Headache is a frequent reason for consultation between primary care physicians, emergency services physicians, and neurology specialists; however, it is not always well managed. The Andalusian Society of Neurology’s Headache Study Group (SANCE) aimed to analyse headache management at different levels of care.
Material and methodsWe conducted a descriptive cross-sectional study with data gathered through a retrospective survey in July 2019. Participants completed a series of structured questionnaires on different social and work-related variables from 4 different groups of healthcare professionals (primary care [PC], emergency departments, neurology departments, headache units).
ResultsA total of 204 healthcare professionals completed the survey: 35 emergency department physicians, 113 PC physicians, 37 general neurologists, and 19 neurologists specialising in headache. Eighty-five percent of PC physicians reported prescribing preventive drugs, which were maintained for at least 6 months (59%), with flunarizine and amitriptyline being the most commonly used. Most patients attended at neurology consultations (65%) are referred by PC physicians, with changes in the headache pattern being the main reason for referral (74%). Healthcare professionals across all levels of care showed great interest in headache and in receiving training in headache management (97% of PC physicians, 100% of emergency services physicians, 100% of general neurologists).
ConclusionsMigraine sparks great interest among healthcare professionals from different levels of care. Our results also reveal a lack of resources for headache management, which is reflected in the long waiting times. Other means of bilateral communication between different levels of care should be explored (eg, e-mail).
La cefalea representa un motivo de consulta frecuente entre los médicos de atención primaria, urgencias y especialistas en Neurología, que no siempre es bien manejada. El Grupo de Cefaleas de la Sociedad Andaluza de Neurología (SANCE) se plantea conocer su manejo entre los distintos niveles asistenciales.
Material y métodosEstudio descriptivo transversal realizado mediante una encuesta retrospectiva en julio de 2019. Los participantes completaron una serie de cuestionarios estructurados recogiéndose distintas variables socio-laborales en cuatro grupos sanitarios distintos (Atención Primaria, Servicios de Urgencias, Neurología General, Unidades de Cefalea).
ResultadosSe llevaron a cabo un total de 204 entrevistas repartidas entre los distintos grupos profesionales: 35 médicos de urgencias, 113 de atención primaria, 37 neurólogos generales y 19 neurólogos especialistas en cefaleas. El 85% de los médicos de AP prescribe fármacos preventivos, que mantiene durante al menos seis meses (59%), siendo flunarizina y amitriptilina los más utilizados. La atención primaria representa la vía principal de llegada a las consultas de Neurología General (65%), siendo los cambios en el patrón de la cefalea el principal motivo de derivación (74%). Todos los niveles asistenciales incluidos en el trabajo muestran gran interés en la cefalea y en la posibilidad de asistir a cursos de formación (97% AP, 100% médicos de urgencias, 100% neurólogos generales).
ConclusionesEl presente trabajo ha observado escasez de recursos reflejado por prolongadas listas de esperas, así como gran interés en las cefaleas por parte de los participantes. Es necesario buscar otras formas de comunicación bilateral entre los distintos ámbitos asistenciales, como por ejemplo el correo electrónico.
Headache represents one of the main reasons for consultation with neurologists1,2 and is one of the leading causes of disability in daily living activities worldwide.3–5 It has a considerable social and economic impact, as it affects a population segment in the most productive period of life.1
Migraine is a primary headache disorder affecting approximately 12% of the global population.6,7 Migraine is the most prevalent neurological disease in Spain, affecting over 5 million people; according to the 2019 Global Burden of Disease Survey, it is the third most prevalent disorder worldwide, the second leading cause of disability (and the leading cause in individuals aged 15–49 years), and one of the 5 main causes of years lived with disability.8 It more frequently occurs in women, with a higher degree of disability as measured with the Migraine Disability Assessment, according to the results of the American Migraine Prevalence and Prevention study.9
Such is the magnitude of the problem that the World Health Organization has declared migraine to be the seventh disease overall, and the second neurological disease, causing the most years lived with disability, accounting for a high percentage of workplace absences and loss of productivity in Spain, with an annual cost estimated at 2 billion euros. Despite the great impact of migraine, 2 significant issues remain: underdiagnosis and undertreatment of the disease.4,5 Furthermore, a high percentage of patients with migraine overuse non-prescription analgesics.
