Electroencephalography (EEG) is an essential diagnostic tool in epilepsy. Its use in emergency departments (ED) is usually restricted to the diagnosis and management of non-convulsive status epilepticus (NCSE). However, EDs may also benefit from EEG in the context of other situations in epilepsy.
MethodsWe conducted a retrospective observational study using the clinical histories of patients treated at our hospital's ED for epileptic seizures and suspicion of NCSE and undergoing EEG studies in 2015 and 2016. We collected a series of demographic and clinical variables.
ResultsOur sample included 87 patients (mean age of 44 years). Epileptic seizures constituted the most common reason for consultation: 59.8% due to the first episode of epileptic seizures (FES), 27.6% due to recurrence, and 12.6% due to suspected NCSE. Interictal epileptiform discharges (IED) were observed in 38.4% of patients reporting FES and in 33.3% of those with a known diagnosis of epilepsy. NCSE was confirmed by EEG in 36.4% of all cases of suspected NCSE. Presence of IED led to administration of or changes in long-term treatment in 59.8% of the patients.
ConclusionsEEG is a useful tool for seizure management in EDs, not only for severe, sudden-onset clinical situations such as NCSE but also for diagnosis in cases of non-affiliated epilepsy and in patients experiencing the first episode of epilepsy.
El electroencefalograma (EEG) es una prueba diagnóstica esencial en epilepsia. Su uso en los Servicios de Urgencias (SU) es limitado, estando habitualmente restringido al diagnóstico y el manejo del estado epiléptico no convulsivo (EENC). Sin embargo, pueden existir otras situaciones en las que, por su perfil temporal, el EEG puede ser una herramienta útil en este entorno.
MétodosEstudio observacional retrospectivo, sobre la base de la historia clínica, de los pacientes atendidos en el SU de nuestro hospital por crisis epilépticas (CE) y sospecha de EENC a los que se realizó un EEG, en el periodo 2015-2016, recogiendo variables demográficas y clínicas.
ResultadosSe reclutó a 87 pacientes, con una edad media de 44 años. El motivo de consulta más frecuente fue CE, el 59,8% por primera CE (pCE) y el 27,6% por CE en paciente con epilepsia; en 12,6% la sospecha era EENC. Se observaron descargas epileptiformes interictales (DEI) en el 38,4% de los pacientes atendidos por pCE y en el 33,3% de los epilépticos conocidos; el 36,4% de los posibles EENC se confirmaron mediante EEG. El EEG con DEI supuso un inicio o cambio de tratamiento crónico en el 59,8% de los pacientes.
ConclusionesEl EEG es una herramienta útil en el manejo de las CE en los SU, tanto de situaciones agudas graves como el EENC, como en el estudio diagnóstico de la epilepsia de debut o no filiada.
Epileptic seizures account for 1% of all visits to emergency departments.1 Management requires thorough medical history taking, a physical examination, and a neurological examination. Complementary tests, including laboratory analyses, electrocardiography, and head CT, are frequently performed to rule out potentially life-threatening acute conditions.2
Electroencephalography (EEG) is an essential tool in the study of epilepsy.3 In view of the advances at all levels of healthcare and the increased demand for specialised care, the use of EEG in patients with seizures attended at emergency departments is not only necessary, but also inevitable. However, some authors have warned about the progressive abuse of emergency EEG,4 given that the technique is indicated mainly for non-convulsive status epilepticus (NCSE) but has also been acknowledged to be useful for the study of such other conditions as coma of unknown origin or non-epileptic paroxysmal events.5–8 EEG should therefore be used reasonably; indiscriminate use may have a negative impact on the routine functioning of EEG laboratories, with EEG often providing no essential information for the management of patients arriving at the emergency department.
Furthermore, according to some studies, EEG is most useful when performed within 48hour after a seizure,9–13 since interictal epileptiform discharges (IED) are more frequent in the first hours/days following a seizure.14,15 This may be particularly relevant in the management of a first unprovoked episode of epileptic seizures, or seizures in patients with no previous EEG diagnosis of epilepsy, with EEG studies providing early, precise diagnostic data and enabling early, safe treatment.
