Subarachnoid haemorrhages (SAH) are responsible for 6% to 8% of all acute cerebrovascular events, 5% of deaths, and 25% of the potential life years lost. Their importance lies in the fact that they tend to affect younger patients than ischaemic stroke and result in high morbidity and mortality rates. In addition, a SAH is both a pathological process in itself and an epiphenomenon of an underlying disease that must be treated.1–5 We present the case of a patient with aneurysmal SAH (aSAH) manifesting with intermittent symptoms who was found to have mirror aneurysms in both middle cerebral arteries (MCA).
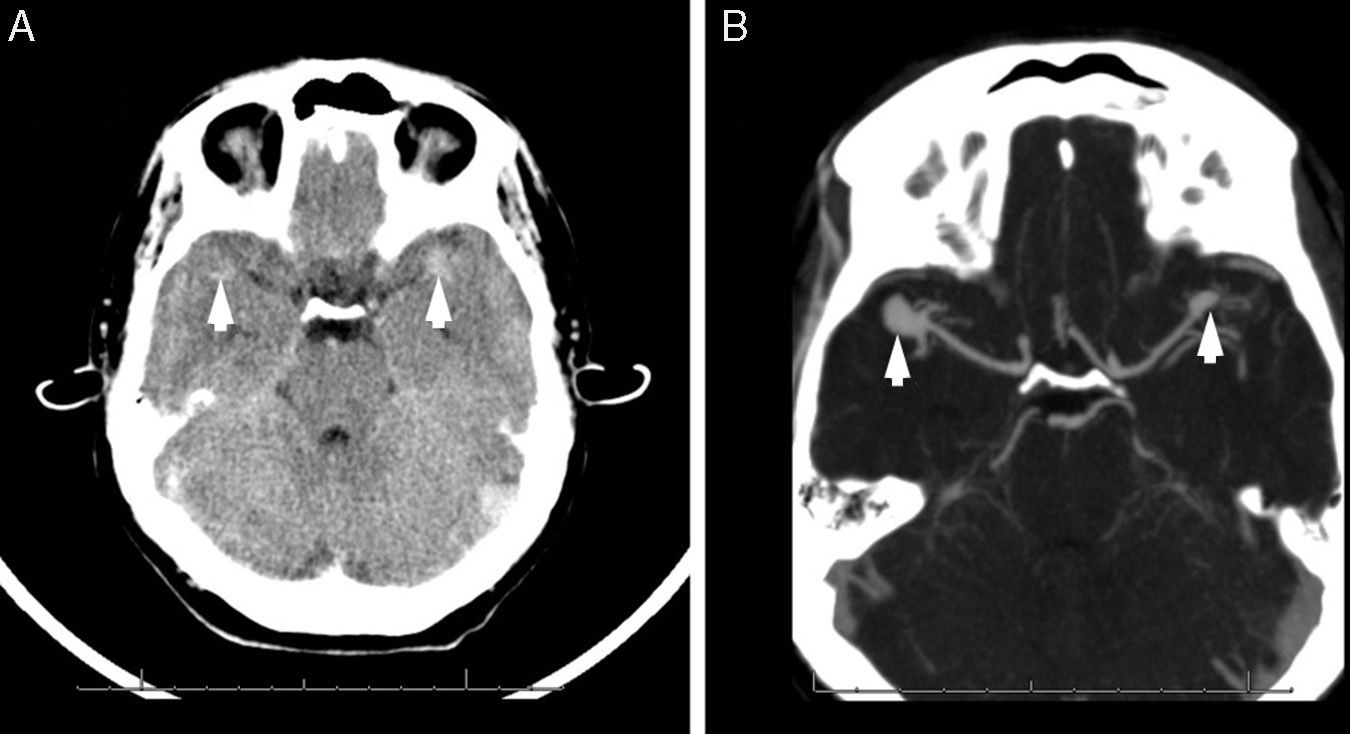
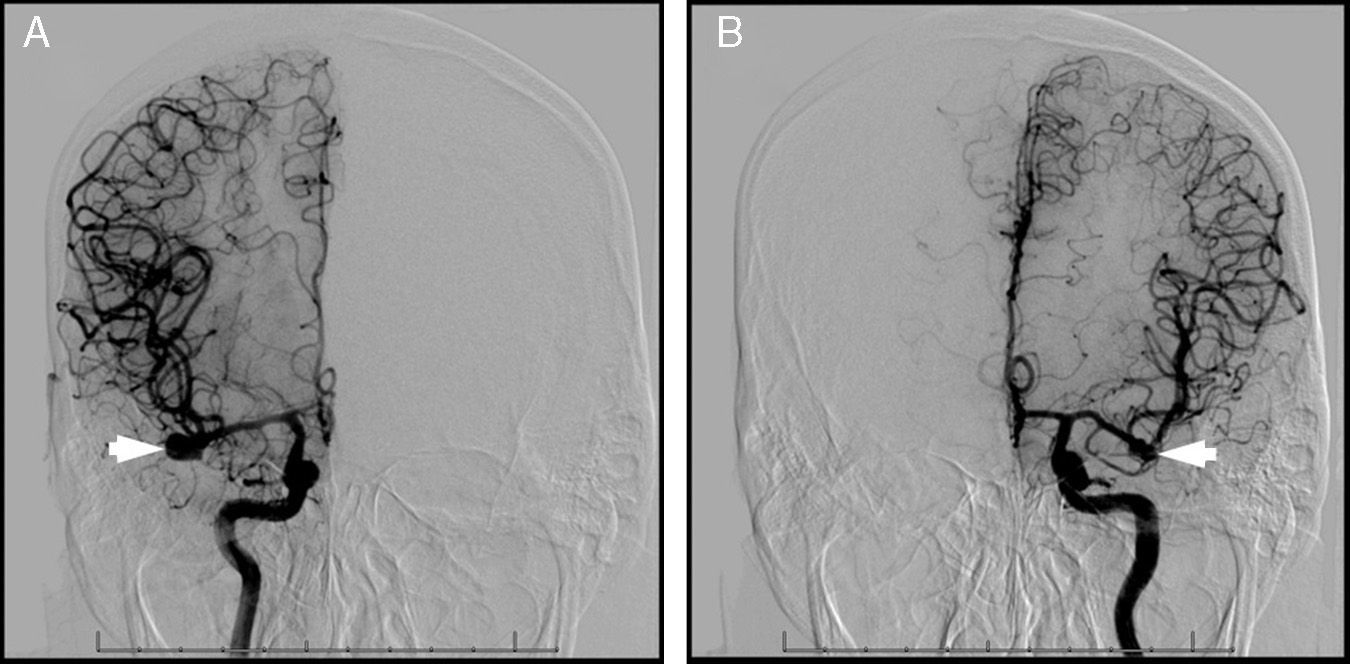
Our patient was a 42-year-old man who presented at the emergency department with fluctuating non-traumatic clinical symptoms consisting of a holocranial headache of moderate intensity, which had started 4 days previously while he was playing volleyball. The headache was self-limiting but later reappeared in association with presyncopal symptoms and meningismus. The patient described the headache as ‘the worst headache of his life’. Suspicion of aSAH led to a request for an urgent brain CT scan and a general blood test. The blood test yielded normal results and the CT scan revealed an aSAH (Fig. 1A). The vascular study also included an intracranial