Headache has a negative impact on health-related quality of life in young patients. We aim to analyse the characteristics of a series of young patients visiting a headache clinic and estimate the burden of different types of headaches listed by the International Classification of Headache Disorders (ICHD).
MethodsWe prospectively recruited patients aged 14 to 25 years who were treated at our clinic during a period of 6.5 years. We recorded each patient's sex, complementary test results, and previous treatment. We subsequently compared the characteristics of our sample to those of patients older than 25.
ResultsDuring the study period, we treated 651 patients aged 14 to 25 years; 95.6% had received symptomatic treatment, and 30.1% had received preventive treatment. A total of 755 headaches were recorded. Only 80 were secondary headaches, most of which were included in Group 8; 77.2% were included in Group 1, 3.1% in Group 2, 1.2% in Group 3, 5% in Group 4, 0.6% in Group 13, and 0.9% in Group 14. According to Headache Impact Test (HIT-6) scores, headache had at least a moderate impact on the quality of life of 449 patients.
ConclusionMost headaches in young patients can be classified according to ICHD criteria. Migraine was the most frequent diagnosis in our sample. Although headache was commonly associated with a negative impact on quality of life, most patients had received little preventive treatment before being referred to our clinic.
La cefalea produce un impacto negativo sobre la calidad de vida de los jóvenes. Nuestro objetivo es analizar las características de esta población en una consulta monográfica de cefaleas (CMC) y evaluar la carga de las diferentes cefaleas codificadas según la Clasificación Internacional de Cefaleas (CIC).
MétodosDurante un período de 6 años y medio, se han registrado los pacientes de edades entre los 14 y los 25 años atendidos en la CMC recogiendo de cada uno de ellos el sexo, pruebas complementarias y tratamiento utilizado previamente. Se llevó a cabo la comparación de las características de esta población con la de mayores de 25 años.
ResultadosSeiscientos cincuenta y un pacientes de entre 14 y 25 años fueron atendidos durante el período de inclusión; el 95,6% había recibido tratamiento sintomático y el 30,1% tratamiento preventivo. Setecientas cincuenta y cinco cefaleas fueron registradas, 80 fueron cefaleas secundarias, la mayoría codificadas en el grupo 8. El 77,2% de ellas fueron incluidas en el grupo 1, el 3,1% en el grupo 2, el 1,2% en el grupo 3 y el 5% en el grupo 4. El 0,6% de ellas fueron clasificadas en el grupo 13 y el 0,9% en el grupo 14. En 449 pacientes la puntuación del Headache Impact Test (HIT-6) mostró al menos un impacto moderado sobre la calidad de vida.
ConclusiónLa mayoría de las cefaleas en jóvenes podrían ser codificadas de acuerdo con los criterios de la CIC. La migraña fue el diagnóstico más frecuente. Aunque la cefalea fue comúnmente asociada con impacto negativo en la calidad de vida, los tratamientos preventivos no fueron utilizados extensamente antes de ser derivados a la CMC.
Headache is a frequent cause of somatic symptoms and a common reason for consultation among adolescents and young adults. Migraine and tension-type headache are the most frequent types of headache in this population.1,2 Correct diagnosis and appropriate treatment are essential due to the negative impact of headache on these patients’ physical, psychological, and social well-being.
These patients are at a high risk of developing chronic disorders, anxiety, and depression. The condition may have a negative impact on family and social relationships, school attendance, and academic performance.3–5
The purpose of this study is to analyse the characteristics of a group of young patients (ages 14 to 25 years) attended at the headache unit of a tertiary hospital. We also aimed to evaluate the prevalence of each type of headache according to the diagnostic criteria of the second and third editions of the International Classification of Headache Disorders (ICHD-2 and ICHD-3 beta version).6,7
Material and methodsWe prospectively gathered patients aged 14 to 25 attended at our hospital's headache unit between January 2008 and July 2016. Due to the structure of our region's healthcare system, the unit only receives patients aged 14 and over, who in most cases are referred by primary care physicians.
We recorded demographic characteristics (age and sex), age at onset of headache, the referring healthcare professional, the need to perform complementary tests during diagnosis at our unit, and treatments administered before referral (both symptomatic and preventive).