We conducted a descriptive study to analyse the use of EEG at our hospital's emergency department and evaluate the usefulness of the technique in different clinical scenarios in this setting.
Patients and methodsWe reviewed the medical histories of all patients aged 14 years and older attended between 2015 and 2016 at the emergency department of Hospital Clínico Universitario Lozano Blesa (Zaragoza, Spain) who underwent EEG due to epileptic seizures or suspected NCSE and were evaluated by the on-call neurologist. EEG was indicated by the neurologist evaluating each case; all EEG studies were performed within 24hours of symptom onset. Our hospital's neurophysiology department performs emergency EEG studies between 08:00 and 15:00 from Monday to Friday. Therefore, the patients included in the study were attended and evaluated by the neurology department between 09:00 on Sunday and 15:00 on Friday and underwent EEG within a 24-hour window. EEG was performed with a Nihon Kohden Neurofax EEG-1200 system. Electrodes were placed according to the international 10-20 EEG system; the EEG study lasted 30 minutes, with the patient at rest and performing activation procedures (eye opening, eye closing, photic stimulation, hyperventilation) wherever possible. We gathered demographic data and the following clinical variables: history of epilepsy or other predisposing factors, previous use of antiepileptic drugs (AED), reason for visiting the emergency department, neurological examination findings, head CT findings, EEG findings (normal, generalised IEDs, focal IEDs, generalised slowing, focal slowing, findings compatible with NCSE), AED treatment started at the emergency department, destination at discharge, and diagnosis at discharge. In patients with history of epilepsy who underwent EEG due to seizures, we also gathered data on the reason for indicating the EEG study (when available).
We performed a univariate analysis using the SPSS statistics software (version 22).
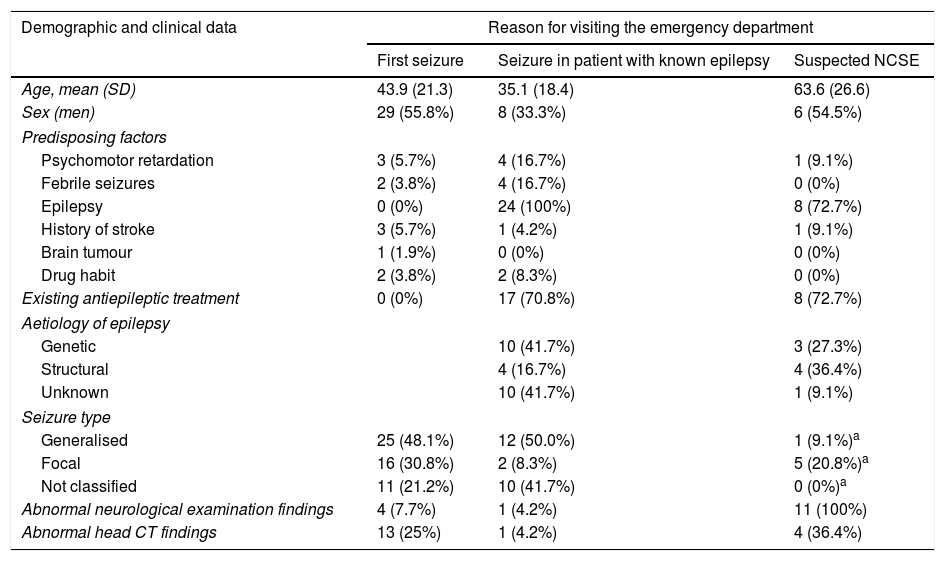
ResultsWe gathered data from 87 patients with a mean age of 44 years (range, 14-92); 44 (50.6%) were women. Fifty-two (59.8%) were attended due to a first seizure, 24 (27.6%) were patients with known epilepsy who presented seizures, and 11 (12.6%) had suspected NCSE. Table 1 summarises data on demographic variables, history of epilepsy and other predisposing factors, seizure type, and abnormal results in the neurological examination and emergency neuroimaging study in our sample.