CT angiography (Fig. 1B), which showed an aneurysm on each MCA (distal M2 segment). The haemorrhage was attributed to the aneurysm on the left MCA, which was confirmed by cerebral arteriography (Fig. 2). The patient was diagnosed with aSAH (Hunt & Hess grade 1, WFNS grade 1, Fisher grade 3). After starting on oral nimodipine 60mg/4h, our patient was admitted and underwent an emergency pterional craniotomy (clipping the aneurysm on the M2 segment of the left MCA); the same procedure was repeated for the unruptured aneurysm on the right MCA 30 days later. The clinical and radiological outcomes were favourable, and the patient recovered ad integrum.
(A) The CT scan (axial slice) shows foci of subarachnoid haemorrhage with an aneurysmal pattern in both Sylvian fissures (more marked on the left side). Areas of increased focal density with pseudonodular morphology may be seen in both MCAs, suggesting either a haemorrhagic component or aneurysms (arrowheads). (B) Intracranial CT angiography showing the circle of Willis (axial slice): 2 saccular aneurysms can be seen in the MCAs (arrowheads). An aneurysm measuring 11mm×9mm with a 5-mm neck can be seen in the right MCA (at M2 bifurcation). An aneurysm measuring 8mm×4.5mm with a neck of 1 to 2mm can be seen in the left MCA (also in the most distal portion of the M2 segment).
