Intraneural ganglion cysts are very infrequent benign lesions generally affecting peripheral nerves, particularly the external popliteal sciatic (EPS) nerve. They may cause symptoms of neuropathic pain, frequently manifesting as paralysis of the EPS nerve, which requires differential diagnosis from such other conditions as trauma, spinal compression syndrome, or lumbar disc or tumour lesion.1 Early diagnosis is equally necessary, since delayed diagnosis leads to axonal injury, which may cause muscle denervation.2 In the case of the tibialis anterior and fibularis longus and brevis muscles, which are responsible for foot dorsiflexion and eversion, denervation may be irreversible. Since the first description of an intraneural ganglion cyst of the SPE in 1809, pathophysiology and the different treatments proposed have constantly been debated; treatments were based on irregular clinical findings and high recurrence rates. The most widely accepted theory, Spinner's3,4 unifying articular theory, was proposed in 2003. According to this theory, the ganglion cyst arises from the superior tibiofibular joint; the cyst allows fluid to infiltrate the articular branch of the EPS nerve, to which it is connected, and through a one-way valve mechanism, that mucinous content fills and dissects the nerve in a proximal direction.5–7 The clinical findings constitute the most conclusive aspect of this theory, revealing decreased recurrence rates after procedures for ligating and disconnecting this articular branch were introduced into surgical treatment.8–11
We present a series of 2 cases of intraneural ganglion cyst of the EPS nerve and describe the patients’ clinical and neuroimaging manifestations, treatment, and outcomes. We also review the literature on the subject.
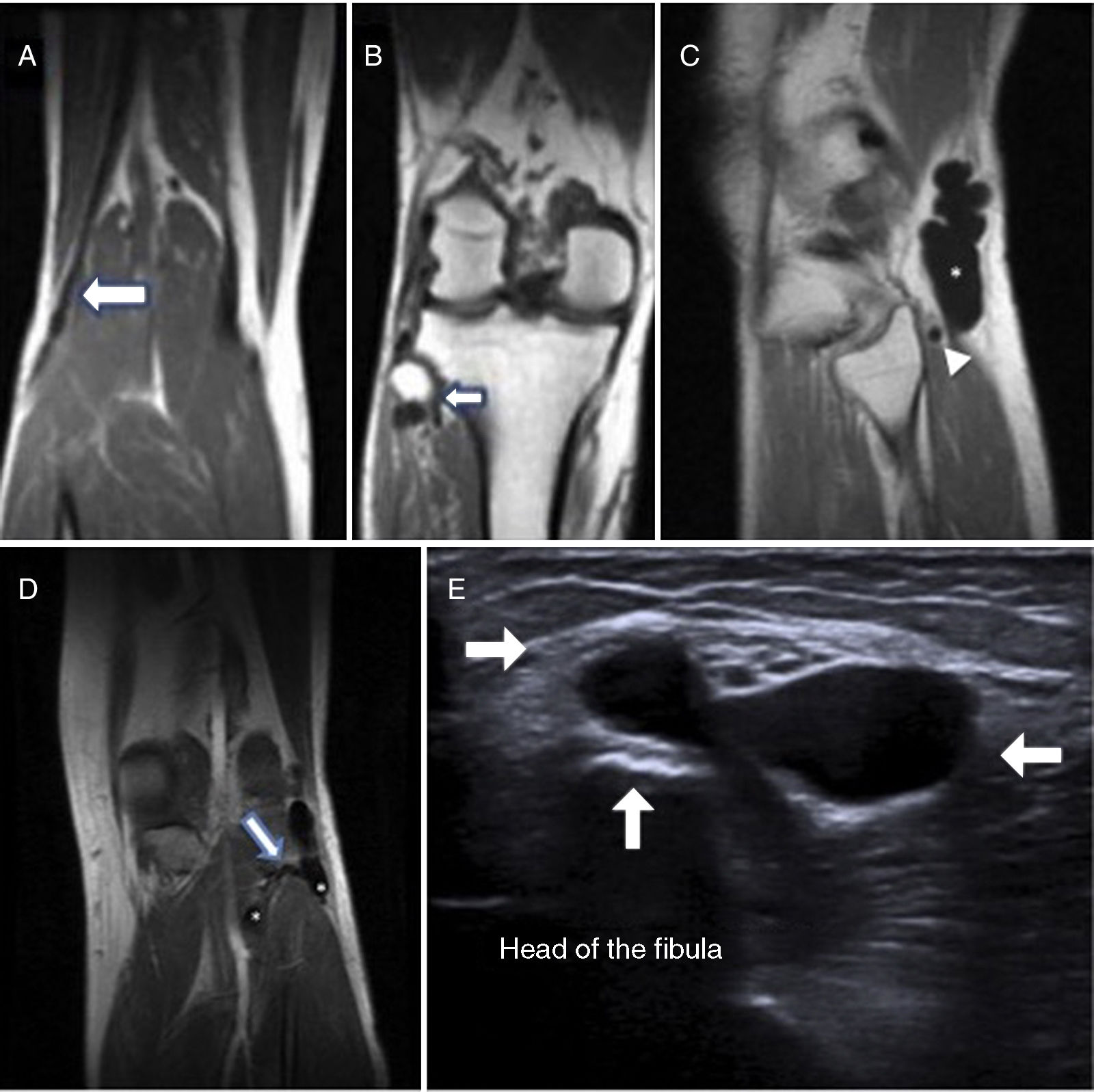
Case 1The patient was a 52-year-old man with no relevant medical history. He visited the hospital due to a 4-month history of decreased sensitivity of the right instep and the outer surface of the leg, together with steppage gait. Examination revealed loss of strength (2/5) on dorsiflexion and hallux extension of the right foot, lack of lower back pain on palpation, and deep tendon reflexes. Tinel test on the EPS nerve at the level of the head of the fibula yielded negative results. A neurophysiological study revealed chronic axonal neuropathy of the right EPS nerve. The electroneurography showed diminished motor conduction speed of the EPS nerve in the section between the popliteal fossa and the head