A number of chronic neurological diseases may provoke changes in the clinical course of gestation or puerperium.1 In addition, the physiological changes involved in these states may entail potential risks for developing new neurological pathologies. These include neurological diseases of vascular origin, which have a significant incidence rate. We present the case of a 34-year-old puerperal patient with no relevant personal history who experienced sudden-onset dyspnoea, headache, and epileptic seizure.
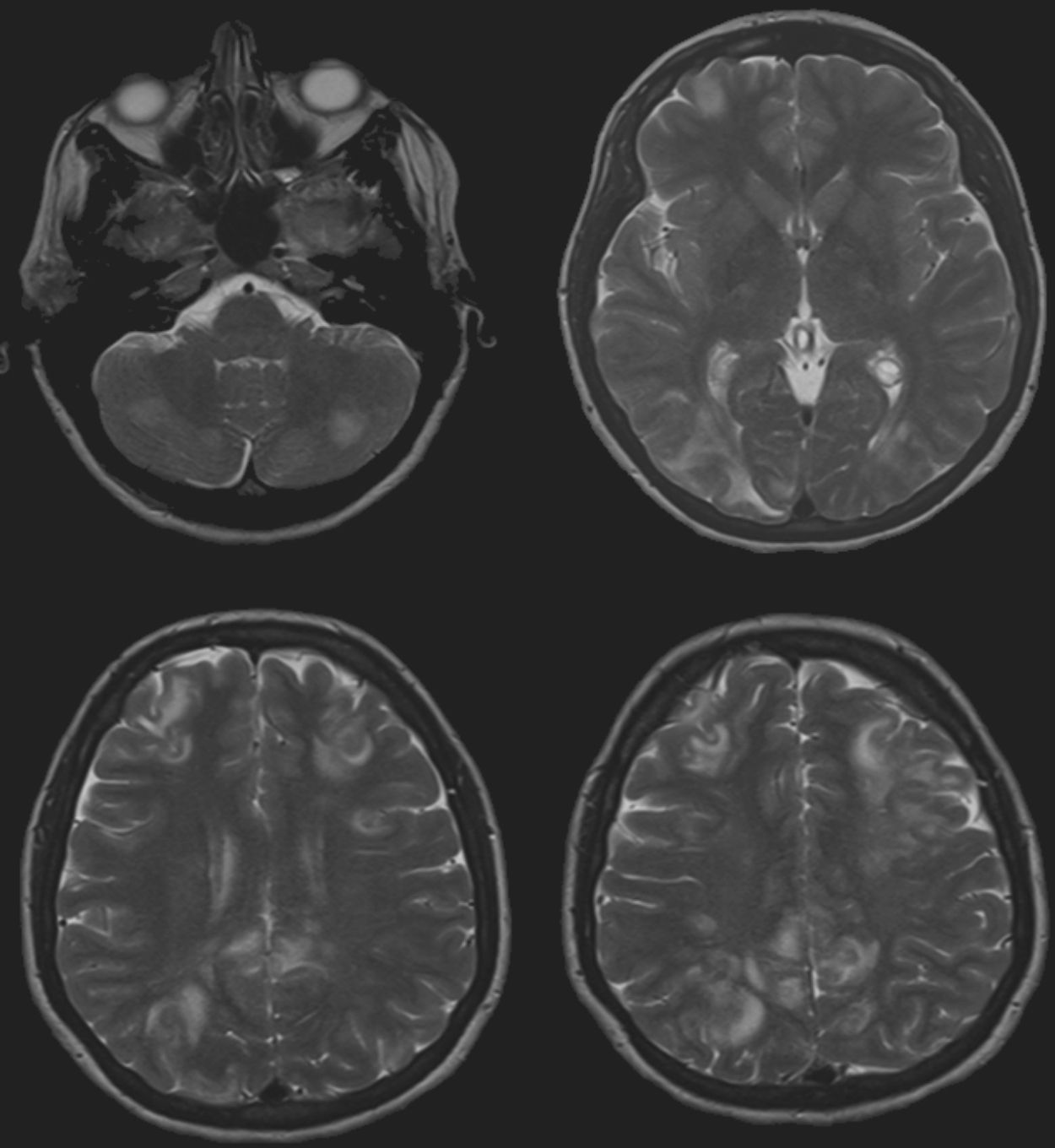
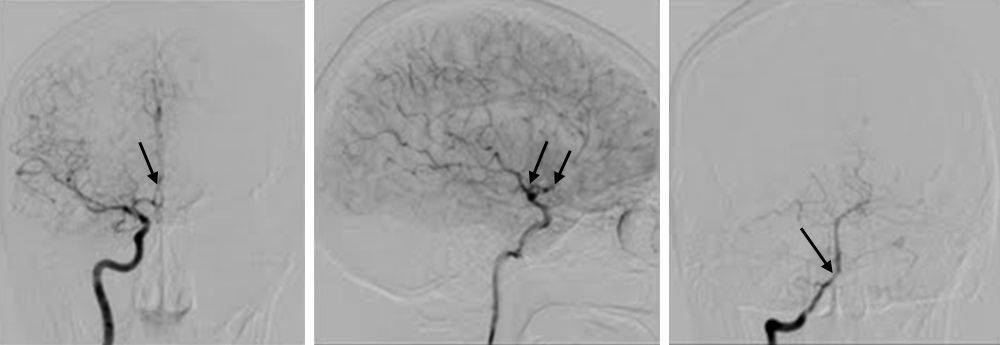
Pregnancy and normal vaginal delivery transpired without complications. The patient presented with dyspnoea and generalised oedema in conjunction with a holocranial thunderclap headache. The patient experienced an occipital seizure (seeing bright colours in the right visual hemifield followed by loss of consciousness and generalised tonic–clonic convulsions). Doctors then ordered a brain MRI that revealed hyperintense lesions in T2-weighted sequences in the territory of the posterior cerebral artery and asymmetrical lesions in the basal ganglia. The full work-up comprised a lumbar puncture, serology, and immunology studies, which all showed normal results. Five days later, the patient experienced an additional focal seizure. A new MRI (Fig. 1) revealed further lesions in the vascular watershed territory in addition to the previously identified lesions. The patient was suspected of having a generalised cerebral vasospasm, which was confirmed by arteriography (Fig. 2). Nimodipine was administered during 21 days and most of the lesions resolved. The patient was asymptomatic upon discharge. A routine arteriography performed 3 months later confirmed complete resolution of the vasoconstriction.
Axial T2. Patchy, hyperintense areas in both cerebellar hemispheres, the right parietal–occipital lobes and bilateral frontal lobes, predominantly in the subcortical region and affecting the cortex without causing thickening. Distribution of the lesions in the vascular watershed territory.
