trained in neurosurgery or neurology:
- •
During the programme, candidates will complete training in diagnostic neuroradiology in an accredited unit (minimum of 9 months). This will include a grounding in the physical basis, use, and biological effects of ionising radiation. Candidates must also accredit having performed a minimum of 100 diagnostic cerebral angiographies. Where applicable, they may accredit any training in these areas that they may have completed during their residencies.
- •
Candidates must necessarily complete a minimum of 18 months of advanced specialist training in INR-NI techniques.
- •
In all cases, the INR-NI programme will require candidates to complete specific hands-on training in which the specialist will participate actively in no fewer than 100 therapeutic procedures during the programme. Candidates must certify having performed the following (numbers are approximate):
- •
25 endovascular procedures to treat cerebral aneurysms
- •
15 endovascular procedures to treat cerebrovascular malformations
- •
15 extracranial artery angioplasties with stent placement
- •
10 cases of endovascular treatment for acute stroke
- •
15 miscellaneous (e.g. intracranial angioplasty due to stenosis or vasospasm, correction of vascular malformations of the external carotid or venous vascular malformations, tumour embolisation, etc.)
- •
5 bulbospinal endovascular procedures (spinal dural arteriovenous fistula, spinal arteriovenous malformation, etc.)
- •
15 spine interventional procedures (vertebroplasty; kyphoplasty; discolysis; paravertebral, periradicular, or periganglionar infiltrations; biopsies; etc.)
If a candidate is unable to complete the full training programme at a single hospital, he or she may use external rotations to meet the entire list of requirements.
Conflict of interestNo conflict of interest.
The committee is made up of 5 members:
- •
The president (or delegate) of the GENI
- •
The president (or delegate) of the SENR
- •
Member of the GENI designated by its Steering Committee
- •
Coordinator (or delegate) of the Spanish Society of Neurosurgery vascular disease study group
- •
Coordinator (or delegate) of the Spanish Society of Neurology cerebrovascular disease study group
The duration of these appointments to the Committee shall depend on the duration of members’ positions in their respective medical societies.
Establishment, functions, and activities:
The committee shall be constituted at such time as its founding document is signed by the societies involved.
A secretary/spokesperson shall be chosen from among the members of the committee.
Applications for training centre accreditation will be submitted by the parties responsible for INR-NI units to the secretary of the committee.
The secretary will then use the data recorded in the Spanish INR-NI register (RENIN, www.neurointervencionismo.es) to validate the hospital's proposal before notifying the rest of the committee members to proceed to confirm that validation. The process will be halted if members find contradictory data in databases pertaining to other medical societies.
Applications for certifying specialists who have completed a training programme will be submitted by accredited training centres to the committee secretary.
Decisions regarding accreditation will depend on a majority vote.
Meetings may be held in person or by means of other forms of communication agreed on by the members.
Every year, the committee will establish the number of training programme openings for the coming year, based on the need for new professionals as measured by RENIN.
The committee will review applications received no later than 31 December for the training programmes presented in the same year; it will then have a maximum of 3 months to issue the decision regarding accreditation.
At any time it is deemed necessary, or when requested by an outside body, the committee will verify that certified specialists meet the criteria for maintaining their certification. Where this criterion is not met, the Committee will cancel the certification.
- 1.
The medical team responsible for the training programme must include at least one expert in INR-NI (full member of GENI/SENR) able to certify more than 10 years of uninterrupted practice and at least 2 specialists exclusively dedicated to INR-NI. It is recommended that the team provide continuous care to patients with urgent neurovascular disease.
- 2.
Annual INR-NI activity in a hospital accredited to participate in training programmes must exceed 100 therapeutic programmes per year so as to guarantee adequate hands-on experience to each specialist during the training period. The team's activity and participation by specialists in training must be recorded in an electronic database to which the accrediting committee will have access.
- 3.
They should have an INR-NI unit with a permanently reserved, specific neurovascular cath lab with aseptic conditions for patients and professionals, digital radiological technology mounted on an isocentric arc, and a reconstruction and analysis system for 3D vascular images.