of the fibula, as well as decreased motor and sensory potential amplitude in the superficial peroneal branch. The electromyography revealed no acute denervation (spontaneous activity) in the tibialis anterior and fibularis longus muscles, with signs of chronic reinnervation, and motor unit action potentials of increased amplitude, duration, and polyphasia. An MRI scan showed a multilobular mass measuring 2cm adhering to the head of the fibula, and atrophy of the anterior tibialis muscle due to denervation; these findings are compatible with malformation or arthrosynovial cyst (Fig. 1A and B). An ultrasound revealed an avascular anechoic tubular structure of cystic content inside the EPS nerve, compatible with an intraneural ganglion cyst arising from the superior tibiofibular joint.
Patient 1: (A and B) Coronal MRI section showing the beginning and the end of the lesion. Patient 2: (C) Sagittal MRI section showing a cyst-like ganglion (asterisk) and the dilated section of the articular branch (arrowhead). (D) Coronal MRI section showing how the common peroneal nerve is affected in the area proximal to the superior tibiofibular joint and its distal extension, with bifurcation into a superficial and deep component, demonstrating the connection with the superior tibiofibular joint (outlined arrow). (E) Ultrasound image revealing the ganglion cyst limits at the articular level (white arrows).
The patient was a 53-year-old man with no previous trauma or relevant personal history, who visited our hospital due to a 6-week history of foot drop and paraesthesia of the left lateral leg, which he believed to be due to work overload. Baseline examination revealed a soft tumour which was palpable at the level of the head of the fibula; Tinel sign was positive at that point. Muscle strength was 2/5 in the anterior tibialis muscle and 3/5 in the extensor hallucis longus muscle. A neurophysiological study revealed acute axonal neuropathy of the left EPS nerve. Electroneurography findings were consistent with those of case 1, whereas the electromyography showed denervation (spontaneous activity) in the tibialis anterior and fibularis longus muscles, manifesting as fibrillations and positive waves, with normal motor unit action potentials. Given these findings, we jointly performed an ultrasound and an MRI scan, which revealed an intraneural cyst-like tumour along the EPS nerve, showing distension and occupation of the articular branch by liquid, extending to the proximal tibiofibular joint (Fig. 1C-E).
