One of the main goals of the rehabilitation of patients with spinal cord injury (SCI) is the reintegration of the individual to their family, social, and work setting. The objective of this study was to identify the factors that determine the discharge destination after a traumatic spinal cord injury.
Material and methodsWe conducted a retrospective descriptive study of 305 patients with SCI who completed the rehabilitation treatment at the spinal injury unit of Hospital Insular de Gran Canaria between 2001 and 2018.
ResultsDuring the study period, we observed an increase in the number of patients referred to long-term care centres, from 9.14% between 2001 and 2010 to 18.4% between 2011 and 2018 (P < .01). Of 20 variables that presented a significant association with destination at discharge in the univariate study, 7 presented a significant association in the multivariate study: age (OR: 1.05; 95% CI, 1.02–1.08), living with a partner (OR: 0.26; 95% CI, 0.09−0.76), residing on another island (OR: 3.57; 95% CI, 1.32–9.63), smoking (OR: 3.44; 95% CI, 1.26–9.44), diabetes (OR: 6.51; 95% CI, 1.46–29.02), history of psychiatric disorders (OR: 3.79; 95% CI, 1.31–10.93), and scores on the Spinal Cord Independence Measure-III (SCIM-III) (OR: 0.48; 95% CI, 0.33−0.69).
ConclusionsOur findings identified advanced age, living on the island of Tenerife, not being married, smoking, type 2 diabetes mellitus, history of psychiatric disorders, and low SCIM-III scores as predictive factors of referral to a long-term care centre in patients with traumatic SCI in the Canary Islands.
Uno de los principales objetivos de la rehabilitación en el lesionado medular es la reintegración del individuo a su entorno familiar, social y laboral. El objetivo de este trabajo ha sido identificar los factores que determinan el destino al alta tras una lesión medular aguda traumática.
Material y MétodosSe ha realizado un estudio descriptivo retrospectivo de los 305 pacientes que han sufrido una lesión medular y han completado el periodo de rehabilitación en la Unidad de Lesionados Medulares del Hospital Insular de Gran Canaria, entre 2001−2018.
Resultados. En el periodo del estudio ha habido un incremento de los pacientes derivados a un centro socio-sanitario pasando del 9,14% entre 2001-10 al 18,4% entre 2011-18 (p<0,01). De las veinte variables con relación significativa con el destino al alta en el estudio univariante, siete variables la tuvieron en el estudio multivariante: edad (OR 1,05, 95%CI, 1,02−1,08), vivir en pareja (OR 0,26, 95%CI, 0,09−0,76), residir en otra isla (OR 3,57, 95%CI, 1,32−9,63), ser fumador (OR 3,44, 95%CI, 1,26−9,44), diabético (OR 6,51, 95%CI, 1,46−29,02), tener un antecedente psiquiátrico (OR 3,79, 95%CI, 1,31−10,93) y la valoración funcional del SCIM III (Spinal Cord Independence Measure) (OR 0,48, 95%CI, 0,33−0,69).
ConclusionesEn este estudio se ha observado que la edad avanzada, ser residente en la isla de Tenerife, no estar casado, ser fumador, tener DM-tipo 2, tener un antecedente psiquiátrico y la puntuación baja en el SCIM total son factores predictores para que un paciente que ha sufrido una lesión medular traumática en Canarias sea derivado a una residencia.