All types of headache were codified according to the ICHD-2 diagnostic criteria (or the ICHD-3-beta criteria, after the last version was published). In cases of discrepancies between the ICHD-2 and ICHD-3 beta diagnoses, we used the latter. When a patient met criteria for more than one headache type, all relevant types were diagnosed and codified.
We evaluated the negative impact of headache on quality of life using the 6-item Headache Impact Test (HIT-6).8
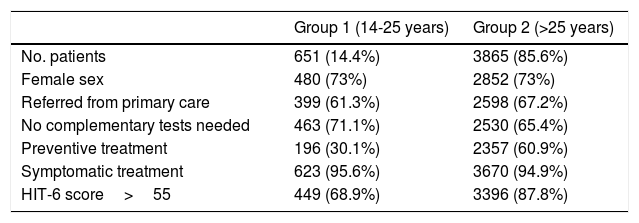
We also compared results from our sample of patients aged 14 to 25 years (group 1) to those of patients aged over 25 who were attended at our headache unit during the study period (group 2).
ResultsGroup 1 included 651 patients (14.4% of the sample; 171 male and 480 female) and group 2 included 3865 patients (85.6%; 1013 male and 2852 female).
Among patients in group 1, 399 (61.3%) were referred by primary care physicians; 623 (95.6%) had received at least one type of symptomatic treatment prior to inclusion in the study, but only 196 (30.1%) had received preventive treatment. The most frequently used preventive drugs were beta blockers (39.8%) and calcium channel antagonists (38.4%) in group 1, and antidepressants (46.2%) and neuromodulators (39%) in group 2. No complementary testing was necessary for diagnosis in 463 cases (71.1%).
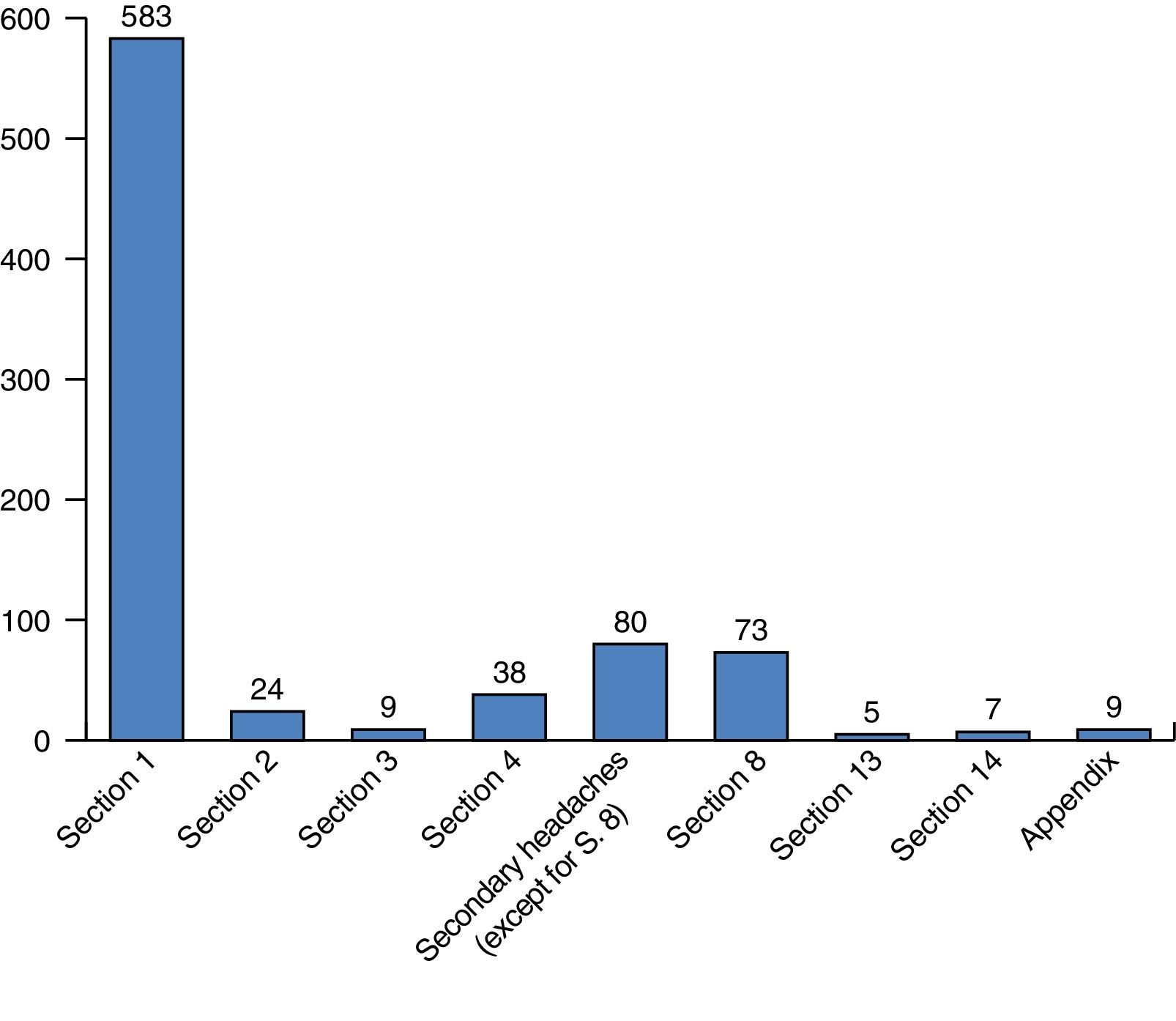
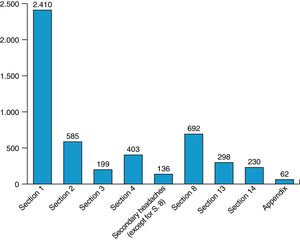