- 4.
Specific hospital admission procedure, managed by the INR-NI unit, for patients with scheduled interventions, provided that they do not require intensive care. These patients should be hospitalised in the same area as neurological and neurosurgical patients. Caring for hospitalised patients is an important part of the training provided to specialists who are not clinicians.
- 5.
For this reason, the INR-NI training unit must have outpatient clinics in which patients receive medical attention and nursing care before and after their hospital stays.
- 6.
The training centre must have neurosurgical and neurology services staffed with experts in vascular disease. It is recommendable for these units to be integrated into nervous system vascular disease units (stroke units, neurovascular surgery units, and neuroradiology units).
- 7.
They should have an intensive care service or unit for patients requiring this level of care.
- 8.
If the unit schedules interventions for paediatric patients, it must also have the following:
- a.
Specialised medical, surgical, and anaesthesia care for paediatric patients
- b.
Expendable materials for use in paediatric patients
- c.
Cath lab in which all technological devices can be adapted for use in paediatric patients, especially components of radiology protection systems
- a.
- 9.
In any case, practising INR-NI will require the presence and permanent availability of a diagnostic neuroradiology unit or section with a multislice CT unit, MRI scanner of at least 1.5 T with neuroimaging sequences and software, and a volume of at least 100 CT/MRI studies weekly (head, spine, neck) on all 5 weekdays, with 10% being emergency studies.
- 10.
This unit providing the training must have up-to-date protocols for the different diagnostic and therapeutic procedures and be able to provide monitoring and follow-up for each of its interventions. Morbidity and mortality rates must be within acceptable limits.
- 11.
There must be a designated head of the training unit.
- 12.
Given the complexity of INR-NI and the risks posed by improper practices in this area, the accreditation process must contemplate not only initial training, but also a mechanism for maintaining accreditation based on the criteria set forth in Appendix 3.
Criteria required of all hospitals and specialists practising INR-NI
In addition to appropriate training for specialists, as described in this training and certification programme (Appendix 4), there are certain requirements for maintaining INR-NI accreditation up to date.
- •
INR-NI should be carried out within multidisciplinary teams that foster the exchange of knowledge and experiences.
- •
The accreditation provided by this training programme does not certify doctors to practise INR-NI immediately and on an individual basis; rather, it certifies candidates as members of an existing INR-NI team that includes at least one trained and certified specialist with at least 5 years of experience.
- •
Practising INR-NI must be based on criteria of efficiency, safety, and quality of care within structured INR-NI units that perform all procedures pertaining to that area of study and provided by that hospital.
- •
Specialists with INR-NI certification must show that at least 50% of their overall clinical activity has to do with that area of knowledge.
- •
INR-NI teams must maintain a close functional relationship with diagnostic neuroradiology units.
- •
INR-NI techniques should be carried out in units able to demonstrate sufficient experience with such techniques and procedures.
The committee responsible for certifying INR-NI training will ensure that the activities performed by accredited specialists take place according to the stipulated guidelines so as to be able to guarantee up-to-date accreditation.
