Contradictory data have been reported on the incidence of stroke in patients with COVID-19 and the risk of SARS-CoV-2 infection among patients with history of stroke.
MethodsThis study systematically reviews case series reporting stroke as a complication of COVID-19, and analyses the prognosis of patients with COVID-19 and history of stroke. The pathophysiological mechanisms of stroke in patients with COVID-19 are also reviewed.
ConclusionsHistory of stroke increases the risk of death due to COVID-19 by 3 times. Stroke currently seems not to be one of the main complications of COVID-19.
Existe información contradictoria acerca de la incidencia de ictus en enfermos de COVID-19 y sobre el riesgo de los enfermos con antecedentes de ictus de padecer la pandemia.
MétodosRevisión sistemática de la bibliografía sobre las series de casos de COVID-19 que han tenido un ictus como complicación y sobre el pronóstico de los enfermos con antecedentes de ictus que sufren COVID-19. También se han revisado los mecanismos por los que se pueden producir ictus en esta enfermedad.
ConclusionesTener antecedentes de ictus aumenta 3 veces el riesgo de fallecer por COVID-19. En este momento el ictus no parece una de las complicaciones principales de COVID-19.
Since the beginning of the COVID-19 pandemic, contradictory findings have been reported regarding the incidence of stroke in patients with the disease and the risk of SARS-CoV-2 infection among patients with history of stroke.
MethodsA systematic review analysed series of patients presenting stroke as a complication of COVID-19 and the prognosis of COVID-19 in patients with history of stroke. Pathogenesis of stroke in patients with COVID-19 is also addressed.
A systematic search was performed of the MEDLINE (PubMed search tool) and Embase® databases. The search strategy used the following Medical Subject Headings indexing terms: (cerebrovascular disorders OR stroke OR cerebral haemorrhage OR blood coagulation disorders OR myocardial infarction) AND (SARS-CoV-2 OR Coronavirus infections OR COVID-19 OR SARS virus OR Middle East Respiratory Syndrome Coronavirus). The search returned 78 articles. The following searches were also performed: “Plaque, atherosclerotic” AND “Virus diseases” (165 results); “Autopsy” AND “Coronavirus infection” (90 results). The Embase® search identified 25 articles that were not found on MEDLINE. The review was expanded by including relevant articles from the reference lists of the articles found. This review does not address other neurological complications of COVID-19, besides stroke.
ResultsBefore 2003, acute infection with different coronaviruses was known to cause congestion of the upper respiratory tract; these viruses are endemic, and their relationship with several chronic neurological diseases are currently under study.1 Since then, 3 new coronaviruses have caused epidemics of respiratory syndromes with high mortality rates, which are occasionally associated with neurological complications. The 2003 epidemic was caused by the SARS-CoV virus, the 2012 epidemic by the MERS-CoV virus, and the current epidemic (COVID-19), which began in Wuhan (China) in December 2019, was caused by the novel coronavirus SARS-CoV-2. During the 2003 SARS-CoV epidemic, a series of 206 cases in Singapore included 5 cases of large-vessel stroke2; a case series from Taiwan (664 patients) included 5 cases.3 Hypercoagulability, caused either by the disease itself or by immunoglobulin treatment, was proposed as a possible cause of stroke. Autopsies performed during the 2003 epidemic revealed venous thrombosis, inflammation, and fibrinoid necrosis of small vessel walls in many organs, including the lungs, heart, and brain.4 The virus has been detected in the cerebrospinal fluid with polymerase chain reaction testing5 and in neurons and glial cells with in situ hybridisation and electron microscopy.6,7 During the 2012 MERS-CoV epidemic, patients with respiratory symptoms occasionally presented stroke, intracranial haemorrhage,8 acute disseminated encephalomyelitis, or encephalitis. As the virus was not detected in the cerebrospinal fluid or in brain tissues, neurological complications were thought to be immune-mediated.9
The novel coronavirus SARS-CoV-2 presents a genetic similarity of 79.5% with SARS-CoV and 96% with the bat SARS-like coronavirus.10 Similarly to other coronaviruses, it can access the nervous system via the haematogenous route or by retrograde axonal transport; the latter mechanism probably explains the frequent association with anosmia. Before entering cells, the virus binds to the ACE2 receptor,11 which is present in many types of human cells.