Patients’ demographic and clinical characteristics.
| Demographic and clinical data | Reason for visiting the emergency department | ||
|---|---|---|---|
| First seizure | Seizure in patient with known epilepsy | Suspected NCSE | |
| Age, mean (SD) | 43.9 (21.3) | 35.1 (18.4) | 63.6 (26.6) |
| Sex (men) | 29 (55.8%) | 8 (33.3%) | 6 (54.5%) |
| Predisposing factors | |||
| Psychomotor retardation | 3 (5.7%) | 4 (16.7%) | 1 (9.1%) |
| Febrile seizures | 2 (3.8%) | 4 (16.7%) | 0 (0%) |
| Epilepsy | 0 (0%) | 24 (100%) | 8 (72.7%) |
| History of stroke | 3 (5.7%) | 1 (4.2%) | 1 (9.1%) |
| Brain tumour | 1 (1.9%) | 0 (0%) | 0 (0%) |
| Drug habit | 2 (3.8%) | 2 (8.3%) | 0 (0%) |
| Existing antiepileptic treatment | 0 (0%) | 17 (70.8%) | 8 (72.7%) |
| Aetiology of epilepsy | |||
| Genetic | 10 (41.7%) | 3 (27.3%) | |
| Structural | 4 (16.7%) | 4 (36.4%) | |
| Unknown | 10 (41.7%) | 1 (9.1%) | |
| Seizure type | |||
| Generalised | 25 (48.1%) | 12 (50.0%) | 1 (9.1%)a |
| Focal | 16 (30.8%) | 2 (8.3%) | 5 (20.8%)a |
| Not classified | 11 (21.2%) | 10 (41.7%) | 0 (0%)a |
| Abnormal neurological examination findings | 4 (7.7%) | 1 (4.2%) | 11 (100%) |
| Abnormal head CT findings | 13 (25%) | 1 (4.2%) | 4 (36.4%) |
CT: computed tomography; NCSE: non-convulsive status epilepticus; SD: standard deviation.
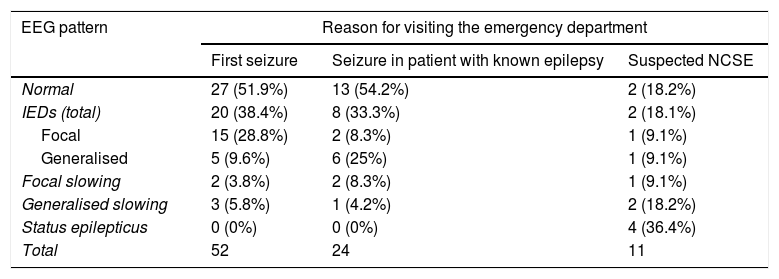
EEG results were abnormal in 45 patients (51.7%): 30 patients (34.5%) showed IEDs, 11 (12.6%) presented slowing, and 4 (4.6%) showed EEG patterns compatible with NCSE (Table 2). Fifty-nine patients (67.8%) received AEDs, 52 (59.8%) for long-term treatment (starting AED treatment or changing their usual treatment) and the rest for acute treatment of NCSE or seizures. Levetiracetam was the most frequently used AED (45 patients, 51.7%).
EEG patterns detected, according to reason for visiting the emergency department.
| EEG pattern | Reason for visiting the emergency department | ||
|---|---|---|---|
| First seizure | Seizure in patient with known epilepsy | Suspected NCSE | |
| Normal | 27 (51.9%) | 13 (54.2%) | 2 (18.2%) |
| IEDs (total) | 20 (38.4%) | 8 (33.3%) | 2 (18.1%) |
| Focal | 15 (28.8%) | 2 (8.3%) | 1 (9.1%) |
| Generalised | 5 (9.6%) | 6 (25%) | 1 (9.1%) |
| Focal slowing | 2 (3.8%) | 2 (8.3%) | 1 (9.1%) |
| Generalised slowing | 3 (5.8%) | 1 (4.2%) | 2 (18.2%) |
| Status epilepticus | 0 (0%) | 0 (0%) | 4 (36.4%) |
| Total | 52 | 24 | 11 |
EEG: electroencephalography; IED: interictal epileptiform discharge; NCSE: non-convulsive status epilepticus.