The Spanish Action Plan Against Migraine (PALM) project, developed in 2006, sought to characterise the problem of migraine at different levels of care, demonstrate the impact of this disease, and train the professionals involved in treating patients with migraine.10–12 As we may expect, the study demonstrated the high prevalence of the disease, which was poorly treated and often underestimated, with delayed diagnosis.
To meet these challenges, headache units were introduced to offer specialised care to this patient group, enabling assessment by highly qualified healthcare professionals with access to the latest treatments to manage this widespread disorder, optimising health expenditure by improving the efficacy of diagnostic and therapeutic management and decreasing the rate of unnecessary studies, medication consumption, and emergency department visits.13
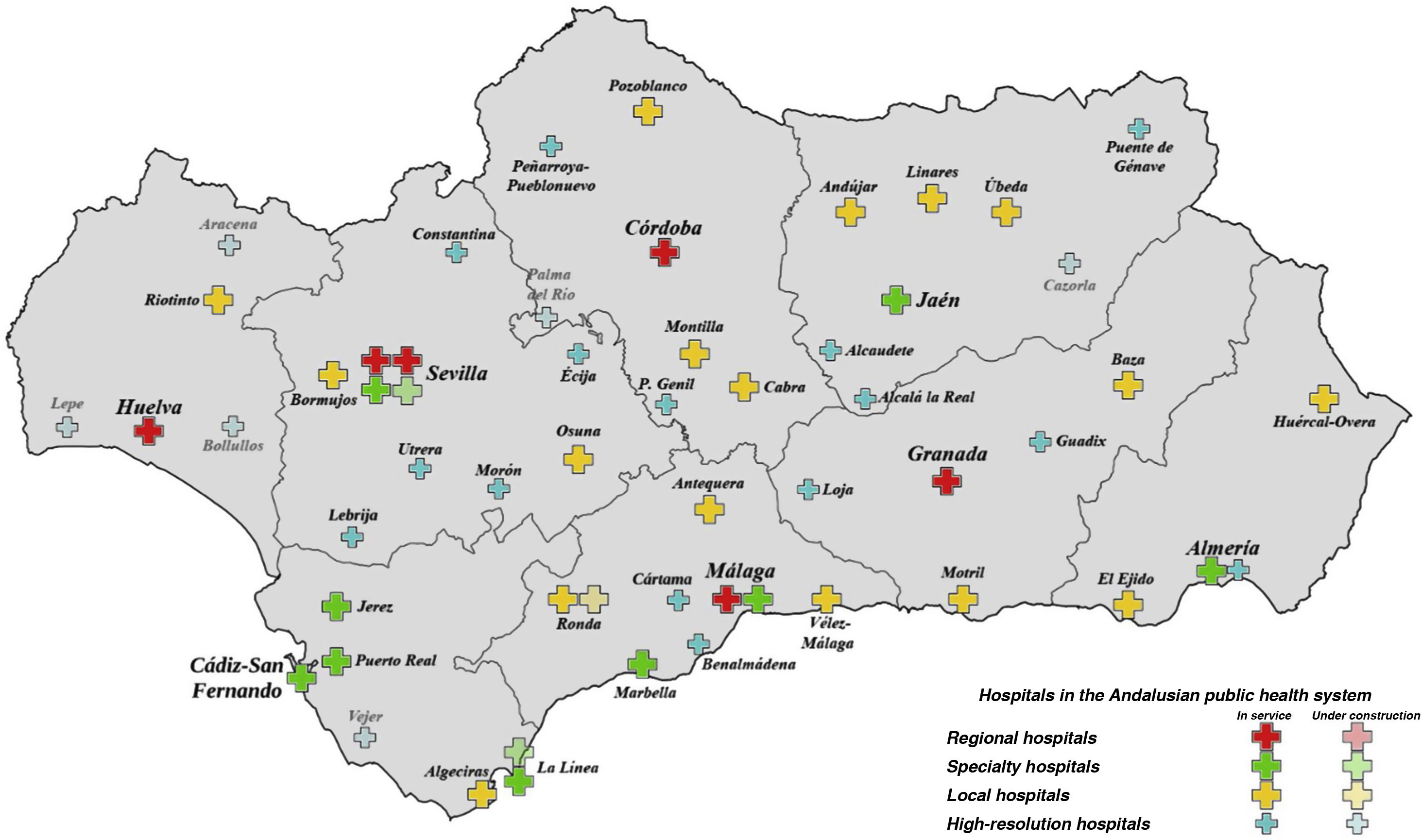
Andalusia is the most populous autonomous community in Spain, with a population of 8 476 718 (2020 data from the Spanish National Statistics Institute), and the second largest (87 268 km2), after Castile–Leon. A large part of its population lives in rural areas, with limited resources and access to large cities. At present, the Andalusian economy is disadvantaged with respect to the wider Spanish and European context, as a result of the late arrival of the industrial revolution and the significant weight of rural settings and agriculture. This lack of resources also leaves its mark on the Andalusian regional health service in general and on neurology departments in particular, with very few local hospitals having a specialist neurologist on their staff. Within the regional health system, there are 4 levels of healthcare centres: regional hospitals (serving the entire autonomous community), speciality hospitals (each serving a province), local hospitals (population within one hour’s travel), and high-resolution hospitals (population within 30 minutes’ travel). Fig. 1 shows the hospitals in each province.
