In 1971 Spillane described painful legs-moving toes syndrome (PLMT)1 in 6 patients with involuntary and continuous movements of legs and toes in association with causalgic pain. Ever since, a number of different publications have featured new cases, always in the form of short series or case reports. Several authors recognise different subtypes within PLMT: unilateral impairment, upper limb impairment, upper and lower limb involvement, and the painless variety described by Walters in 1993 which is considered to be extremely rare.2 PLMT is a neurological disorder requiring clinical diagnosis. There is no established complementary test confirming that diagnosis.3 It is characterised by continuous, involuntary, non-purposeful, slow, and complex movements, which are often stereotypical and may be momentarily reduced or abolished at will. They usually disappear when the patient is in a deep sleep. Movements have a broad phenotypic spectrum with flexion-extension, abduction-adduction, and rotational motion of the toes, appearing in different combinations. More proximal involvement of the limbs (hand or foot) may also appear. Pain is another characteristic of the syndrome. Involuntary movements are usually preceded by a burning, sharp, stabbing, electric, or other type of pain. The syndrome may cause sensations ranging from mild discomfort to incapacitating pain. This pain lacks a metameric or peripheral nerve distribution and it cannot be relieved by voluntary movement of the affected limb. PLMT syndrome has been linked to multiple causes4: central nervous system disorders (ischaemic stroke, encephalitis, myelopathies) and peripheral nervous system disorders (radiculopathies, all types of neuropathies [toxic, nerve entrapment, traumatic]); soft tissue trauma without neuropathic lesions (muscle, tendon, fat, blood vessels, synovial tissue, or bone); neurodegenerative diseases (Wilson's disease); autoimmune diseases (Hashimoto's thyroiditis); adenosine deficiency in blood; and drugs (neuroleptics, anticholinergics, vincristine, cytarabine, and metronidazole; the last 3 are able to cause toxic neuropathy). Many cases in which a causal relationship cannot be determined are considered idiopathic. Differential5 diagnosis of restless legs syndrome must rule out complex regional pain, focal continuous muscle activity due to axonal hyperexcitability, tardive dyskinesia caused by neuroleptics, segmental myoclonus due to spinal cord injury, continuous partial epilepsy, and post-traumatic focal dystonia. Although the aetiopathogenesis of PLMT remains unknown, it is believed that a dysfunction of the mechanisms controlling the sensory and motor afferents at the supramedullary (cortical) and spinal interneuron levels occurs due to peripheral nerve injury.6,7 A study with somatosensory evoked potentials, brain MRI, and functional MRI may support the hypothesis that involuntary movements originate in the spinal cord.8 Treatment for this condition is complex, and according to published literature, responses are poor. Doctors have tried many drugs including baclofen, clonazepam, carbamazepine, tricyclic antidepressants, gabapentin, botulinum toxin, and more aggressive methods such as lumbar sympathetic block, epidural block, or epidural spinal cord stimulation.
As stated above, the painless variation or subtype of PLMT is rare. It is named painless legs and moving toes (PLMT) when it affects the lower limbs and painless hand and moving fingers (PHMF) when it affects the hands. We will use the acronym PLME in our article to denote “painless limbs and moving extremities”, an entity which includes any painless type of PLMT. A Medline search revealed 5 articles about this painless variation in the feet (PLMT)9–13 and 1 about the painless variation in the hands (PHMF).14
We present 2 cases of PLME: one had left lower limb involvement (PLMT) secondary to foot swelling caused by a gout flare-up, and a second case with bilateral hand involvement (PHMF) possibly secondary to post-operative myelopathy following surgery to correct an occipitocervical malformation.