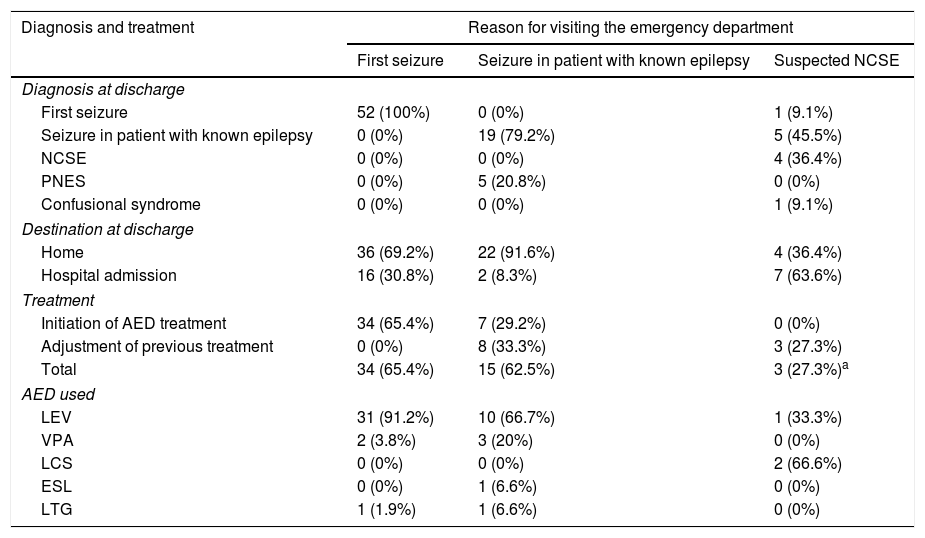
Fifteen of the 52 patients with a first seizure (28.8%) reported symptoms suggestive of epilepsy before the episode. EEG results were abnormal in 25 of these patients (48.1%), with 20 (38.4%) presenting IEDs (Table 2). Thirty-four (65.4%) were prescribed AEDs at discharge; this figure includes the 20 patients displaying epileptiform activity on the EEG and the patients presenting previous episodes of possible epileptic origin. Seventeen of the 18 patients who did not start treatment with AEDs at discharge showed normal EEG results, and the remaining patient displayed focal slowing. Table 3 lists the AEDs indicated and the destination at discharge.
Diagnosis and treatment, according to reason for visiting the emergency department.
| Diagnosis and treatment | Reason for visiting the emergency department | ||
|---|---|---|---|
| First seizure | Seizure in patient with known epilepsy | Suspected NCSE | |
| Diagnosis at discharge | |||
| First seizure | 52 (100%) | 0 (0%) | 1 (9.1%) |
| Seizure in patient with known epilepsy | 0 (0%) | 19 (79.2%) | 5 (45.5%) |
| NCSE | 0 (0%) | 0 (0%) | 4 (36.4%) |
| PNES | 0 (0%) | 5 (20.8%) | 0 (0%) |
| Confusional syndrome | 0 (0%) | 0 (0%) | 1 (9.1%) |
| Destination at discharge | |||
| Home | 36 (69.2%) | 22 (91.6%) | 4 (36.4%) |
| Hospital admission | 16 (30.8%) | 2 (8.3%) | 7 (63.6%) |
| Treatment | |||
| Initiation of AED treatment | 34 (65.4%) | 7 (29.2%) | 0 (0%) |
| Adjustment of previous treatment | 0 (0%) | 8 (33.3%) | 3 (27.3%) |
| Total | 34 (65.4%) | 15 (62.5%) | 3 (27.3%)a |
| AED used | |||
| LEV | 31 (91.2%) | 10 (66.7%) | 1 (33.3%) |
| VPA | 2 (3.8%) | 3 (20%) | 0 (0%) |
| LCS | 0 (0%) | 0 (0%) | 2 (66.6%) |
| ESL | 0 (0%) | 1 (6.6%) | 0 (0%) |
| LTG | 1 (1.9%) | 1 (6.6%) | 0 (0%) |
AED: antiepileptic drug; ESL: eslicarbazepine acetate; LCS: lacosamide; LEV: levetiracetam; LTG: lamotrigine; NCSE: non-convulsive status epilepticus; PNES: psychogenic non-epileptic seizures; VPA: valproic acid.
