Unlike in other natural disasters, patients have avoided visiting healthcare facilities during the COVID-19 pandemic as these settings have become a major focus of infection. The same phenomenon was observed during the SARS-CoV and MERS-CoV outbreaks in 2003 and 2012, respectively.1 This, combined with the risk of exacerbation of neurological diseases associated with SARS-CoV-2 infection,2,3 results in more pronounced worsening of chronic diseases. In this scenario, telemedicine represents an extremely useful tool.4,5 In the case of epilepsy, and given the characteristics of these consultations, which are mainly based on clinical history and assessment of symptoms, telemedicine has been shown to be effective for follow-up of these patients.6 In a recent interview on the subject, Dr Jacqueline French (NYU Langone Medical Center, New York) argued that assessment of epileptic patients can be successfully completed in remote consultations in 99% of cases.7
However, the current scenario has increased the risk of treatment discontinuation among patients with epilepsy. To date, only one study has been published on the topic in the context of confinement due to coronavirus disease. In 2005, Shung-Lon et al.1 published their observations on the impact of confinement on epilepsy drug withdrawal in Taiwan during the 2003 SARS outbreak. The study included 227 patients who were evaluated via telephone consultation between 16 May and 2 June 2003. Many patients could not be contacted, although the exact number is not disclosed. Forty-nine discontinued treatment without consulting their physicians; 28 of this group presented seizures. Interestingly, more patients remained seizure-free during confinement than in the 6 months prior (125 vs 117; P=.05).
The purpose of this study was to evaluate follow-up of patients with epilepsy during confinement and to compare it against the previous 7 months.
We contacted a total of 62 patients with epilepsy by telephone between confinement days 6 and 30 in Spain (20 March to 13 April 2020). Thirteen of these were excluded from our sample, for the following reasons: surgery or severe intercurrent processes (3 cases), epilepsy history of less than 6 months’ duration prior to confinement (2), seizure frequency of =7 per day (2), hospitalisation due to COVID-19 (1), death (1), factitious disorder (1), change of hospital (1), inability to contact the patient (1), and hospitalisation during confinement (1). A total of 49 individuals were finally included in our analysis.
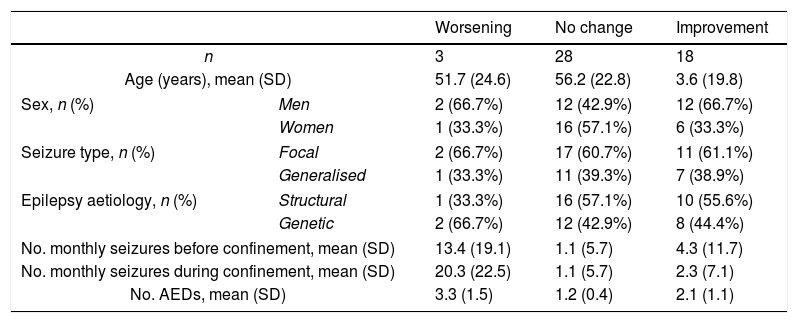
Mean epilepsy duration in our sample was 20.7 months (range, 7-64). Seizure frequency was significantly lower during confinement than in the previous 7 months (P=.004; t test). Patients were classified into 3 groups according to whether their condition had worsened, improved, or remained stable (in terms of the number of seizures per month). The chi-square test for each dichotomous variable found no significant differences associated with sex (P=.25), seizure type (P=.98), or aetiology of epilepsy (P=.73). Improvement during confinement was more frequent among patients receiving 1-2 antiepileptic drugs than among those taking more than 2 drugs (P<.003) (Table 1).
Epidemiological characteristics and seizure frequency in our sample before and during COVID-19 confinement.
| Worsening | No change | Improvement | ||
|---|---|---|---|---|
| n | 3 | 28 | 18 | |
| Age (years), mean (SD) | 51.7 (24.6) | 56.2 (22.8) | 3.6 (19.8) | |
| Sex, n (%) | Men | 2 (66.7%) | 12 (42.9%) | 12 (66.7%) |
| Women | 1 (33.3%) | 16 (57.1%) | 6 (33.3%) | |
| Seizure type, n (%) | Focal | 2 (66.7%) | 17 (60.7%) | 11 (61.1%) |
| Generalised | 1 (33.3%) | 11 (39.3%) | 7 (38.9%) | |
| Epilepsy aetiology, n (%) | Structural | 1 (33.3%) | 16 (57.1%) | 10 (55.6%) |
| Genetic | 2 (66.7%) | 12 (42.9%) | 8 (44.4%) | |
| No. monthly seizures before confinement, mean (SD) | 13.4 (19.1) | 1.1 (5.7) | 4.3 (11.7) | |
| No. monthly seizures during confinement, mean (SD) | 20.3 (22.5) | 1.1 (5.7) | 2.3 (7.1) | |
| No. AEDs, mean (SD) | 3.3 (1.5) | 1.2 (0.4) | 2.1 (1.1) | |
AED: antiepileptic drug; SD: standard deviation.
Unlike Shung-Lun et al.,1 we were able to contact nearly all patients (only one could not be reached), which may explain why none of our patients discontinued treatment. This may also have been favoured by the use of electronic prescribing, which allows patients to collect their medications directly from the pharmacy.
As in the study by Shung-Lun et al.,1 our patients presented fewer seizures during confinement. This finding should be interpreted with caution, given that our study gathered data from patients who had been in confinement for a maximum of one month.
Another limitation of our study is the lack of test data; telephone consultations are useful in the short and medium term, but insufficient in the long term. In conclusion, telephone consultations provide a useful tool for the management of patients with epilepsy in the context of confinement due to COVID-19, since they allow physicians to follow up all patients, which in turn prevents treatment discontinuation. If confinement is not extended, epileptic patients may present a decrease in seizure frequency during this period.
Please cite this article as: Hernando-Requejo V, Huertas-González N, Lapeña-Motilva J, Ogando-Durán G. Consulta de epilepsia durante la pandemia de COVID-19: papel de la telemedicina y efectos del confinamiento en pacientes epilépticos. Neurología. 2020;35:274–276.