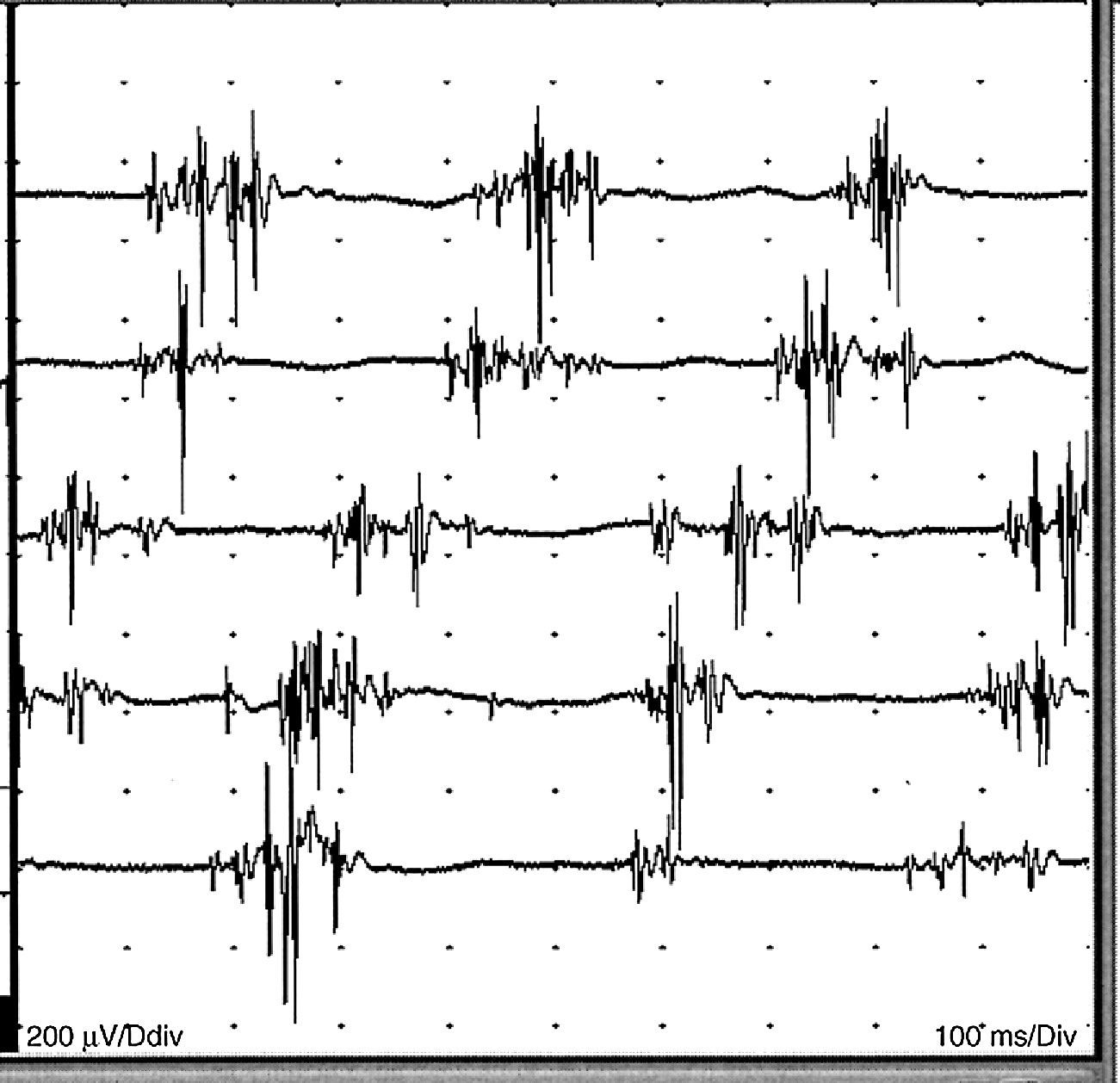
Case 1. Male patient aged 35 years with a history of hyperuricaemia and gout and undergoing treatment with allopurinol. A few weeks before his referral to our department, he had an attack of gouty arthritis in the left foot, which resulted in significant swelling of the entire foot during more than a month. He was treated with colchicine and allopurinol. He was referred to our department to assess involuntary and semicontinuous movements of the toes of the left foot, which coincided with the beginning of recovery from arthritis and persisted after it had resolved. The patient reported having experienced discomfort in his foot, but believed it to be related to arthritic inflammation. He did not subsequently complain of pain. Movements increased when moving the foot voluntarily, but they could be intentionally suppressed for short periods. He reported no use of neuroleptic or pro-dyskinetic drugs. Examination of the toes of the left foot showed low-frequency complex movement with nearly continuous flexion-extension and abduction-adduction motions which increased when he moved his foot intentionally (video footage is available). The rest of the neurological examination was normal. Cranial and cervical/dorsolumbar magnetic resonance imaging (MRI) was performed with no evidence of relevant pathological signs. The neurophysiological study (Fig. 1) revealed the presence of MUP with normal morphology and an arrhythmic but stereotyped pattern, which was spontaneous and nearly continuous. It was facilitated by the voluntary activity of the short extensor muscles of the toes, the abductor muscle of the first toe, and, to a lesser extent, the gastrocnemius muscle. Needle EMG detected no denervation activity. Voluntary movement patterns at maximal effort were normal. Results from the motor and sensory nerve conduction study were normal. The patient was diagnosed with PLMT based on these data. After a one-year follow-up period, the involuntary movement of his foot had decreased greatly. The patient repeatedly refused drug treatment since his disorder was not painful or disabling.