Due to the high prevalence of headache disorders, and particularly migraine, and the associated disability, together with the need to create a comprehensive care plan for patients with headache, the main aim of the Headache Study Group of the Andalusian Society of Neurology (SANCE) in conducting the present study was to improve the knowledge and understanding of this disorder among healthcare professionals in the region. As primary care is the first level of care provision, we addressed this aim from a multidisciplinary perspective, including primary care physicians, emergency departments, general neurologists, and headache specialists.
Material and methodsWe conducted a cross-sectional descriptive study using a survey enquiring about past experience. Participants completed a series of structured questionnaires on an online platform, using their mobile phones, personal computers, or tablets. An e-mail was sent to all members of the Andalusian Society of Neurology (SAN) (n = 250) inviting them to participate; members replying to the e-mail eventually formed the study sample, responding to our online survey. Data are expressed as absolute and relative frequencies (n [%]).
We received a total of 35 completed surveys (10 minutes’ duration) from emergency department physicians, 133 (10 minutes’ duration) from primary care physicians, 37 (14 minutes’ duration) from neurology department specialists, and 19 (20 minutes’ duration) from neurologists at headache units (including those working in specialist clinics). The variation in survey completion time is fundamentally explained by the content of each survey: more general questions were put to professionals not working in the area of neurology, whereas surveys completed by neurologists included more specific and broader questions. Surveys are included in the supplementary material. Questions on the percentage of patients consulting with headache/migraine were ordinal and stratified.
All fieldwork was conducted between 3 and 25 July 2019.
We collected the following demographic data on survey respondents:
- a.
Sex
- b.
Age
- c.
Area of practice (primary care, emergency department, general neurology department, headache unit)
- d.
Public/private practice
- e.
Tenure hospital position
- f.
Years of professional experience, including residency period.
Below, we present detailed results from the 4 groups of respondents. Baseline characteristics included:
- -
Emergency department physicians: two-thirds (66%) of respondents were women; 34% were aged 50 years or older. Nearly all respondents worked in the public health system (97%), with 83% having worked for 10 years or longer.
- -
Primary care physicians: sixty-five percent of respondents were women; 34% were aged 50 years or older. Ninety-six percent worked in the public health system, with 56% having worked for 10 years or longer.
- -
General neurologists: fifty-one percent of respondents were women; 51% were aged 50 years or older. A total of 89% worked in the public health system, with 87% working at university hospitals.
- -
Headache unit neurologists: Nearly half (47%) of respondents were women; 37% were aged 50 years or older. A total of 95% worked in the public health system, with 84% working at university hospitals.
