Atypical non-arteritic anterior ischaemic optic neuropathy (NAION) is defined as those cases that manifest in young patients (<50 years) or those lacking classical risk factors for typical NAION.1,2
Atypical NAION may have a more insidious clinical presentation, usually with a milder loss of visual acuity, and with greater frequency of bilateral involvement than typical cases. Cases have been described of atypical NAION related to such drugs as amiodarone,1 5-alpha-reductase inhibitors,3 nasal decongestants,4 and epinephrine5; as well as cases associated with tumours, prothrombotic states, and perioperative bleeding.1
We present the case of a young, healthy patient with no history of cardiovascular risk factors, who presented sequential bilateral atypical NAION during a hypertensive crisis secondary to massive intake of liquorice root extract over a period of 5 years.
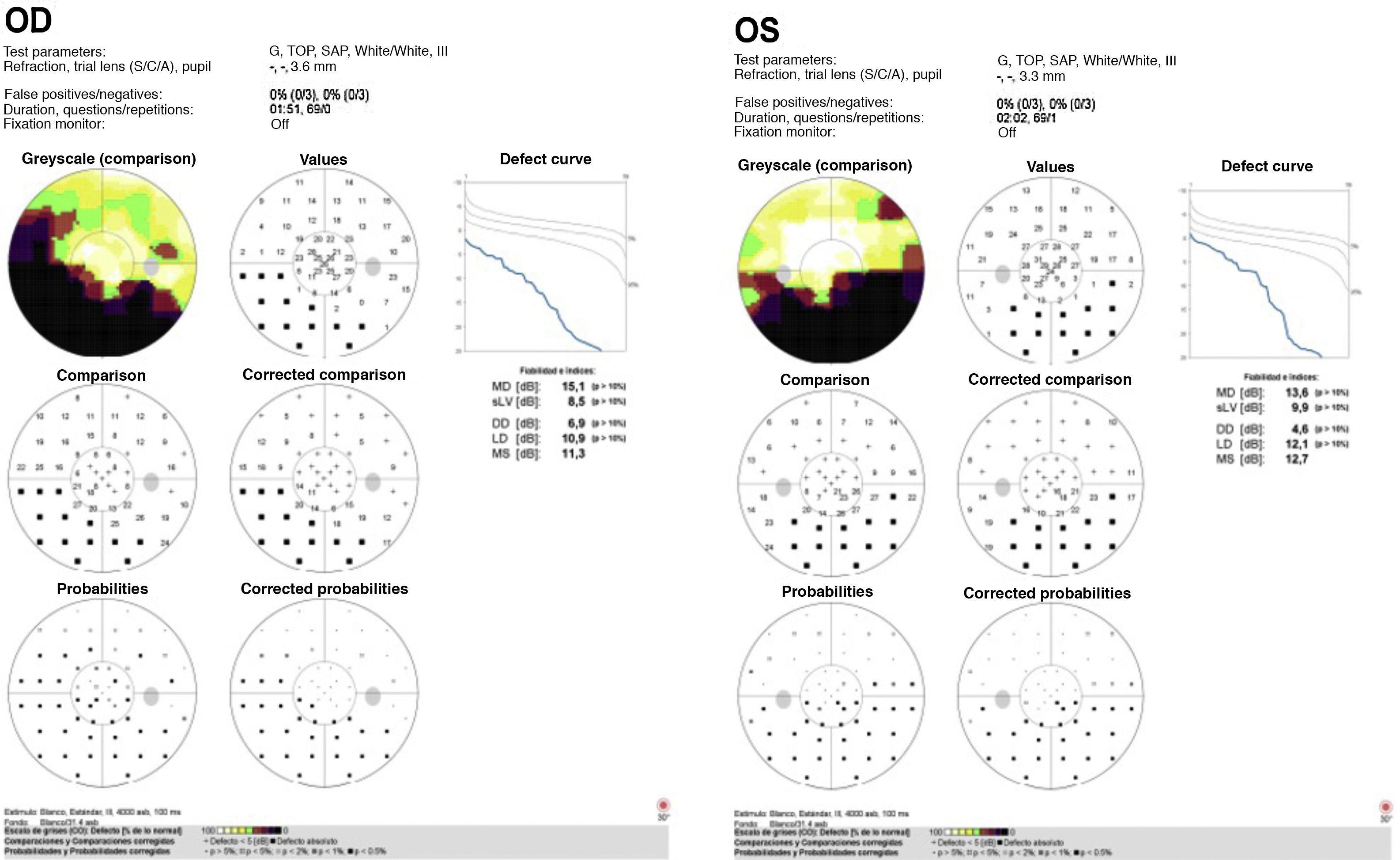
Clinical caseOur patient was a 39-year-old man who in the context of a hypertensive crisis presented altered visual field in the right eye (OD), describing difficulty perceiving images in the inferior field, leading to his referral to the neuro-ophthalmology unit. The patient had no relevant personal or family history. He reported episodes of holocranial headache progressing for months, which improved with analgesics. The ophthalmological examination revealed visual acuity of 0.8 in OD, normal anterior pole, papilloedema with poorly-defined edges in the fundus examination, and 2 flame-shaped haemorrhages in OD; in the left eye (OS), the papilla was apparently normal, with optic disc cupping of 0.2. A visual field test revealed a lower altitudinal defect (Fig. 1) and a blood analysis including complete blood count, C reactive protein, and glomerular sedimentation rate yielded normal results. The absence of any other systemic or neurological symptoms, as well as the normal results obtained in the complementary tests, ruled out other causes of unilateral papilloedema in young patients, including infiltrative, compressive, or post-traumatic neuropathy. The patient was diagnosed with atypical NAION in the context of uncontrolled essential arterial hypertension (AHT). After 5 months of follow-up, the patient visited the emergency department due to similar visual symptoms, but this time involving the left eye. After the