Reversible cerebral vasoconstriction syndrome (RCVS) is an uncommon pathology of unknown aetiology, which has been associated with pregnancy/puerperium,2 and the use of certain drugs. This syndrome presents with thunderclap headache and variable focal neurological signs, which are predominantly occipital.3 Cranial MRI may reveal ischaemic or haemorrhagic lesions in different areas; however, the diagnostic test of choice is arteriography, which shows areas of constriction and dilation in different vascular beds. Resolution of these alterations after 12 weeks2 is considered a diagnostic criterion. Differential diagnosis must rule out other causes of sudden-onset thunderclap headache and focal neurological signs,2,4 such as arterial dissection, venous sinus thrombosis, subarachnoid haemorrhage, and isolated vasculitis of the central nervous system.
Treatment approaches are controversial and they include use of calcium channel blockers, corticosteroid bolus, magnesium sulphate, and even clinical observation. However, none of them has been shown to be more effective than another. In cases associated with use of drugs, those drugs must be discontinued. Prognosis for this syndrome is good since the arterial disorder and most of the lesions are reversible. Nevertheless, if vasospasm is present for a prolonged period of time, ischaemic or haemorrhagic infarcts and permanent focal lesions may occur.
In the present case, the patient sought medical assistance due to dyspnoea and oedema, which may indicate that vasospasm was systemic. The literature does not include any cases that might support this theory.
Although this syndrome is rare, it should be considered where symptoms are compatible. A strong clinical suspicion can deliver an early diagnosis that may prevent potentially fatal complications.