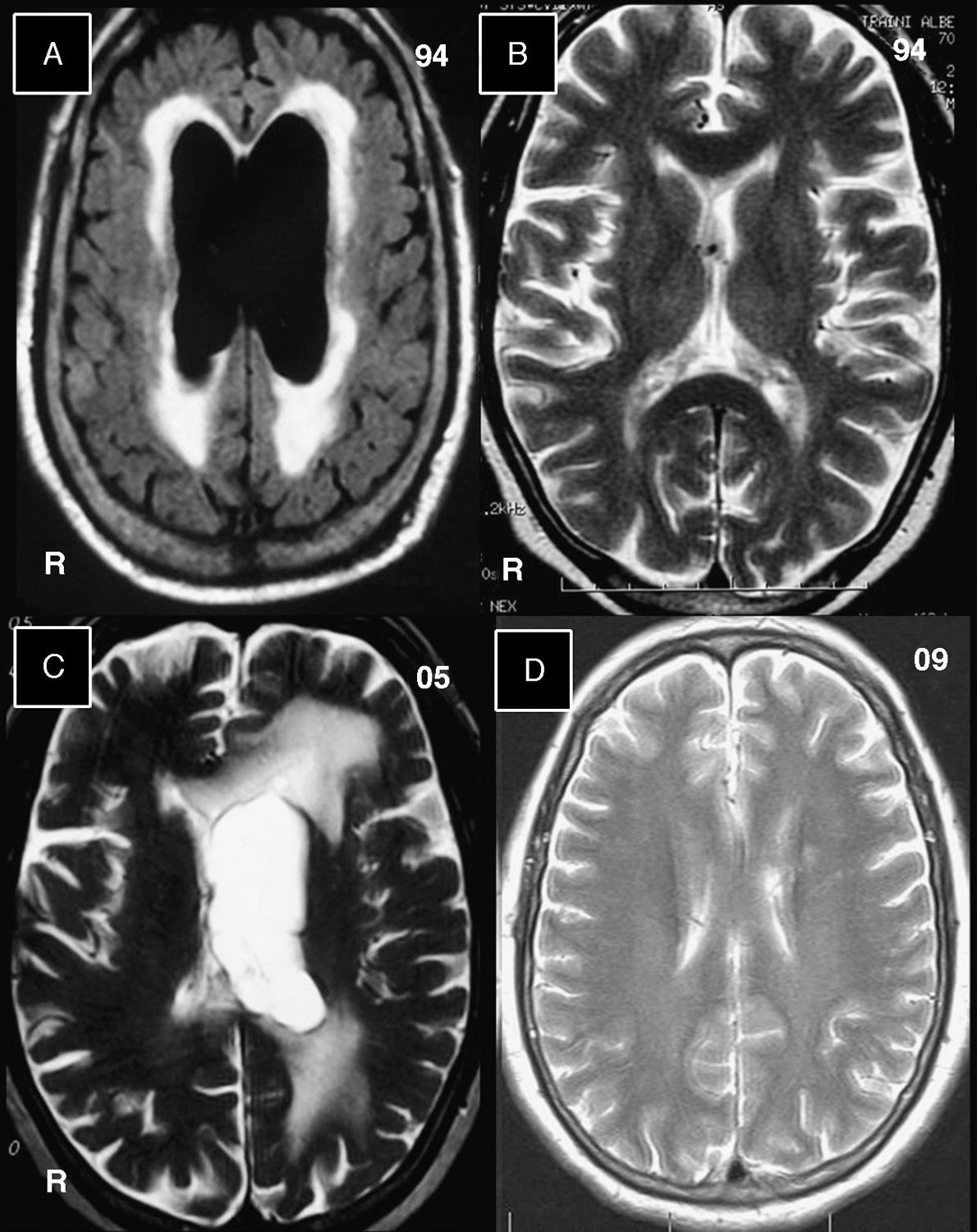
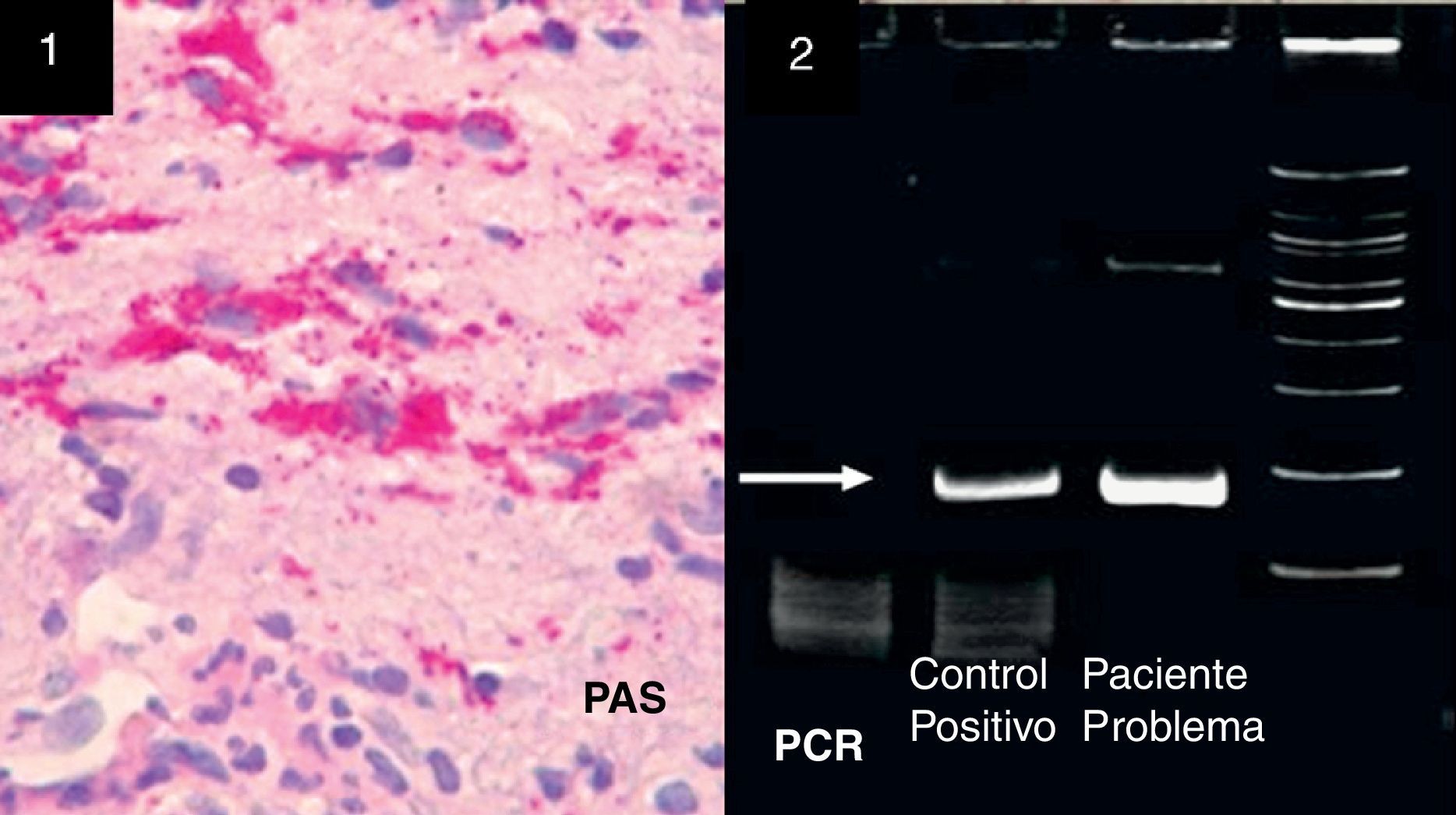
Whipple's disease (WD) is an uncommon condition caused by persistent infection with Tropheryma whipplei (TW). Clinical manifestations vary greatly, and may include digestive, articular, ocular, cardiac, renal, pulmonary, and nervous system symptoms. We present the hospital reports for a 78-year old male patient who had been suffering numerous recurring and remitting febrile episodes with migratory polyarthritis since the age of 33. WD was diagnosed by duodenal biopsy when the patient was 53 and had been experiencing recurring diarrhoea over several months. The patient was then treated with oral trimethoprim/sulfamethoxazole (TS) for more than 6 years. In 1994, he presented with unstable gait due to normal pressure hydrocephalus, which was treated surgically. Results from the cytochemical analysis of CSF were normal (Fig. 1, (A) hydrocephalus and periventricular oedema and (B) resolution of hydrocephalus following ventriculo-atrial shunting). Patient was treated with TS for an additional 6 years. He remained asymptomatic until the age of 70, when he suffered 3 episodes of transient dysarthria in 6 months. At the age of 72, he developed an acute confusional state. Brain MRI revealed hyperintensities in the left hemisphere and asymmetrical ventricular dilation (Fig. 1C). CSF analysis showed normal cell counts and glucose and a very high protein level (2.5g/L); both specific and non-specific cultures were negative. He underwent placement of a second cerebral shunt and during the procedure, doctors performed a biopsy on the periventricular region and intraventricular adhesions; PCR testing of the sample revealed PAS+ macrophages (Fig. 2, 1) and TW (Fig. 2, 2). Doctors also examined the sample with an electron microscope and found macrophage inclusions with trilaminar membranes and resembling bacilli.