examination, he was diagnosed with atypical NAION. During a more detailed history-taking, the patient reported daily consumption of liquorice root extract capsules for 5 years. After examination at the internal medicine department, he was diagnosed with arterial hypertension secondary to primary pseudohyperaldosteronism (pseudo-HAP) due to excessive liquorice intake.
Discussion and conclusionsThe isoenzymes 11β-hydroxysteroid dehydrogenase type 1 (HSD11B1) and type 2 (HSD11B2) play an important role in ion regulation and arterial pressure, catalysing conversion between cortisol and its inactive metabolite, cortisone. HSD11B2 is predominantly expressed in tissues sensitive to mineralocorticoids; when locally catalysing the conversion of cortisol into cortisone, it prevents the activation of mineralocorticoid receptors through physiological concentrations of cortisol in the body.6
Liquorice contains glycyrrhizin, which is absorbed in the intestine and converted into glycyrrhizinic acid (GA), which competitively inhibits HSD11B2. High concentrations of GA prevent the catabolism of cortisol into cortisone, causing activation of mineralocorticoid receptors, which results in a state of hypermineralocorticoidism that may clinically manifest as AHT secondary to hypokalaemia.7 The neurological alterations described to date in association with liquorice consumption, including paresis, paralysis, and encephalopathies, are secondary to AHT and electrolyte imbalance.8
One gramme of liquorice contains an average of 2 mg of GA; however, this concentration is variable, particularly in extracts such as those consumed by our patient, in which concentrations of up to 98 mg/g have been reported.6,7
We suspect that excessive consumption of this extract caused secondary AHT, which predisposed our patient to sequential bilateral atypical NAION.
Our case is particularly interesting due to the unusual association between pseudo-HAP and atypical NAION. We should underscore the importance of detailed history-taking in cases of atypical NAION, given its association with a broad range of drugs, conditions, and clinical situations.
Please cite this article as: Oribio-Quinto C, Collado-Vincueria I, Pineda-Garrido E, Santos-Bueso E. Neuropatía óptica isquémica anterior no arterítica bilateral asociada a consumo de regaliz. Neurología. 2021;36:554–556.