- 1
Training itinerary A
- 1.1
Anatomical and physiological foundation
- 1.1.1
Arterial and venous angiographic anatomy of the central nervous system, head, neck, and spinal column
- 1.1.2
Vascular territories. Anatomical variants
- 1.1.3
Collateral circulation. Dangerous anastomosis
- 1.1.4
Cerebral blood flow. Self-regulation
- 1.1.1
- 1.2
Anatomy and physiology of soft tissues and related bone structures
- 1.2.1
Cranio-facial and vertebrae anatomy
- 1.2.2
Anatomy and physiology of the CNS and soft tissues of the neck, face, and spine
- 1.2.3
Anatomy of the articular and muscle-ligament structures of the spinal column
- 1.2.1
- 1.3
CNS pharmacology and basic neurovascular physiology
- 1.3.1
Vasodilators and vasoconstrictors
- 1.3.2
Pharmacological agents used in functional tests
- 1.3.3
Coagulation cascade. Anticoagulants. Antiplatelet agents. Thrombolytic agents
- 1.3.4
Drugs and therapeutic measures used to control arterial pressure and heart rate
- 1.3.5
Treatment for allergic reactions
- 1.3.6
Prevention and treatment for infections
- 1.3.7
Stroke prevention
- 1.3.8
Neurophysiology: functional tests
- 1.3.1
- 1.4
Pathological entities
Classification, clinical presentation, diagnostic imaging findings, natural history, epidemiology, haemodynamic and physiological basis of the disease, and treatment, treatment indications and techniques, treatment contraindications, therapeutic alternatives, combination treatments, treatment risks, and management of complications in:
- 1.4.1
Aneurysms, vascular malformations, and arteriovenous fistulas
- 1.4.2
Vascular trauma
- 1.4.3
Cerebrospinal haemorrhages
- 1.4.4
Postsurgical epistaxis and ORL haemorrhages.
Stroke and cerebral ischaemia
- 1.4.5
Congenital, neoplastic, inflammatory, and degenerative angiopathies
- 1.4.6
Vertebral fractures and degenerative processes
- 1.4.7
Nervous system, meningeal, and craniospinal neoplasm
- 1.4.1
- 1.1
- 2
Training itinerary B
- 2.1
Anatomical and physiological foundation
- 2.1.1
Arterial and venous angiographic anatomy of the central nervous system, head, neck, and spinal column
- 2.1.2
Vascular territories. Anatomical variants
- 2.1.3
Collateral circulation. Dangerous anastomosis
- 2.1.1
- 2.2
Technical aspects of endovascular procedures
- 2.2.1
Drug delivery catheters and release systems
- 2.2.2
Embolic, sclerosing, and bone-reinforcing agents
- 2.2.3
Stents, balloons, and other revascularisation devices
- 2.2.4
Flow-guided catheters and embolisation
- 2.2.5
Complications of angiography and embolisation
- 2.2.6
Flow-diverting techniques and use of collateral networks
- 2.2.1
- 2.3
Pathological entities
Classification, clinical presentation, diagnostic imaging findings, natural history, epidemiology, haemodynamic and physiological basis of the disease, treatment indications and techniques, treatment contraindications, therapeutic alternatives, combination treatments, treatment risks, and management of complications in:
- 2.3.1
Aneurysms, vascular malformations, and arteriovenous fistulas
- 2.3.2
Vascular trauma
- 2.3.3
Cerebrospinal haemorrhages
- 2.3.4
Postsurgical epistaxis and ORL haemorrhages.
Stroke and cerebral ischaemia
- 2.3.5
Congenital, neoplastic, inflammatory, and degenerative angiopathies
- 2.3.6
Vertebral fractures and degenerative processes
- 2.3.7
Nervous system, meningeal, and craniospinal neoplasm
- 2.3.1
- 2.4
Neurophysiology: functional tests
- 2.5
Therapeutic injection and direct puncture techniques, including aspiration biopsy
- 2.6
Contrast agents
- 2.7
Protective measures against ionising radiation
- 2.1
Please cite this article as: Fortea F, Masjuan J, Arikán-Abello F, Rovira A, González A, Arenillas J, et al. Criterios para la formación y capacitación en Neurorradiología Intervencionista-Neurointervencionismo, acordados por el Grupo Español de Neurorradiología Intervencionista (GENI), la Sociedad Española de Neurorradiología (SENR), el Grupo de Estudio de Enfermedades Cerebrovasculares (GEECV) de la Sociedad Española de Neurología (SEN) y el grupo experto en enfermedades vasculares de la Sociedad Española de Neurocirugía (SENEC). Bases para la obtención de una Acreditación de Centros y Especialistas en Neurorradiología Intervencionista-Neurointervencionismo. Neurología. 2017;32:106–112.
By an agreement of the authors and editors, the full version of this article was also published in Neurocirugía, http://dx.doi.org/10.1016/j.neucir.2015.11.001.