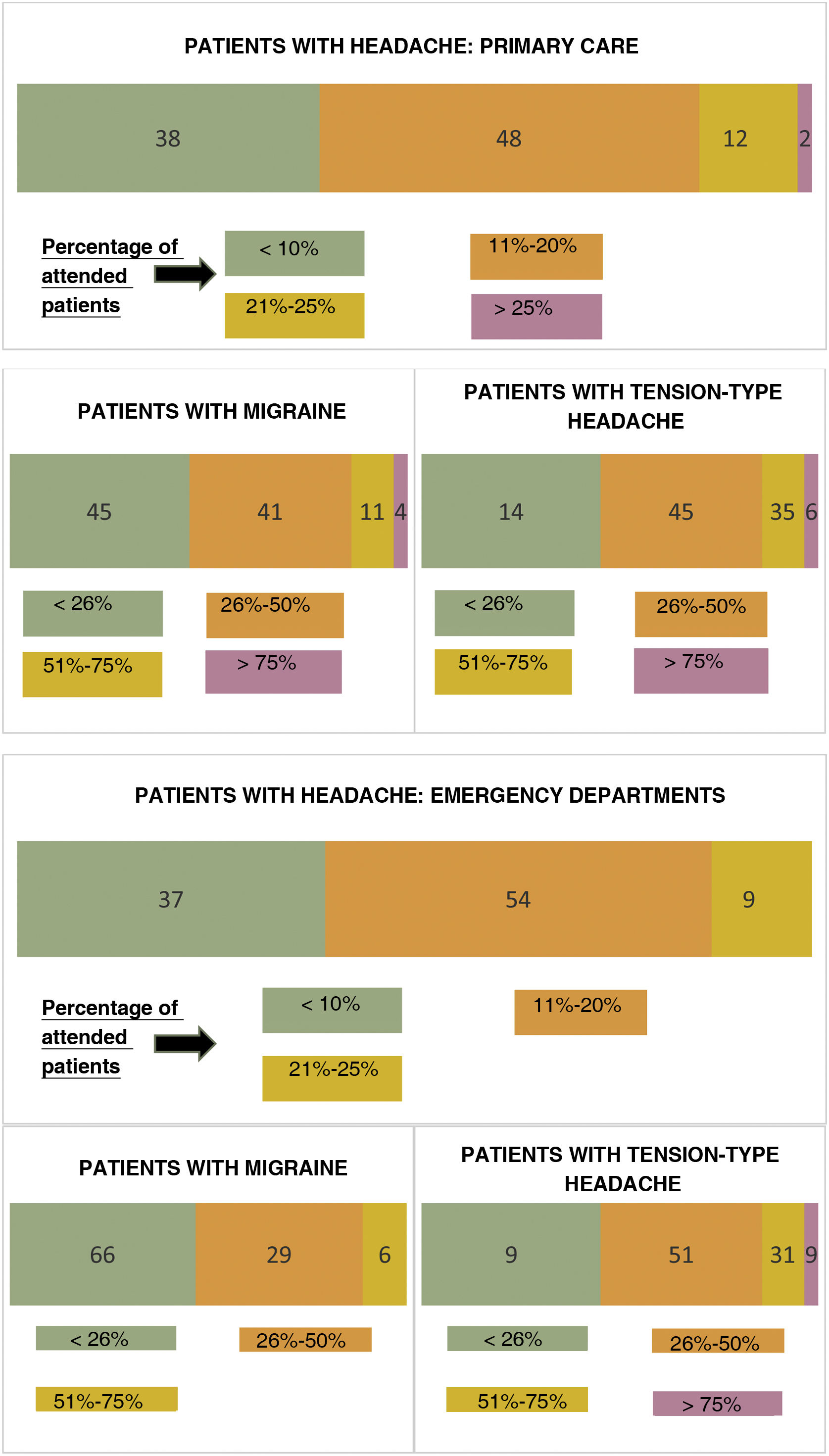
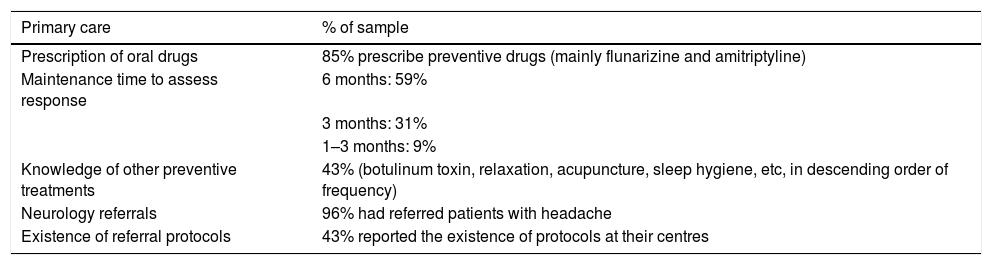
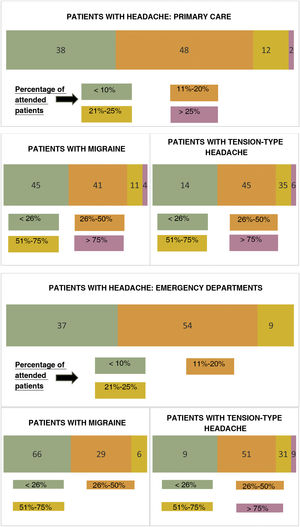
Eighty-six percent of respondents reported that 50% or less of the clinical assessments performed each month were in patients consulting due to migraine: < 26% of all patients for 45% of respondents and 26%–50% for 41% (detailed percentages are shown in Fig. 2). Eighty-five percent prescribed oral preventive drugs, which they maintained for at least 6 months to assess efficacy (59%); fewer than half of this group (43%) were familiar with and used preventive methods other than oral medication (eg, acupuncture, botulinum toxin, lifestyle/dietary measures) (Table 1).