A total of 755 headache episodes were recorded in group 1. Of these, 654 (86.6%) were primary headaches (ICHD sections 1 to 4), and 80 (10.5%) were secondary headaches (sections 5 to 12). Five episodes (0.6%) were classified into ICHD section 13 (painful cranial neuropathies), 7 (0.9%) into section 14 (other headache disorders), and 9 (1.1%) into the appendix. Fig. 1 shows the number of episodes per ICHD section.
Regarding primary headaches, 583 episodes (77.2% of the total) were included in section 1 (migraine); 157 (26.9%) met diagnostic criteria for chronic migraine, and 73 of these were associated with symptomatic medication overuse. Migraine was associated with some type of aura in 94 episodes (16.1%).
Only 24 episodes (3.1% of all headache episodes) were classified into ICHD section 2 (tension-type headache), 9 (1.2%) fell into section 3 (trigeminal autonomic cephalalgias), and 38 (5%) into section 4 (other primary headache disorders). Among the episodes of tension-type headache, 9 (37.5%) met criteria for chronic tension-type headache, 13 (54.2%) for frequent episodic tension-type headache, and only 2 (8.3%) for infrequent episodic tension-type headache. Of the 9 episodes of trigeminal autonomic cephalalgias, 4 were cluster headaches and 4 were episodes of hemicrania continua. The most frequent subtypes of other primary headache disorders in our sample were primary stabbing headache (22 episodes) and nummular headache (14 episodes).
Secondary headaches were less frequent in our series; most episodes (72, 9.5%) were included in section 8 (headache attributed to a substance or its withdrawal).
The impact of headache on quality of life was at least moderate (HIT-6>55) in 449 patients (68.9%).