Because the disease originated in China, the only case series of COVID-19 published to date include Chinese patients.12–24 Of these series, only the first 4 analyse complications or causes of death; only one of these reviewed neurological manifestations and complications, including stroke. This case series12 analyses 214 patients presenting SARS-CoV-2 infection in January and February 2020, 78 (36.4%) of whom presented one or more of the following neurological manifestations: dizziness, headache, impaired consciousness, stroke, ataxia, seizures, anosmia, visual alterations, neuropathic pain, and muscle damage. Stroke was reported in 2.8% of the total cohort, occurring in 5.7% of patients with severe respiratory infection (4 ischaemic and one haemorrhagic stroke) and 0.8% of those with less severe symptoms (one ischaemic stroke). Two of the 6 patients with stroke attended hospital due to hemiplegia and were incidentally found to have pneumonia secondary to SARS-CoV-2 infection at admission, having presented no respiratory symptoms previously. Although the median time between onset of respiratory symptoms and stroke was 10 days, stroke occurred 1-2 days after hospitalisation in most cases. Patients with severe neurological damage had higher D-dimer levels than other patients, and presented greater immunosuppression caused by the virus, demonstrated by the lower lymphocyte count.
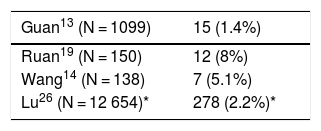
The second issue addressed in this study is whether history of stroke increases the risk of developing COVID-19 or the severity of symptoms. One of the earliest studies, which included 99 patients admitted from 1 to 20 January 2020 in Wuhan, reported history of cardiovascular or cerebrovascular disease in 40% of patients.25 Different COVID-19 case series report different percentages of patients with history of stroke (Table 1); if we combine the data from all series,13,14,19 the percentage of patients with history of stroke shows little difference from that reported in a previous sample of the Chinese general population (2.2%).26
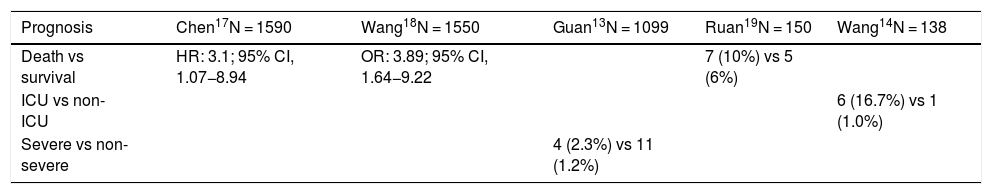
In all the case series studied, history of stroke was associated with poorer progression of COVID-19. In a cohort of patients from 55 hospitals, history of stroke was twice as frequent among patients classified as having severe COVID-19 than among patients with mild symptoms.13 In a smaller series, only one of 7 patients with history of stroke was not admitted to intensive care.14 Combined data from patient series from hospitals across China, including more than 1500 patients, shows that history of stroke is associated with a three-fold increase in the risk of death (Table 2).17,18
Association between history of stroke and prognosis.
| Prognosis | Chen17N = 1590 | Wang18N = 1550 | Guan13N = 1099 | Ruan19N = 150 | Wang14N = 138 |
|---|---|---|---|---|---|
| Death vs survival | HR: 3.1; 95% CI, 1.07−8.94 | OR: 3.89; 95% CI, 1.64−9.22 | 7 (10%) vs 5 (6%) | ||
| ICU vs non-ICU | 6 (16.7%) vs 1 (1.0%) | ||||
| Severe vs non-severe | 4 (2.3%) vs 11 (1.2%) |
CI: confidence interval; HR: hazard ratio; ICU: intensive care unit; OR: odds ratio.