Of the 24 patients with history of epilepsy, 11 (45.8%) displayed abnormal EEG patterns and 8 (33.3%) presented IEDs (Table 2). The reasons for requesting an EEG were as follows: normal findings in previous ambulatory EEG studies in 8 patients (33.3%; 4 of these patients presented IEDs), lack of data on history of epilepsy in 3 (12.5%; 2 presented IEDs), suspicion of psychogenic non-epileptic seizures (PNES) in 5 (20.8%), and not specified in 8 (33.3%). Table 3 provides data on the treatment administered (initiation, change, or addition of AEDs).
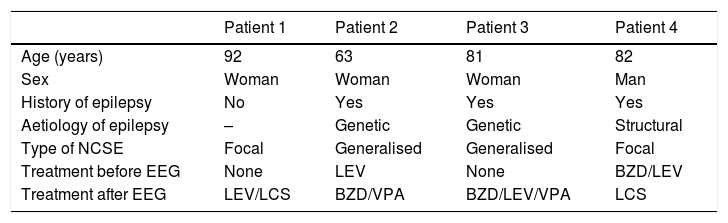
NCSE was suspected in 11 patients, 9 (81.8%) of whom presented abnormal EEG results; 4 (36.4%) displayed EEG traces compatible with status epilepticus. Ten patients started treatment with AEDs (90.9%: all patients but one, who was diagnosed with confusional syndrome). Of these, 3 were admitted to hospital (2 with a diagnosis of epileptic seizures in the context of known epilepsy and the other with a first seizure); 3 were diagnosed with seizures in the context of known epilepsy and discharged after observation in the emergency department and adjustment of their treatment (Table 3); and the remaining 4 patients were diagnosed with NCSE (2 started treatment with AEDs before the EEG was performed due to strong clinical suspicion, and the remaining 2 received AEDs after diagnosis was confirmed by EEG; Table 4).
Clinical data, EEG patterns, and treatment of patients with non-convulsive status epilepticus.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Age (years) | 92 | 63 | 81 | 82 |
| Sex | Woman | Woman | Woman | Man |
| History of epilepsy | No | Yes | Yes | Yes |
| Aetiology of epilepsy | – | Genetic | Genetic | Structural |
| Type of NCSE | Focal | Generalised | Generalised | Focal |
| Treatment before EEG | None | LEV | None | BZD/LEV |
| Treatment after EEG | LEV/LCS | BZD/VPA | BZD/LEV/VPA | LCS |
BZD: benzodiazepine; EEG: electroencephalography; LCS: lacosamide; LEV: levetiracetam; NCSE: non-convulsive status epilepticus; VPA: valproic acid.
Indication of emergency/early EEG is controversial due to the difficulty of finding a balance between the utility of EEG and the potential overload of EEG laboratories. However, early EEG may be more useful than ambulatory EEG for certain indications, which we will address in the following sections.