General information from primary care physicians.
| Primary care | % of sample |
|---|---|
| Prescription of oral drugs | 85% prescribe preventive drugs (mainly flunarizine and amitriptyline) |
| Maintenance time to assess response | 6 months: 59% |
| 3 months: 31% | |
| 1–3 months: 9% | |
| Knowledge of other preventive treatments | 43% (botulinum toxin, relaxation, acupuncture, sleep hygiene, etc, in descending order of frequency) |
| Neurology referrals | 96% had referred patients with headache |
| Existence of referral protocols | 43% reported the existence of protocols at their centres |
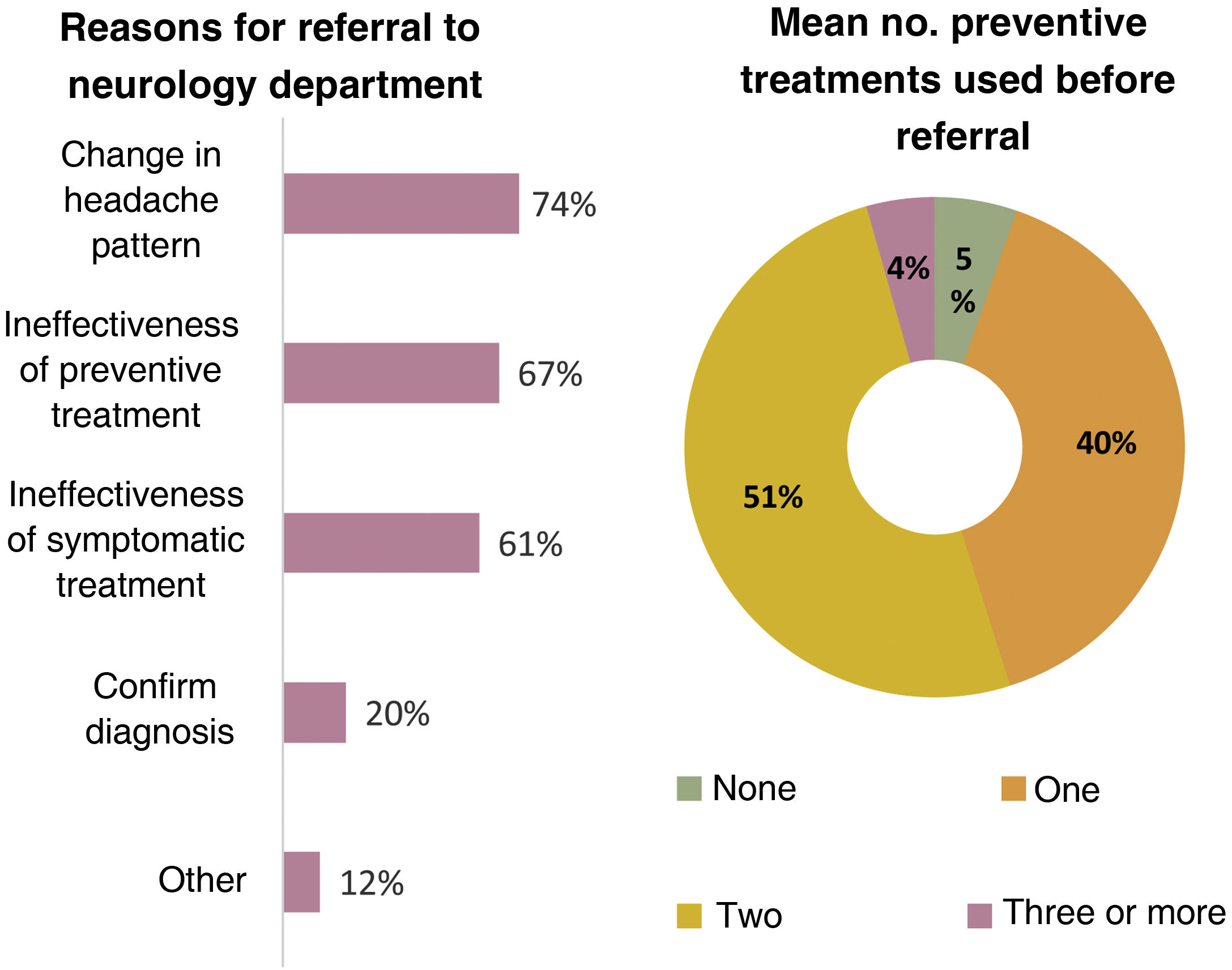
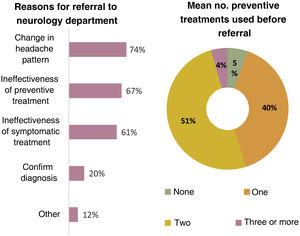
A total of 96% of primary care physicians reported that they referred patients with headache to neurology departments, with the main reason for referral being changes in the headache pattern (74%); 51% of respondents reported trying a mean of 2 drugs before referral to a specialist (Fig. 3).
Nearly all primary care physicians (99%) recommended that their patients use symptomatic treatments, included among the recommendations of the SANCE. However, 23% of respondents regularly prescribe daily symptomatic treatment, despite the great majority (95%) being aware that medication overuse can worsen headache. Despite knowing of the existence of the SANCE guidelines, fewer than half of respondents (44%) said that they would know how to manage patients according to these guidelines in order to achieve dishabituation.
Regarding other headache disorders, 96% of respondents said that they would know how to diagnose cluster headache, and 98% would know how to diagnose trigeminal neuralgia. Non-steroidal anti-inflammatory drugs (NSAID) were the main treatment option reported for cluster headache (49%), followed by neuromodulators (40%: pregabalin, gabapentin, etc.); for trigeminal neuralgia, the preferred option was neuromodulators (97%).
Finally, half of respondents reported using neuroimaging as part of the complementary study. Eighty-seven percent saw headache units as a necessary tool, with 97% being interested in attending training courses in order to better manage these patients.