Spinal cord injury is one of the most significant traumatic events a person can experience. These injuries cause a range of psychological, family, social, and financial difficulties that affect both the patient and those around them.1 The literature includes numerous studies addressing the incidence of traumatic spinal cord injury in different countries. The reported rates vary greatly, ranging from 15 to 40 cases per million person-years. These differences in the reported incidence rates are mainly explained by methodological differences between studies and differences between countries in sociocultural and economic factors and public healthcare systems.2 The latest regional studies conducted in Spain report rates between 9.8 and 21.7 cases per million person-years.3–5
The main objective of rehabilitation is to provide the patient with all the tools needed to achieve the greatest possible degree of independence according to their neurological lesion, age, and comorbidities.6 The other major objective is to reintegrate them into their family, social, and work environment.7 Therefore, discharge of a patient with spinal cord injury to a nursing home or chronic care facility after completion of an intensive rehabilitation intervention at a specialist centre cannot be considered a positive outcome.8 While these residential centres provide whatever assistance and medical care patients may need, they also restrict individuals’ independence and social interactions, which is perceived as a loss of quality of life. Discharge to these centres is the only option for patients whose care needs cannot be met in the home setting.9
Several studies in the literature have addressed in varying degrees of detail the destination at discharge of patients admitted to specialised units due to acute spinal cord injury.6,7,10–12 All these studies date from the early 2000s and include predominantly young populations with spinal cord injury mainly secondary to road traffic accidents. Since then, the profile of patients with spinal cord injury has changed substantially. Mean patient age is increasing, mainly due to an increase in the proportion of elderly patients with spinal cord injuries due to falls.3 Older patients require a different approach to rehabilitation planning with less ambitious functional objectives, resulting in greater disability.13 This, in turn, has led to a rise in the number of patients discharged to residential centres.3
The objective of this study is to identify which factors are associated with discharge to a nursing home/chronic care facility rather than a private home (own or family/friends’ home) after rehabilitation at a specialised centre following spinal cord injury. Identifying these factors from the beginning of the rehabilitation process may inform the multidisciplinary rehabilitation team, patient, and their family in advance about the possible destinations at discharge. These data may also be interesting for social and healthcare services involved in the referral of patients to these centres, when needed.
Material and methodsStudy populationWe conducted a descriptive, retrospective study of all patients with traumatic spinal cord injury who completed an intensive rehabilitation programme at a centre specialising in this type of injury. The spinal cord injury unit for the Canary Islands, located at Complejo Hospitalario Universitario Insular Materno-Infantil in Gran Canaria (Spain), is the reference unit for these patients in the Canary Islands region. The region comprises 8 islands, with the 2 capital islands, Gran Canaria and Tenerife, being the most populated (859 835 and 933 402 inhabitants, respectively). According to the Canary Islands Statistics Institute, the population of the Canary Islands in 2018 was 2 177 000.14
Inclusion and exclusion criteriaThe study included all patients admitted to the spinal cord injury unit due to traumatic spinal cord injury (ICD-9 codes 806 and 952) between 1 January 2001 and 31 December 2018. We excluded patients who died at the unit or who were transferred to other units/hospitals before completing the rehabilitation programme, and patients younger than 15 years. Of 335 patients admitted during the study period, 9 died at the unit and 21 were transferred to their region or country of origin; therefore, the final sample included 305 patients.
Data sourcesData were extracted from the hospital database and the clinical records from patients’ stay at the unit. The lead author gathered data annually from the hospital records, compared data against those recorded by the admissions and transfers department, and was responsible for coding data throughout the study period. Despite this, the lack of a region-wide registry of hospitalised patients means that it was not possible to confirm the final destination of patients from the island of Tenerife, who would subsequently be transferred to a nursing home by the local hospital social services. The study was approved by the ethics committee of Complejo Hospitalario Universitario Insular Materno-Infantil (project code CEIm-CHUIMI-2017/969).
Study variablesData were collected on several categories of variable:
- -
Sociodemographic variables: age, sex, marital status, number of children, island of residence, living situation, level of study, and employment situation.
- -
Variables related to toxic substance use/medical history: smoking, alcohol, drugs, diabetes mellitus, arterial hypertension, ischaemic heart disease, and history of psychiatric disorder.
- -
Variables related to the spinal cord injury: year of injury, aetiology, workplace accident, vertebral fracture, fracture intervention, neurological lesion (complete quadriplegia, incomplete quadriplegia, complete paraplegia, incomplete paraplegia), type of injury, severity of injury (American Spinal Injury Association [ASIA] impairment scale15; Table 1), and bladder management at discharge.
Table 1.ASIA impairment scale.13
Degree of neurological lesion Clinical description A. Complete No sensory or motor function below the level of the injury, including segments S4–S5 B. Incomplete Sensory but not motor function is preserved below the neurological level, including segments S4–S5. C. Incomplete Motor function is preserved below the neurological level, including segments S4–S5, but more than half of muscles below the neurological level present strength less than 3. D. Incomplete Motor function is preserved below the neurological level, including segments S4–S5, and at least half of muscles below the neurological level present strength greater than 3. E. Normal All motor and sensory functions are unhindered. ASIA: American Spinal Injury Association.
- -
Hospital variables: time from injury to arrival at the spinal cord injury unit, duration of stay at the unit, and destination at discharge.