Case 2. Female patient aged 70 with a history of craniocervical junction surgery to treat an Arnold–Chiari malformation 27 years prior to the visit and no evidence of sequelae. The patient requested a neurological assessment due to having been experiencing continuous movements in the fingers of both hands for one year. This activity disappeared during sleep and could be abolished voluntarily. The sensation caused by this movement was unpleasant although not exactly painful, and the patient tried unsuccessfully to relieve it with voluntary movement. The patient's medical history ruled out the possibility that effects were caused by neuroleptic or other pro-dyskinetic drugs. Examination revealed mild pyramidal signs and enhanced muscle stretch reflexes, with increased area and Babinski sign in the left foot. She also presented complex, continuous, arrhythmic, irregular, low-frequency, slow movements in the fingers of both hands, which imitated the continuous muscle activity caused by myokymias or similar processes. The patient occasionally experienced abrupt jerking movements while at rest or keeping both hands still. A blood smear was performed to screen for acanthocytes, along with a biochemical analysis of TSH, ions, transaminases, ferritin, copper, and ceruloplasmin; none of the values were pathological. Cranial/cervical MRI showed postoperative changes with no posterior arch of the atlas, degenerative disc disease with central disc protrusion at C4 and C7, and no myeloradicular impairment. The neurophysiological study revealed the presence of continuous muscle activity due to MUPs of different morphologies with normal characteristics and a semi-rhythmic pattern in the short abductor muscle of the thumb, first dorsal interosseous muscle, and abductor digiti minimi on both sides although the left hand was more affected than the right. Needle EMG displayed no denervating activity. Results from the nerve conduction study were normal. During a 10-year follow-up period, she has been treated with oxcarbazepine, clonazepam, gabapentin, and pregabalin. The patient has decided not to take medication at present, since the treatments used to date have caused side effects without improving her condition. Recent examinations have found that the movement in her fingers has lessened to become nearly imperceptible.
We believe that these 2 cases should be classified as a painless variation of PMLT (PLME), with the first case corresponding to PLMT and the second case to PHMF. This appears to be an incomplete form of painful legs/moving toes syndrome that contradicts its name. It may seem like a strange choice to classify processes within an entity when they lack one of the characteristics defining the disorder, namely pain. Nevertheless, several authors believe that this variation is an incomplete form of PLMT and therefore affirm that the presence of pain is not a requirement for PLMT syndrome. We believe that PLMT and its painless variation (PLME) are poorly defined syndromes whose diagnoses are based on clinical descriptions alone. In addition, their diagnostic criteria are not solid, since cases are infrequent and their pathophysiology remains unknown. No signs have been described that would distinguish this variation of PLMT from the normal form of PLMT and researchers still do not know why some cases are painless. Since other similar processes were ruled out (including segmental spinal myoclonus, focal dystonia due to peripheral trauma, atypical forms of restless legs syndrome, tardive dyskinesias due to neuroleptic drugs, and focal forms of axonal hyperexcitability), these cases were included within PLMT syndrome. This leads us to believe that they are central in origin and often caused by peripheral trauma, although cases may of course be idiopathic. In the first case, PLMT appeared after a soft tissue lesion with arthritis and cellulitis due to a gout flare-up. In the second case, the patient had suffered a spinal injury long before developing symptoms, and faint signs of post-traumatic myelopathy were revealed by the examination. However, we cannot provide a solid explanation for the onset of PHMF 25 years after that event. We were able to clinically observe a myoclonic component in the second case, which led us to consider segmental myoclonus due to spinal cord injury as an alternative diagnosis. Nevertheless, continuous movement of the fingers was the patient's most noticeable symptom. Another alternative diagnosis could be an atypical form of restless legs syndrome (restless hands in this case) based on patient using voluntary hand movements in an attempt to make involuntary movements disappear. However, we should not forget that restless legs syndrome is basically a sensory dysfunction that causes patients to move their limbs in order to relieve this perceived discomfort. The opposite situation exists in our case: the patient suffers an involuntary movement giving rise to discomfort (not pain) which the patient tries to relieve by moving her limbs. Therefore, no sensory component is involved in this process. Researchers have described patients with PLMT as responding poorly to treatment. There are so few cases of the painless variation of PLMT (P-LME) that we are unable to draw conclusions, except to state that in our experience, painless cases are easier to treat. The first case required no treatment, and in the second, the patient decided not to take any further medications after having tried several drugs and weighing their benefits against the adverse effects.
In conclusion, we wish to highlight that much remains to be learned about the mechanisms involved in this syndrome. It also remains to be seen whether or not the painless variation (PLME) can be classified as a subtype of PMLT or if it is actually another movement disorder that we have been unable to diagnose correctly.
Please cite this article as: Pérez-Errazquin F, et al. Síndrome “painless limbs and moving extremities”. Aportación de 2 casos y revisión de la literatura. Neurología. 2013;28:121–3.