First seizureIn our study, first seizures were the main reason for early EEG in patients attending the emergency department. The classical diagnostic definition of epilepsy as a condition presenting with 2 unprovoked seizures occurring over 24hours apart was subsequently expanded with the 2014 ILAE definition, allowing diagnosis of epilepsy after a first seizure in patients with a recurrence risk > 60%.16 Early diagnosis of a first seizure is therefore particularly relevant. A meta-analysis conducted by the American Academy of Neurology on the management of first seizures in adults analysed one Class I article and 10 Class II articles on the diagnostic yield of EEG, finding that significant abnormalities (IEDs) were detected in 29% of patients.17 However, Pohlmann-Eden and Newton18 differentiate between the diagnostic yield of conventional EEG and that of sleep EEG, with the former achieving lower detection rates (12%-27% vs 23%-50%). Other studies have found an association between short-term conventional EEG (24-48hour) and higher rates of IED detection.9–13 In a prospective study of 300 patients with a first seizure, King et al.9 found a significantly higher percentage of IEDs in EEG studies performed within 24hours of the seizure than in EEG studies performed later (51% vs 34%). In our study, EEG detected IEDs in 38.4% of patients with a first seizure; this percentage is higher than that reported in the meta-analysis from the American Academy of Neurology,17 in which no distinction was made according to the time interval between the seizure and the EEG study, and even higher than the 12%-27% diagnostic yield established by Pohlmann-Eden and Newton18 for conventional EEG (ours is more similar to the rate reported after excluding patients undergoing sleep EEG). The fact that our rate is lower than that reported by King et al.9 may be explained by differences in age ranges: King et al. included paediatric patients, who displayed IEDs more frequently than adults (59% vs 39%). Likewise, other authors have reported different percentages of patients showing significant abnormalities on early EEG studies, including Sierra-Marcos et al.10 (41%), Paliwal et al.11 (48.6%), Schreiner and Pohlmann-Eden12 (26.8%), and Yigit et al.13 (43.3%). Other studies, however, suggest that performance of EEG studies after a first seizure should be evaluated and coordinated by specific units on an outpatient basis,19,20 depending on each centre's characteristics. In our opinion, early EEG requested by a neurologist after a thorough examination is beneficial since it is more sensitive to IEDs.
Another relevant finding is that 28.8% of patients reported symptoms suggestive of epilepsy prior to the first seizure. These events can go unnoticed and are often compatible with absence seizures, myoclonus, or epileptic aura.9 Regardless of EEG findings, all patients in our series started treatment with AEDs due to the high risk of recurrence, since the event motivating the consultation may be classified as an “apparent” first seizure. This underscores the importance of gathering a complete medical history, even in such situations as those seen at emergency departments.
Non-convulsive status epilepticusSuspicion of NCSE is the most widely accepted indication for an emergency EEG. A survey of the directors of several accredited EEG laboratories revealed little consensus on the clinical symptoms found to be most appropriate for indicating an emergency EEG, with the exception of suspected NCSE.21 In our study, NCSE was initially suspected in 12.6% of patients; suspicion was confirmed by EEG in 36.4% of this group. In a study analysing EEG patterns in elderly patients hospitalised due to delirium, 28% of EEG patterns recorded within 24hours of arrival at the emergency department were compatible with NCSE.22 In another prospective study into the incidence of NCSE, the diagnosis was not suspected by the treating physician in nearly half of patients.23 This suggests that NCSE is probably underdiagnosed; protocols should be developed for detecting the condition among patients with suspected NCSE. In fact, history of epileptic seizures is the only finding consistently reported to be a risk factor for NCSE in patients with suspected NCSE,24–26 which makes selecting cases a challenge. This explains why EEG continues to be essential for the diagnosis and treatment of NCSE and underscores the need to develop protocols for EEG use and to train healthcare professionals to interpret EEG recordings. The development of simpler EEG systems may be useful in this clinical setting27 and help to achieve these goals.