- -
Functional variables: total and domain scores on the Spinal Cord Independence Measure (SCIM, version III).16 Total and domain scores were divided into bands (every 5 points for self-care, every 10 points for respiration and sphincter management and for mobility, and every 20 points for total SCIM score).
To improve the precision of the multivariate analysis, variables were treated as binary. Thus, marital status was classed as married/partner vs other; living situation as own home (alone, with spouse, or with parents) vs other; smoking as daily or occasional vs ex- or non-smokers; alcohol consumption as toxic or daily vs other; drug use as hard and/or soft drug users vs non-users; psychiatric history as presence vs absence of psychiatric history; and island of residence as Tenerife vs other.
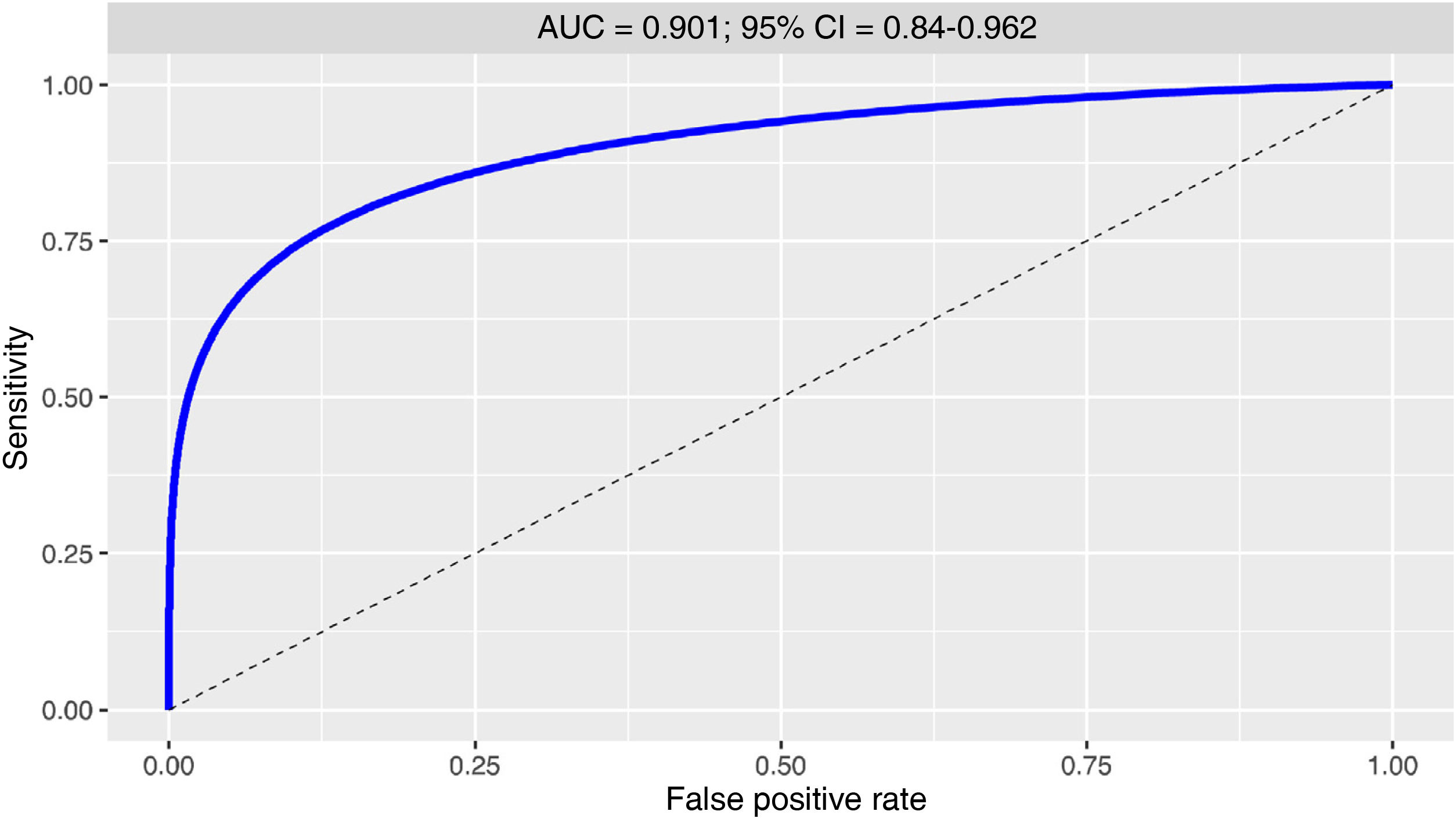
Statistical analysisCategorical variables are expressed as frequencies and percentages, and quantitative variables are expressed as means (standard deviation [SD]) if data were normally distributed and medians (percentiles 25 and 75 [p25–p75]) if not. We compared percentages using the chi-square test or the Fisher exact test, as appropriate, means with the t test, and medians with the Wilcoxon test for unpaired data. A multivariate logistic regression analysis was conducted to identify the factors independently associated with destination at discharge. The model included those variables showing a significant association with destination at discharge. Subsequently, variables were selected using the best subsets regression and Akaike information criterion methods. The model obtained is expressed as coefficients with standard error and P-values, and odds ratios (OR) with 95% confidence intervals (95% CI). From the logistic regression model, we calculated a predictive score, defined as the linear combination of variables from the logistic regression model. This score yields a rule to predict patient destination at discharge, as follows: a patient is considered likely to be transferred to a residential centre if and only if they score higher than a cut-off point C. Each cut-off point is associated with a sensitivity and specificity value. The receiver operating characteristic (ROC) curve is a graphical representation of sensitivity values against the corresponding false positive rates (1 – specificity). The discriminant capacity of the predictive rule was evaluated according to the area under the ROC curve. The optimal cut-off point was considered to be that with the smallest number of misclassified individuals (the point of the curve nearest the upper left corner):
For that optimal cut-off point, we calculated sensitivity and specificity with 95% confidence intervals. The threshold for significance was set at P< .05. Data were analysed using the R software package, version 3.5.1.17