While history of cardiovascular disease and risk factors are not the main focus of this review, we should note that, like history of stroke, they are associated with poorer prognosis of COVID-19. The largest, most recent Chinese register, which includes 72 314 patients with COVID-19, reports a mortality rate of 2.3% globally, 10.5% in patients with history of cardiovascular disease (including stroke), and 7.3% in patients with diabetes.20
SARS-CoV-2 may cause stroke by several mechanisms: invasion of vessel walls, coagulation disorders, cerebral embolism secondary to myocardial damage, or destabilisation of an existing atheromatous plaque. The virus is able to invade vessel walls because endothelial cells express the ACE2 receptor, which the virus uses to enter cells; SARS-CoV-2 has been detected in the endothelium.27 When it invades vessel walls, it may behave similarly to the varicella zoster virus, the most frequent viral cause of stroke, triggering inflammation and even necrosis of the walls of cerebral arteries.28
Another potential mechanism by which SARS-CoV-2 may cause stroke is by interfering with coagulation. Respiratory infection with Streptococcus pneumoniae or influenza virus is known to increase the incidence of myocardial infarction and stroke; the influenza vaccine partially prevents the occurrence of these events.29,30 Cytomegalovirus can also cause venous thrombosis by damaging vessel walls or inducing antiphospholipid antibody production.31 Viruses can cause thrombosis by activating the immune system, which affects coagulation, platelet activation, and endothelial function.32 The general inflammatory status or “cytokine storm” that SARS-CoV-2 causes in some patients may alter coagulation, increasing D-dimer levels and procoagulant activity.12,33,34 Patients with D-dimer levels above 1 μg/mL are nearly 20 times more likely to die.15 Pulmonary embolism and venous thrombosis of various tissues are even more frequent than arterial thromboses.35
As occurred in the 2003 SARS epidemic,36 the SARS-CoV-2 virus can damage the heart, which may in turn lead to cardioembolic stroke. Acute myocardial damage, detected by presence of elevated troponin levels, was detected in 15% of patients in one series16 and in 17% in another, in which it was also associated with morbidity and mortality37; in a third study, 16.7% of patients developed arrhythmic complications, with 7% presenting acute myocardial infarction.14 Seven percent of deaths were attributed to myocarditis.19
The systemic inflammation caused by SARS-CoV-2 may also cause stroke through destabilisation of atheromatous plaques, as is thought to occur during influenza epidemics. Systemic inflammation ruptures the fibrous cap of the atheroma, exposing the thrombogenic material.38 This hypothesis was proposed as an explanation for acute coronary syndromes observed during the 2003 SARS-CoV epidemic.39 Systemic inflammation may activate the endothelium40 and result in failure of thrombolytic treatment for myocardial infarction.41
Finally, rates of morbidity and mortality due to stroke may present a discreet increase as a result of such indirect mechanisms as patients’ fear of attending hospital or the fact that nearly all hospital resources are occupied in caring for patients with COVID-19. This has resulted in longer cardiac and cerebrovascular reperfusion times,42,43 which has led professional organisations to issue recommendations on adapting the treatment of stroke44,45 and myocardial infarction46 during the pandemic. Stroke incidence may also increase because of decreased monitoring of cardiovascular risk factors as a result of reduced healthcare provision47 and lockdown measures.48
Limitations
The findings from this review should be considered provisional: given how recently the pandemic started, few clinical series have been published; all those published studies include only Chinese patients and place little emphasis on stroke. The saturation of hospitals and limitations to patients’ mobility may have prevented patients with history of stroke from reaching hospital, distorting data on the percentage of these patients with confirmed SARS-CoV-2 infection and on mortality rates.
ConclusionsHistory of stroke is associated with a three-fold increase in the risk of death due to SARS-CoV-2 infection. Stroke currently seems not to be one of the main complications of COVID-19. The virus enters the brain parenchyma, endothelium, and heart, and alters coagulation, which may lead to stroke; we must therefore remain vigilant. Patients with stroke may concomitantly present SARS-CoV-2 infection, even if they have not previously shown respiratory symptoms.
Conflicts of interestNone.
FundingNone.
Please cite this article as: Trejo Gabriel y Galán JM. Ictus como complicación y como factor pronóstico de COVID-19. Neurología. 2020;35:318–322.