Brain MR images without gadolinium contrast enhancement. (A) In this FLAIR image from 1994, we see bilateral ventricular dilation with hyperintensities around ventricular cavities. (B) T2-weighted image taken 1 month after (A) and after placement of the ventriculo-atrial shunt. The ventricular cavities returned to normal. (C) T2-weighted image from 2005 showing dilation of the lateral ventricle in the left hemisphere and hyperintensities surrounding that ventricle. (D) T2-weighted image from 2009 showing normal-sized lateral ventricles and no changes to the cerebral parenchyma.
(1) Biopsy sample of brain and intraventricular adhesion tissue subjected to periodic acid Schiff test (PAS+), revealing lymphocytes and macrophages containing material consistent with TW bacteria. (2) Polymerase chain reaction (PCR) test; TW detected with 16s ribosomal RNA sequencing. These oligonucleotides can detect fragments of 160 base pairs in the presence of bacterial DNA. The white arrow indicates the intense white band in the column indicating our patient sample, compared to a positive control.
Treatment with continuous sulfamethoxazole and trimethoprim was reinstated (800mg and 160mg, respectively, twice daily) in addition to intramuscular ceftriaxone (1g twice daily) for 2 months. Symptoms disappeared and a brain MRI taken when the patient was 77 showed no lesions (Fig. 1D). The patient was asymptomatic as of his last check-up in 2010, and on treatment with equal doses of trimethoprim and sulfamethoxazole. This clinical history was presented in poster format at the 86th Annual Meeting of the American Association of Neuropathologists, held from 9 to 13 June 2010. It was also published as an abstract.1 Our current objective is to publish the case in Spanish.
Diagnosing WD may be difficult in patients who did not experience digestive symptoms from the onset. Polyarthralgias are the cardinal symptoms in half of all cases of the disease.2 In the case described here, both of those characteristics were present. Central nervous system disorders may appear as communicating hydrocephalus, vertical gaze palsy, cerebrovascular events, convulsions, confusional state, progressive cognitive impairment, and very characteristic signs such as oculomasticatory myorhythmia.3,4 The case we describe presented with 3 of the neurological manifestations listed above. In patients with WD, macrophages have an abnormally acidic pH, which permits survival of TW within the cytoplasm.5–7 Prior to the development of antibiotics (ATBs), WD was fatal. The first ATBs used in WD treatment were penicillin and tetracyclines, but recurrences were very common. In recent decades guidelines have recommended ATBs that cross the blood–brain barrier, such as TS, which has been used since the 1970s. Recent suggestions include parenteral ceftriaxone and oral TS. Additional recommendations include oral cephalosporins and doxycycline as long-term treatment and hydroxychloroquine to modify the pH in macrophages,8–10 but these recommendations are based on infrequent case studies and not on controlled trials. Treatment time with ATB for cases of WD with neurological complications has not been established, and prolonged administration may be a reasonable option. Throughout this patient's long observation period, we have found that nervous system symptom relapses tended to appear after TS treatment had been suspended or reduced, or possibly after failure of prolonged TS treatment,11 almost as if TW were waiting for lower concentrations of the bacteriostatic agent. When treating patients with WD and neurological manifestations, we suggest that the antibiotic that improves their condition should not be reduced or discontinued.
Please cite this article as: Domínguez RO, et al. Enfermedad de Whipple: Múltiples recaídas sistémicas y neurológicas. Neurología. 2013;28:57–9.