ResultsTable 2 shows the results of the univariate analysis of the association between study variables and destination at discharge. The variables showing a significant association with discharge to a residential centre were: age, island of residence, marital status, previous living situation, employment status, history of smoking, history of alcohol use, type 2 diabetes mellitus, arterial hypertension, dyslipidaemia, history of psychiatric disorder, aetiology, time from injury to arrival at the spinal cord injuries unit, neurological lesion, ASIA classification, bladder management at discharge, and functional status (SCIM total score and domain scores).
Patient characteristics: overall and by destination at discharge (residential centre/private home).
| Overalln=305 | Destination | P | ||
|---|---|---|---|---|
| Residentialn=40 | Privaten=265 | |||
| Age (years) | 44.1±17.9 | 56.9±15.2 | 42.1±17.5 | < .001 |
| Male sex | 243 (79.7) | 34 (85.0) | 209 (78.9) | .369 |
| Lesion period | .107 | |||
| 2000−2005 | 106 (34.8) | 9 (22.5) | 97 (36.6) | |
| 2006−2010 | 70 (23.0) | 7 (17.5) | 63 (23.8) | |
| 2011−2015 | 83 (27.2) | 16 (40.0) | 67 (25.3) | |
| 2016−2018 | 46 (15.1) | 8 (20.0) | 38 (14.3) | |
| Island of residence | .009 | |||
| Tenerife | 66 (21.6) | 16 (40.0) | 52 (19.6) | |
| Gran Canaria | 169 (55.4) | 18 (45.0) | 151 (57.0) | |
| Other | 70 (23.0) | 6 (15.0) | 62 (23.4) | |
| Marital status | < .001 | |||
| Single | 119 (39.9) | 14 (36.8) | 105 (40.4) | |
| Married/partner | 139 (46.6) | 11 (28.9) | 128 (49.2) | |
| Separated/divorced | 29 (9.7) | 8 (21.1) | 21 (8.1) | |
| Widowed | 11 (3.7) | 5 (13.2) | 6 (2.3) | |
| Children | 0 (0−2) | 1 (0−2) | 0 (0−2) | .641 |
| Previous living situation | < .001 | |||
| Own home, living alone | 63 (21.0) | 16 (41.0) | 47 (18.0) | |
| Own home, living with partner | 142 (47.3) | 14 (35.9) | 128 (49.0) | |
| Parents’ home | 76 (25.3) | 3 (7.7) | 73 (28.0) | |
| Children’s home | 3 (1.0) | 1 (2.6) | 2 (0.8) | |
| Other relatives’ home | 9 (3.0) | 2 (5.1) | 7 (2.7) | |
| Friends’ home | 4 (1.3) | 0 | 4 (1.5) | |
| Other | 3 (1.0) | 3 (7.7) | 0 | |
| Level of education | .220 | |||
| None/primary study | 210 (76.4) | 32 (84.2) | 178 (75.1) | |
| Secondary/higher study | 65 (23.6) | 6 (15.8) | 59 (24.9) | |
| Employment status | < .001 | |||
| None | 33 (11.1) | 7 (17.9) | 26 (10.1) | |
| Student | 18 (6.1) | 0 | 18 (7.0) | |
| Employed | 158 (53.2) | 9 (23.1) | 149 (57.8) | |
| Unemployed | 11 (3.7) | 3 (7.7) | 8 (3.1) | |
| Retired | 42 (14.1) | 13 (33.3) | 29 (11.2) | |
| Disabled | 15 (5.1) | 4 (10.3) | 11 (4.3) | |
| Homemaker | 20 (6.7) | 3 (7.7) | 17 (6.6) | |
| Smoking | .039 | |||