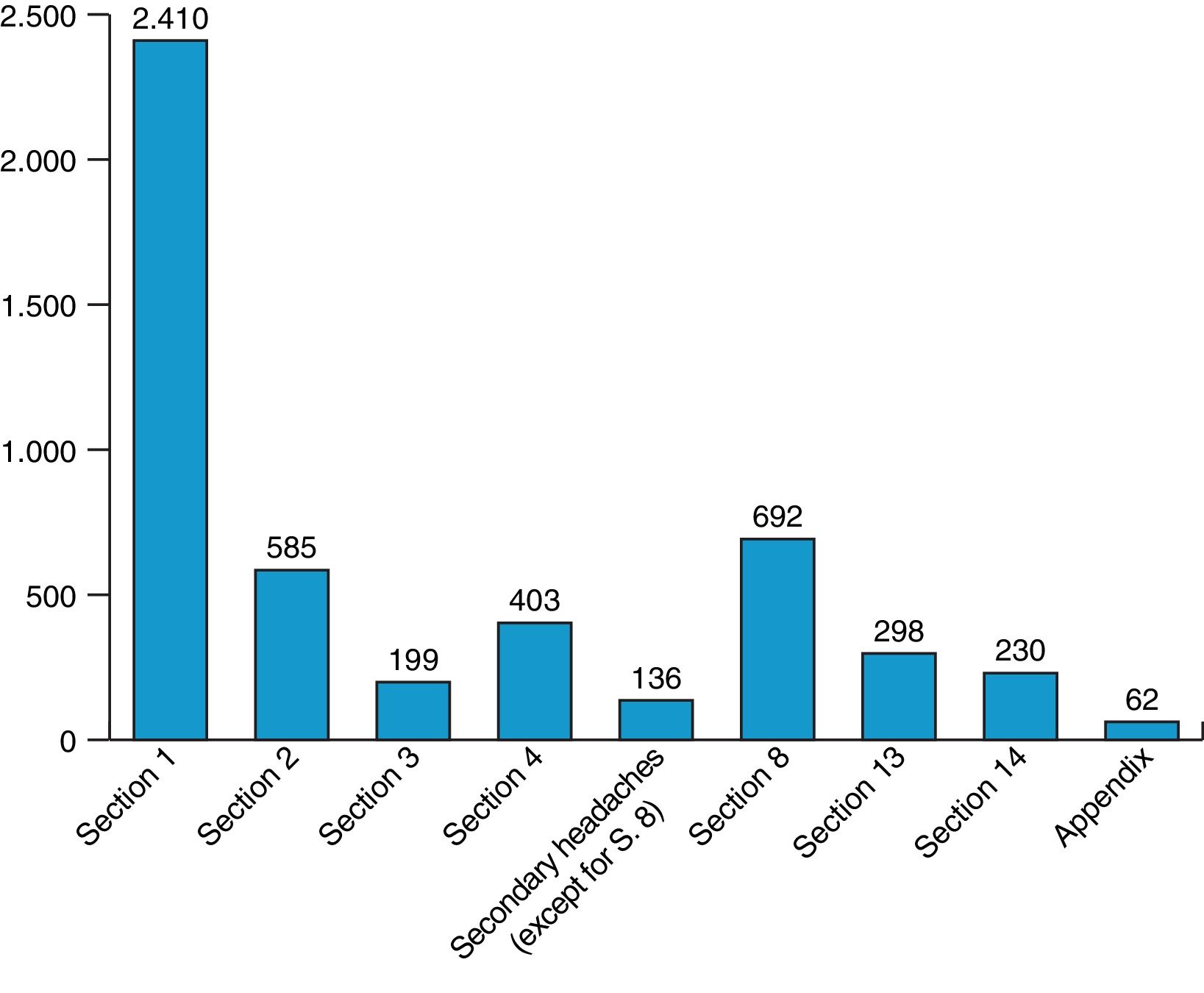
Table 1 compares the characteristics of patients in groups 1 and 2. Fig. 2 shows the distribution of episodes by ICDH section in the patients aged over 25 years.
Patient characteristics by group.