(A) A digital subtraction angiography (anteroposterior projection) with selective contrast injection into the right internal carotid artery confirms the presence of an unruptured aneurysm in the M2 segment of the right MCA (arrowhead). (B) A digital subtraction angiography (anteroposterior projection) with selective contrast injection into the left internal carotid artery reveals the presence of an aneurysm in the M2 segment of the left MCA (arrowhead). The aneurysm has irregular lobulated contours suggesting a rupture, which points to this aneurysm being the one responsible for the SAH.
Despite the many achievements in SAH diagnosis and treatment, SAH is still a serious entity: 10% of patients die before arriving at the hospital, 25% die within the first 24hours after bleeding, 45% die within the following 30 days, 50% present sequelae, and only 33% achieve good outcomes after treatment.1–5 The incidence of ruptured intracranial aneurysms increases with age (≥60 years) and aneurysm size (≥5mm), and is greater in women, patients with posterior circulation aneurysms, and symptomatic patients. In order of frequency, intracranial aneurysms are located in the anterior communicating and anterior cerebral arteries (35%), the middle cerebral artery (25%), the posterior communicating artery (22%), and arteries of the posterior circulation (18%). Between 15% and 33.5% of patients with SAHs have multiple aneurysms.1–4,6 Mirror or twin aneurysms, a rare subtype of multiple aneurysms, account for 5% to 10% of all aneurysms and 36% to 40% of multiple aneurysms. Although they may appear in any intracranial vessel, they are more frequently located in the MCA and their embryologic origin is different from that of typical saccular aneurysms. Patients with mirror aneurysms have a congenital predisposition to weakness of the aneurysmal wall which promotes earlier rupture. Its aetiopathogenesis is based on the fact that the intracranial vascular system comprises multiple segments, each of which has its own genetic identity, which makes them vulnerable to specific triggers (arterial hypertension, tobacco, etc.). During brain angiogenesis, a defect in cell migration may be transmitted to the next generation of cells, leading to a clonal distribution of that defect. In this way, the synchronous presence of several abnormal segments may result in the formation of mirror aneurysms.7–10 Regarding neuroimaging techniques, after finding an SAH with a conventional CT scan we suggest performing a CT angiography, as it provides high-quality data on the topography and angioarchitecture of the aneurysm, which is extremely useful if the patient's neurological state worsens before performing a cerebral arteriography.1–3,11,12 Regarding treatment, the aneurysm responsible for the SAH must be treated as soon as possible (whether with surgery or endovascular treatment, depending on the characteristics of the patient and the aneurysm), whereas the contralateral aneurysm may be treated at that same intervention or at a later stage.13,14
Headaches appear in up to 97% of cases and are usually the leading symptom of SAH. Sentinel headaches, which occur in 30% to 50% of patients with spontaneous SAH, subside within a few hours. As symptoms appear to be benign and non-organic, patients either do not seek medical attention or are not thoroughly examined. Headache may be due to microbleeding, sudden growth of an aneurysm, or intramural haemorrhage secondary to an aneurysm. Recognising this event is essential as it may precede a more severe haemorrhage.1–3,5,11,15 We therefore recommend including aSAH in the differential diagnosis of intermittent headache, especially when mirror aneurysms are found, since delays in diagnosis and treatment may leave irreversible sequelae and lead to a significant increase in the potential life years lost.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank Drs Santiago Cepeda Chafla, Miguel Ángel García Soldevilla, Laura Izquierdo Esteban, Carla Sonsireé Abdelnour Ruiz, María Molina Sánchez, and María Henedina Torregrosa Martínez.
Please cite this article as: León Ruiz M, Lagares Gómez-Abascal A, Fernández Alén JA, Benito-León J, García-Albea Ristol E. Hemorragia subaracnoidea por rotura de aneurisma especular intracraneal. A propósito de un caso y revisión de la literatura. Neurología. 2016;31:283–285.