| Daily smoker | 118 (38.7) | 23 (57.5) | 95 (35.8) | |
| Occasional smoker | 8 (2.6) | 0 | 8 (3.0) | |
| Ex-smoker | 18 (5.9) | 3 (7.5) | 15 (5.7) | |
| Non-smoker | 161 (52.8) | 14 (35.0) | 147 (55.5) | |
| Alcohol | .005 | |||
| Toxic levels | 35 (11.5) | 11 (27.5) | 24 (9.1) | |
| Daily | 26 (8.5) | 1 (2.5) | 25 (9.4) | |
| Occasional | 163 (53.4) | 18 (45.0) | 145 (54.7) | |
| None | 81 (26.6) | 10 (25.0) | 71 (26.8) | |
| Drug use | .429 | |||
| Hard drugs | 23 (7.5) | 3 (7.5) | 20 (7.5) | |
| Soft drugs | 23 (7.5) | 1 (2.5) | 22 (8.3) | |
| None | 259 (84.9) | 36 (90.0) | 223 (84.2) | |
| Type 2 diabetes mellitus | 24 (7.9) | 9 (22.5) | 15 (5.7) | .001 |
| AHT | 60 (19.7) | 14 (35.0) | 46 (17.4) | .009 |
| Ischaemic heart disease | 20 (6.6) | 7 (17.5) | 13 (4.9) | .008 |
| Dyslipidaemia | 39 (12.8) | 8 (20.0) | 31 (11.7) | .024 |
| History of psychiatric disorders | < .001 | |||
| Anxiety | 4 (1.3) | 2 (5.0) | 2 (0.8) | |
| Depression | 15 (4.9) | 3 (7.5) | 12 (4.5) | |
| Schizophrenia | 11 (3.6) | 4 (10.0) | 7 (2.6) | |
| Dementia | 3 (1.0) | 3 (7.5) | 0 | |
| Other | 5 (1.6) | 1 (2.5) | 4 (1.5) | |
| None | 267 (87.5) | 27 (67.5) | 240 (90.6) | |
| Workplace accident | 39 (12.8) | 2 (5.0) | 37 (14.0) | .114 |
| Aetiology | .006 | |||
| Traffic accident | 113 (37.0) | 8 (20.0) | 105 (39.6) | |
| Fall | 135 (44.3) | 28 (70.0) | 107 (40.4) | |
| Diving | 22 (7.2) | 2 (5.0) | 20 (7.5) | |
| Other | 35 (11.5) | 2 (5.0) | 33 (12.5) | |
| Time to admission, days | 17 (1−36) | 36 (21.5−63.2) | 14 (10−32) | < .001 |
| Hospital stay, days | 100 (52−150) | 108 (72−144) | 98 (48−150) | .296 |
| Lesion type | .199 | |||
| Complete | 139 (45.6) | 22 (55.0) | 117 (44.2) | |
| Incomplete | 166 (54.4) | 18 (45.0) | 148 (55.8) | |
| Neurological lesion | .017 | |||
| Complete quadriplegia | 54 (17.7) | 13 (32.5) | 41 (15.5) | |
| Incomplete quadriplegia | 100 (32.8) | 14 (35.0) | 86 (32.5) | |
| Incomplete paraplegia | 67 (22.0) | 3 (7.5) | 64 (24.2) | |
| Complete paraplegia | 84 (27.5) | 10 (25.0) | 74 (27.9) | |
| ASIA | < .001 | |||
| A | 133 (46.8) | 21 (52.5) | 112 (45.9) | |
| B | 18 (6.3) | 4 (10.0) | 14 (5.7) | |
| C | 46 (16.2) | 13 (32.5) | 33 (13.5) | |
| D | 78 (27.5) | 2 (5.0) | 76 (31.1) | |
| E | 9 (3.2) | 0 | 9 (3.7) | |
| Bladder management | < .001 | |||
| Intermittent catheterisation | 121 (40.9) | 7 (17.9) | 114 (44.4) | |
| Assistance for spastic bladder | 11 (3.7) | 1 (2.6) | 10 (3.9) | |
| Assistance for areflexic bladder | 9 (3.0) | 0 | 9 (3.5) | |
| Permanent catheter | 65 (22.0) | 29 (74.4) | 36 (14.0) | |
| Voluntary control | 90 (30.4) | 2 (5.1) | 88 (34.2) | |
| SCIM1 | < .001 | |||
| 0−5 | 68 (23.2) | 24 (61.5) | 44 (17.3) | |
| 6−10 | 28 (9.6) | 3 (7.7) | 25 (9.8) | |
| 11−15 | 27 (9.2) | 4 (10.3) | 23 (9.1) | |
| 16−20 | 170 (58.0) | 8 (20.5) | 162 (63.8) | |