Epileptic seizures in patients with known epilepsyThe value of EEG in chronic management of epilepsy is limited (a patient with epilepsy does not need to undergo an EEG in the event of a seizure), although it may provide valuable data in certain situations, such as changes in semiology or a marked increase in seizure frequency.28 Early EEG (< 24hours after a seizure) may be of diagnostic value in a very limited number of cases. Therefore, the increased likelihood of detecting IEDs within 24hours of the episode offers the opportunity to establish a diagnosis with a higher level of certainty. In our sample, 24 patients (27.6%) had a prior diagnosis of epilepsy; seizure type was not clearly defined in 8 of these (33.3%) due to inconclusive medical history data and a lack of abnormal results in previous EEG studies; no data on history of epilepsy were available for another 3 patients (12.5%). Early EEG results were abnormal in 4 patients (50%) in the first subgroup and 2 (66.7%) in the second. Of these 6 patients, AED treatment was modified in 4 cases based on EEG results (one patient was started on a new AED and treatment was adjusted for the remaining 3 since they displayed generalised IEDs and were receiving inappropriate AEDs). Therefore, EEG influenced treatment decision-making and contributed new clinical data in one-third of patients for whom early EEG was correctly indicated. Although early EEG in the emergency department is usually not indicated for this population, it may be useful in some cases, mainly in patients with epilepsy displaying normal results in previous EEG studies and receiving long-term AED treatment. Requests for early EEG must be managed by the neurophysiology laboratory, particularly when the technique is not necessary for emergency management. In fact, early EEG was not justified for this indication in 33.3% of these patients, which highlights the importance of avoiding abuse of the technique.
Psychogenic non-epileptic seizuresFive patients in our series were discharged with a diagnosis of PNES; all had previously been diagnosed with epilepsy. All 5 displayed normal interictal EEG results. One patient underwent EEG during the episode, but the reading revealed no epileptiform activity. The gold standard for diagnosing PNES is clinical suspicion combined with normal ictal video-EEG results. Although normal interictal EEG results do not rule out the possibility of epileptic seizures, they are a defining feature of probable and possible PNES.29 Early EEG is of limited diagnostic value in emergency departments due to the complexity of these cases; although the technique may provide additional data, in most cases it is neither beneficial nor necessary for the management of these patients.
Early EEG and treatment after a first seizureTreatment with AEDs after a first seizure is much debated. According to a recent meta-analysis, IEDs constitute a risk factor for recurrence after a first seizure, together with potentially epileptogenic neuroimaging alterations and nocturnal seizures. Furthermore, treatment with AEDs after a first seizure reduces the risk of seizure recurrence within 2 years, but does not change long-term prognosis.30 The decision to treat is complex and must be based on the analysis of risk factors for recurrent seizures, the patient's occupation and need to drive, patient preferences, and the adverse effects of AEDs.31 The decision must therefore be made case by case and agreed with the patient. A recent prospective study including a large patient sample suggests that longer seizure freedom after a first seizure may predict a lower risk of recurrence32 in the long term, which may justify early, comprehensive assessment of these patients with a view to starting treatment early. A survey of a group of Spanish experts, enquiring about treatment initiation after a first seizure, revealed consensus on beginning antiepileptic treatment in patients showing IEDs in the EEG study, those with structural MRI alterations, and elderly patients.33 In our study, 100% of patients with a first seizure and displaying IEDs received AED treatment, vs. 37% of patients with normal EEG results and 80% of those with non-epileptiform EEG alterations; this is consistent with the consensus recommendations mentioned above. The most frequently prescribed AEDs were levetiracetam and valproic acid, which is also consistent with the consensus recommendations; these 2 AEDs are recommended in an ILAE meta-analysis as initial monotherapy for adults with focal seizures (levetiracetam, level A evidence) or generalised tonic-clonic seizures (valproic acid, level C evidence).34 Early EEG may therefore be useful not only for diagnosis but also for treatment decision-making at the emergency department.
Our study has several limitations, including its retrospective design and the small sample size. However, our results support the hypothesis that EEG is a useful tool for the diagnosis and treatment of epilepsy at the emergency department. It constitutes an essential tool for the management of NCSE and is probably beneficial for evaluating unprovoked first seizures, since it allows rapid treatment decision-making. Although EEG use is becoming increasingly frequent, efforts should be made to make the technique available for hospital emergency departments, and indication and action protocols should be implemented to ensure that the tool is used rationally and efficiently.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Viloria Alebesque A, López Bravo A, Bellosta Diago E, Santos Lasaosa S, Mauri Llerda JA. Utilidad del electroencefalograma en el manejo de la epilepsia en el Servicio de Urgencias. Neurología. 2020;35:238–244.