| Group 1 (14-25 years) | Group 2 (>25 years) | |
|---|---|---|
| No. patients | 651 (14.4%) | 3865 (85.6%) |
| Female sex | 480 (73%) | 2852 (73%) |
| Referred from primary care | 399 (61.3%) | 2598 (67.2%) |
| No complementary tests needed | 463 (71.1%) | 2530 (65.4%) |
| Preventive treatment | 196 (30.1%) | 2357 (60.9%) |
| Symptomatic treatment | 623 (95.6%) | 3670 (94.9%) |
| HIT-6 score>55 | 449 (68.9%) | 3396 (87.8%) |
The prevalence of headache among young patients increases with age.9,10 Several studies have addressed the prevalence of headache in school-age children, adolescents, or university students, but no data are available about this age group as a whole. This population usually experiences pain of different characteristics from that of adults. For example, headache is more frequent in the morning, in association with academic activities. Episodes are shorter, more frequent, and less severe; many patients may experience spontaneous remission without symptomatic treatment.11–13 These unique characteristics make it difficult to apply the ICHD, correctly diagnose headache type, and provide adequate treatment.6,7
According to other studies on the topic, headache has a negative impact on these patients’ quality of life and ability to relate with their family and classmates. Headache may therefore be a predisposing factor for physical and mental disorders.2,3,5,12–17 At this crucial stage of life, patients with headache disorders present higher rates of absence from school or university, resulting in poorer intellectual performance and academic education.4,5 Our results show that the percentage of young patients experiencing at least moderate impact of headache is lower than that observed among patients over 25 years old, but is higher than among young individuals in general.
Previous studies have found an association between recurrent headache and such lifestyle factors as low levels of physical activity, obesity, and smoking.17–19
The sex distribution of headache in our series (72% female) is similar to that of the group of older patients (73%). Previous studies have shown that the incidence of headache is greater among women from adolescence, a tendency that persists throughout their lifetimes.9,10,13
As may be expected, most headache episodes in our series correspond to primary headaches. The percentage of episodes of migraine (ICHD section 1) is very high in both age groups. The percentage of patients with migraine in our sample is higher than those reported for adolescents or university students.1,4,10,12 Though they are more frequent among children (who were not included in our series), we should consider such periodic syndromes as abdominal migraine, cyclic vomiting syndrome, and benign paroxysmal vertigo, which are considered precursors to migraine.9,10
We were not surprised to observe that the proportion of patients with chronic migraine among all individuals with migraine was higher among patients aged 14 to 25 years old than among those older than 25. However, the fact that over a quarter of patients with migraine in the younger group had chronic migraine should call attention to the high prevalence of this disabling condition among young individuals.
Regarding the other categories of primary headache, we were not surprised to find that the percentages of episodes attributed to tension-type headache and trigeminal autonomic cephalalgias were higher among patients over 25 years old. Tension-type headache is less frequent in our series than in other published series of young patients. This difference may be due to the fact that our series was drawn from the headache unit of a tertiary hospital, or due to previous series classifying some patients with chronic migraine as patients with tension-type headache.2,20
Regarding ICHD sections 3 and 4, the frequency of cluster headache and primary stabbing headache in our series is similar to those reported in other series.10 We wish to call attention to hemicrania continua and nummular headache, which were relatively frequent in our series and are not rare among young individuals.21,22
Secondary headaches were not frequent in our series; most corresponded to ICHD section 8 (headache attributed to a substance or its withdrawal). While the percentage of headache episodes attributed to medication overuse was higher among patients aged over 25 than among the younger group, we were concerned by the considerable number of patients with this diagnosis in our series. Symptomatic medication overuse and the limited use of preventive treatment may result in chronic transformation of migraine in young patients.23
As may be expected, the presence of painful cranial neuropathies (ICHD section 13) and other headache disorders (section 14) in our series is anecdotal.6,10,20
Most patients in both groups were referred by primary care physicians. It is therefore not surprising that the percentages of symptomatic and preventive treatment use were similar between groups. Previous use of preventive treatment was infrequent in our sample, especially considering the negative impact of headache on this population. We should raise awareness, especially among primary care physicians, of the fact that lack of appropriate preventive treatment results in medication overuse and frequently in chronic transformation of headache, which has a negative impact on patients’ quality of life.3,17,18
In conclusion, the great majority of headaches in young patients can be codified using the ICHD criteria. Migraine was the most frequent type of headache in our series. Chronic migraine and symptomatic medication overuse may have a negative impact on the quality of life of young patients.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pedraza Hueso MI, Ruíz Piñero M, Martínez Velasco E, Juanatey García A, Guerrero Peral AL. Cefalea en jóvenes: características clínicas en una serie de 651 casos. Neurología. 2019;34:22–26.