| SCIM2 | < .001 | |||
| 0−10 | 5 (1.7) | 2 (5.1) | 3 (1.2) | |
| 11−20 | 71 (24.2) | 26 (66.7) | 45 (17.7) | |
| 21−30 | 46 (15.7) | 5 (12.8) | 41 (16.1) | |
| 31−40 | 171 (58.4) | 6 (15.4) | 165 (65.0) | |
| SCIM3 | < .001 | |||
| 0−10 | 87 (29.7) | 25 (64.1) | 62 (24.4) | |
| 11−20 | 108 (36.9) | 12 (30.8) | 96 (37.8) | |
| 21−30 | 48 (16.4) | 2 (5.1) | 46 (18.1) | |
| 31−40 | 50 (17.1) | 0 | 50 (19.7) | |
| SCIMtotal | < .001 | |||
| 0−20 | 39 (13.3) | 21 (53.8) | 18 (7.1) | |
| 21−40 | 46 (15.7) | 6 (15.4) | 40 (15.7) | |
| 41−60 | 35 (11.9) | 5 (12.8) | 30 (11.8) | |
| 61−80 | 95 (32.4) | 6 (15.4) | 89 (35.0) | |
| 81−100 | 78 (26.6) | 1 (2.6) | 77 (30.3) | |
Data are expressed as mean (standard deviation) or median (percentiles 25 and 75).
AHT: arterial hypertension; ASIA: American Spinal Injury Association; SCIM: Spinal Cord Independence Measure; SCIM1: SCIM self-care domain; SCIM2: SCIM respiration and sphincter management domain; SCIM3: SCIM mobility domain; SCIMtotal: total SCIM score.
The number of patients discharged to residential centres increased over the study period (9.14% of patients in 2001–2010 vs 18.4% in 2011−2018; P< .01). One of the variables showing the strongest associations was advanced age. In the group of patients younger than 30 years, none was discharged to a residential centre, whereas 10% of patients aged 31–45 years and 42.5% of those older than 75 years were discharged to these centres (P< .01).
The results of the multivariate analysis are shown in Table 3. Of 20 variables showing a significant association in the univariate analysis, 7 continued to show an association in the multivariate analysis: age (one-year increment), residence on the island of Tenerife, being married, smoking, type 2 diabetes mellitus, history of psychiatric disorder, and total SCIM score.
Multivariate logistic regression analysis of factors associated with discharge to a residential centre.
| Coefficient (SE) | Pa | AICb | OR (95% CI) | |
|---|---|---|---|---|
| (Intercept) | –3.397 (1.134) | – | – | – |
| Age, per year | 0.054 (0.015) | < .001 | 158.5 | 1.055 (1.025−1.087) |
| DM2 | 1.875 (0.762) | .013 | 149.9 | 6.518 (1.464−29.023) |
| Married/partner | –1.334 (0.540) | .010 | 150.4 | 0.264 (0.091−0.760) |
| Smoking | 1.238 (0.514) | .012 | 150 | 3.449 (1.260−9.443) |
| History of psychiatric disorders | 1.334 (0.540) | .014 | 149.8 | 3.796 (1.318−10.935) |
| Residence in Tenerife | 1.273 (0.506) | .011 | 150.2 | 3.573 (1.325−9.637) |
| SCIMtotal, by band | –0.725 (0.188) | < .001 | 161.3 | 0.484 (0.335−0.699) |
95% CI: 95% confidence interval; AIC: Akaike information criterion; DM2: type 2 diabetes mellitus; OR: odds ratio; SCIMtotal: total Spinal Cord Independence Measure score; SE: standard error.