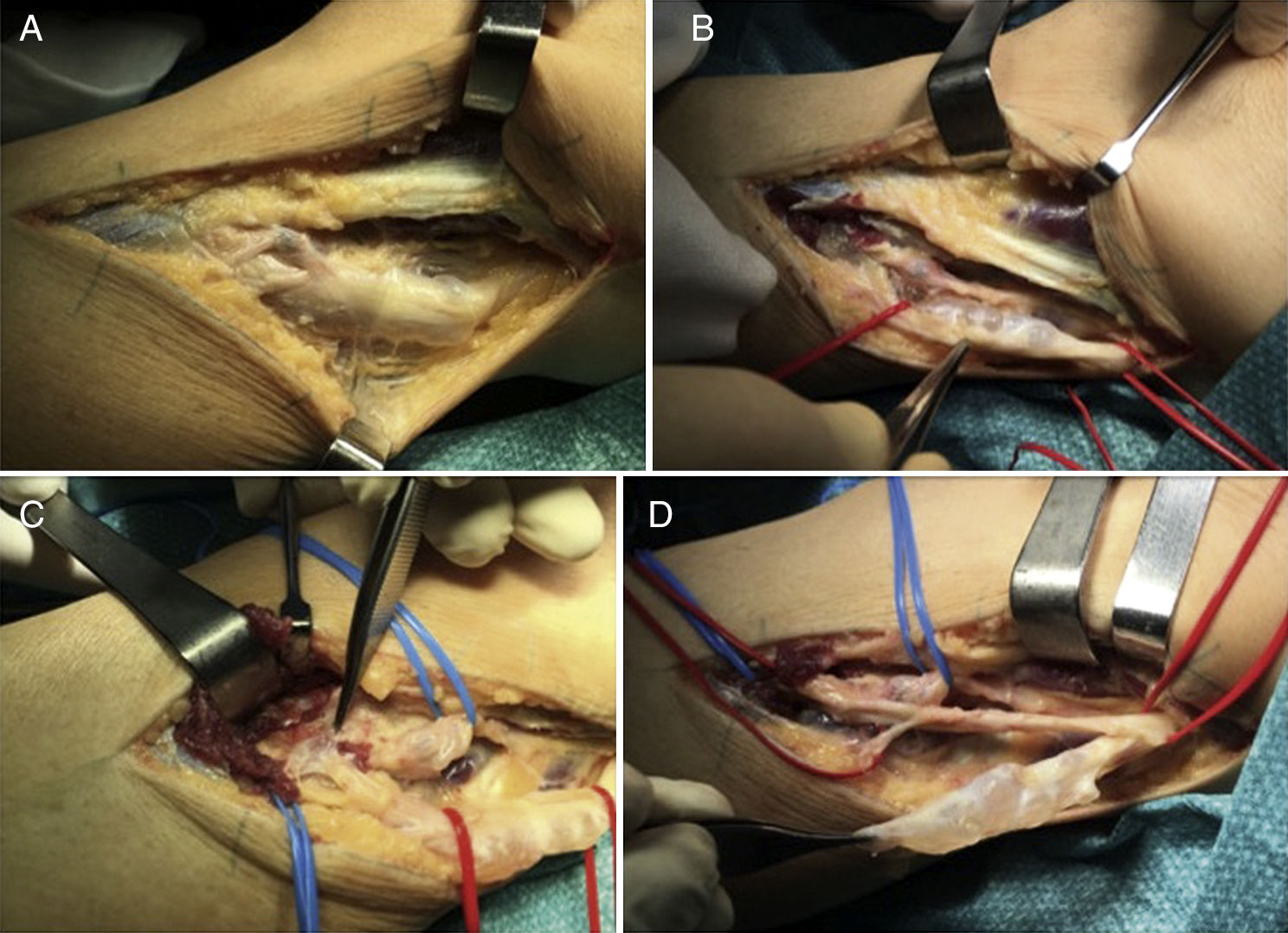
Based on the above mentioned theory, both cases were managed similarly, with identification and dissection of the EPS nerve from the level of the head of the fibula to the bifurcation of the sciatic nerve (Fig. 2A and B), identifying the articular branch (Fig. 2C) and ligating it to prevent recurrence. We performed a longitudinal epineurotomy to remove the cystic content and decompress the nerve (Fig. 2D). In both cases, outcomes were considered positive since total, albeit delayed, recovery of sensitivity was achieved; in patient 1, muscle strength increased 2 points (4/5) and in patient 2, strength of the anterior and extensor hallucis longus muscles was 4/5 and 5/5, respectively. These results were observed at 2 years (patient 1) and one year (patient 2) of follow-up.
(A) Lateral approach by planes. (B) Ganglion cyst dissection and delimitation, revealing its cystic composition. (C) The dissecting forceps indicates the area where the superior tibiofibular joint connects with the articular branch. (D) Epineurotomy and resection of the intraneural ganglion cyst.
According to the literature, better results are generally observed in pain control, as motor recovery is less predictable and more variable. Predicting post-surgical progression of these patients is more difficult, since the common peroneal nerve does not regenerate as easily as other nerves.12 In both cases, despite the presence of a pronounced impairment of dorsiflexion before surgery, we obtained very satisfactory results, with fast motor and sensory recovery, and without the most frequent complication, recurrence. In our experience, previous muscle denervation observed by electromyography, progression time, and the patient's age constitute the most reliable prognostic factors.
Please cite this article as: García García FJ, Pescador Hernández D, Rendon Díaz D, Blanco Blanco J. Ganglión intraneural del nervio ciático poplíteo externo. Una posible causa de pie caído. Neurología. 2018;33:486–489.