The results of the logistic regression analysis were used to calculate the predictive score (linear combination of variables):
Fig. 1 shows the ROC curve for the predictive score for destination at discharge. The area under the curve was 0.901 (95% CI, 0.84−0.962). The optimal cut-off point was 1.028. Therefore, patients scoring higher than this value are considered likely to be discharged to a residential centre. The sensitivity and specificity of this predictor were calculated at 0.868 (95% CI, 0.763−0.947) and 0.813 (0.735−0.948), respectively.
Fig. 2 shows the discriminant power of the score. Example: consider a 41-year-old patient without diabetes (DM2=0), married (couple=1), a non-smoker (smoker=0), without psychiatric history (psych. hist.=0), from Gran Canaria (Tenerife=0), with a SCIMtotal=band 5. This patient’s score would be calculated as follows:
DiscussionCurrently, there is a general consensus that patients with acute spinal cord injury should be transferred as soon as possible to a unit specialising in these injuries. Several studies report that early transfer to specialised units improves patients’ functional status and independence and reduces the duration of hospitalisation, the number and severity of complications associated with the injury, and mortality rates, compared to management at non-specialised traumatology units.18–20 Furthermore, these units more effectively achieve another of the objectives of the management of these patients, with a greater percentage of patients discharged to private homes and, therefore, reintegrated into the community.21
While destination at discharge after hospitalisation for traumatic spinal cord injury has been widely studied in the United States,9,22 Australia,11 Canada,7 and the United Kingdom,10 no recent information is available for our setting. In our study, 86.8% of patients returned to their social/family environment. A similar percentage was reported in the Australian study (86.2%)11 and in other similar studies, with rates between 80% and 95%.8,22
We identified several factors influencing whether patients were discharged to a private home (own home or with a spouse, family members, or friends) or a residential centre after completing rehabilitation at our specialist spinal cord injury centre. Recent studies report an increase in the number of patients discharged to chronic care facilities.22,23 Another study by our group found that between 2001 and 2005, 8.5% of patients were discharged to chronic care facilities; this percentage increased significantly, reaching 20% in the period 2011−2015.3 The present study shows that this upward trend has continued. This increase may be due to the change observed in the target population, with a predominance of older individuals, mainly with incomplete cervical spinal cord injuries resulting from falls.3,5
We found destination at discharge to be significantly associated with several variables related to sociodemographic factors (age, marital status, living situation, and employment status), history of disease or toxic substance use (tobacco, alcohol, diabetes mellitus type 2, arterial hypertension, dyslipidaemia, ischaemic heart disease, stroke, psychiatric disorders), spinal cord injury (aetiology, ASIA classification, neurological lesion, and time to admission), and functional status at discharge (bladder management, SCIM domain scores, and total SCIM score). The variables that continued to show an independent association with destination at discharge were included in the multivariate regression (Table 3). Age was identified as a predictive factor, with a 0.054 increase in risk of discharge to a chronic care facility for each one-year increment. This is consistent with reports from the 1990s and early 2000s.7,22,24 Hsieh et al.25 reported that only 2% of patients younger than 30 years were discharged to these centres, compared to 17.2% among those older than 60. Those authors found an association with lower scores on the Functional Independence Measure at admission and at discharge, due to typically more severe neurological lesions (incomplete quadriplegia) and lower capacity to benefit from the programme, respectively.25,26 DeVivo et al.6 report similar figures, with 1.4% of patients aged 16–30 years and 22.2% of those older than 75 years being discharged to residential centres (2.6% and 18.4%, respectively, in our own study).6 Due to the increase in the mean age and life expectancy of patients with spinal cord injuries, greater emphasis should be placed on providing specific resources to this population, which we may expect to grow if the current trend continues.
History of disease prior to injury was also associated with destination at discharge; this was clearly observed in the univariate logistic regression analysis and subsequently confirmed in the multivariate regression for smoking, type 2 diabetes mellitus, and history of psychiatric disorder. Although these variables may be influenced by age, health awareness is also greater today; this is well-rooted in different sectors of society, and is associated with work activity or level of education.27 In our sample, 5.6% of economically active and 21.5% of non-active patients were transferred to residential centres (P< .01). In contrast, no significant difference was observed in association with level of education, with 15.2% of individuals with no education or primary study only and 9.2% of those with secondary or further education being discharged to these centres. The association with history of disease and toxic substance use is an interesting finding, as this question has not been explored in previous studies.
Another peculiar finding, which is similar to those reported in studies conducted at units serving multiple islands or large territories,11 is the percentage of patients transferred to a hospital nearer their home prior to discharge to a residential centre; in our study, these patients resided on the island of Tenerife. The reason for this is that these patients were able to complete rehabilitation therapy at a centre (with the capacity to manage its own health and social care resources) on their island, closer to their social/family setting, from which they were subsequently transferred to a chronic care facility.
Living with a partner decreased the likelihood of discharge to a residential centre (OR=0.264; 95% CI, 0.091−0.760). Although healthcare is universally and freely provided under the Spanish public health system, social care resources are limited, and insufficient home assistance is available for individuals with significant disability who live alone. If the patient’s close family and friends are unable to provide the additional care they need, the only option is to transfer them to a nursing home or chronic care facility. Living with a partner is probably a substitute for social support available in the patient’s home and general setting.
Finally, and as expected, higher total SCIM score was associated with greater likelihood of discharge to a private home. This reflects how, as reported in other studies, low SCIM scores are associated with the need for proportionally greater daily assistance. The same is the case for spinal cord lesion severity: greater severity (ASIA classification or type of neurological lesion) is associated with greater care needs and, consequently, a greater risk of discharge to a residential centre.11
Study limitationsThis study presents several limitations that prevent extrapolation of our results and conclusions. Each country, and each region within a country, presents specific characteristics that depend both on health and social care systems and on population and geographical factors. Our unit serves an archipelago of 8 islands, in which the only rapid, effective connection is by air transport; this may have led to differences in rehabilitation time, depending on each patient’s island of origin. Therefore, patients from Tenerife (the other capital of the Canary Islands), which has a separate social care system, may be over-represented due to initial discharge to a hospital on their island, and subsequently to the final destination, which may not always have been a residential care centre. Despite some missing data, we believe that a small proportion of these patients were finally discharged to a private home. To confirm this theory and to correct for this small bias, we would need to establish the final place of residence of each patient, several months after hospital discharge.
Another limitation may be the fact that, although the same healthcare, rehabilitation, and social care resources were available for all patients, we did not gather data on other variables that may have had a significant influence on the analysis performed. For instance, outcomes may have been influenced by potential financial compensation after traffic or workplace accidents, the disposable income of each patient, or the specific characteristics of their setting: rural/urban, accessible/architectural barriers, etc.
ConclusionsAccording to our results, advanced age, residence on the island of Tenerife, not being married, smoking, type 2 diabetes mellitus, history of psychiatric disorder, and low total SCIM score were predictive of discharge to a residential centre, with high sensitivity and specificity. The trend over the years has been an increase in the age and number of comorbidities observed in patients with spinal cord injury, with more limited social and family settings. In this context, it seems logical to suppose that the referral of these patients to residential or chronic care centres will continue to increase in the coming years. Understanding the factors associated with discharge into the community or to a residential or chronic care centre has several benefits. For the members of the multidisciplinary team working directly in the rehabilitation programme, this information would help to enable more realistic planning of treatment objectives and, together with the patient and their family, to plan the destination at discharge and the adaptations or assistance needed. For health and social care systems, this information would help improve the efficiency of planning and resource allocation to meet the needs of this population.
Publication ethicsThis retrospective study was approved by the research ethics committee of Complejo Hospitalario Universitario Insular Materno-Infantil (project code CEIm-CHUIMI-2017/969). The study complies with the ethical guidelines of the World Medical Association and the Declaration of Helsinki.
FundingThis study received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Author contributionsAll authors contributed substantially to:
- -
Study design and conception, data acquisition, or data analysis and interpretation
- -
Manuscript drafting or critical review of the intellectual content
- -
Approval of the final version.