Emergency department physiciansA total of 54% of respondents reported that 11%–20% of the patients they attended each month consulted due to headache, with 66% of these reporting that among these patients with headache, at least one in 4 had migraine (detailed percentages are shown in Fig. 2).
The most frequently used treatments for headache attacks in the emergency department were NSAIDs (71%) and triptans (46%). NSAIDs were also the drugs most frequently prescribed at discharge (74%), followed by triptans (63%). Opioids were rarely used by this group of respondents (9%), both for acute treatment and for symptomatic treatment at home (6%).
Furthermore, 60% of the sample prescribed preventive drugs for use at home (the most frequently reported options were topiramate, beta-blockers, amitriptyline, and flunarizine). Thirty-four percent of respondents knew of other preventive or symptomatic treatments other than oral drugs (eg, lifestyle/dietary interventions, anaesthetic nerve block, botulinum toxin).
A total of 91% reported good communication with neurology departments, with 14% always referring patients with migraine for specialist attention. General neurology departments were the main destination for patient referrals (80%), followed by referral to primary care (20%). Twenty-nine percent of respondents reported the existence of joint protocols with neurology departments for the management of migraine at the emergency department, with fewer than half (46%) reporting the existence of a headache unit at their hospital, despite the fact that a high percentage (86%) considered these a necessary tool to improve care provision.
Sixty-three percent of respondents were aware of the possibility of anaesthetic nerve block as a treatment option for migraine attacks, and 91% were interested in learning to perform the procedure.
Regarding other headache disorders, 91% of respondents knew how to diagnose cluster headache, with oxygen therapy being their preferred treatment option (81%), followed by NSAIDs (41%) and subcutaneous sumatriptan (41%). Forty-three percent also prescribed preventive treatments for home use. All respondents answered that they would know how to diagnose trigeminal neuralgia, with neuromodulators being their preferred treatment option (94%).
Finally, all respondents were interested in attending training courses on headache management.
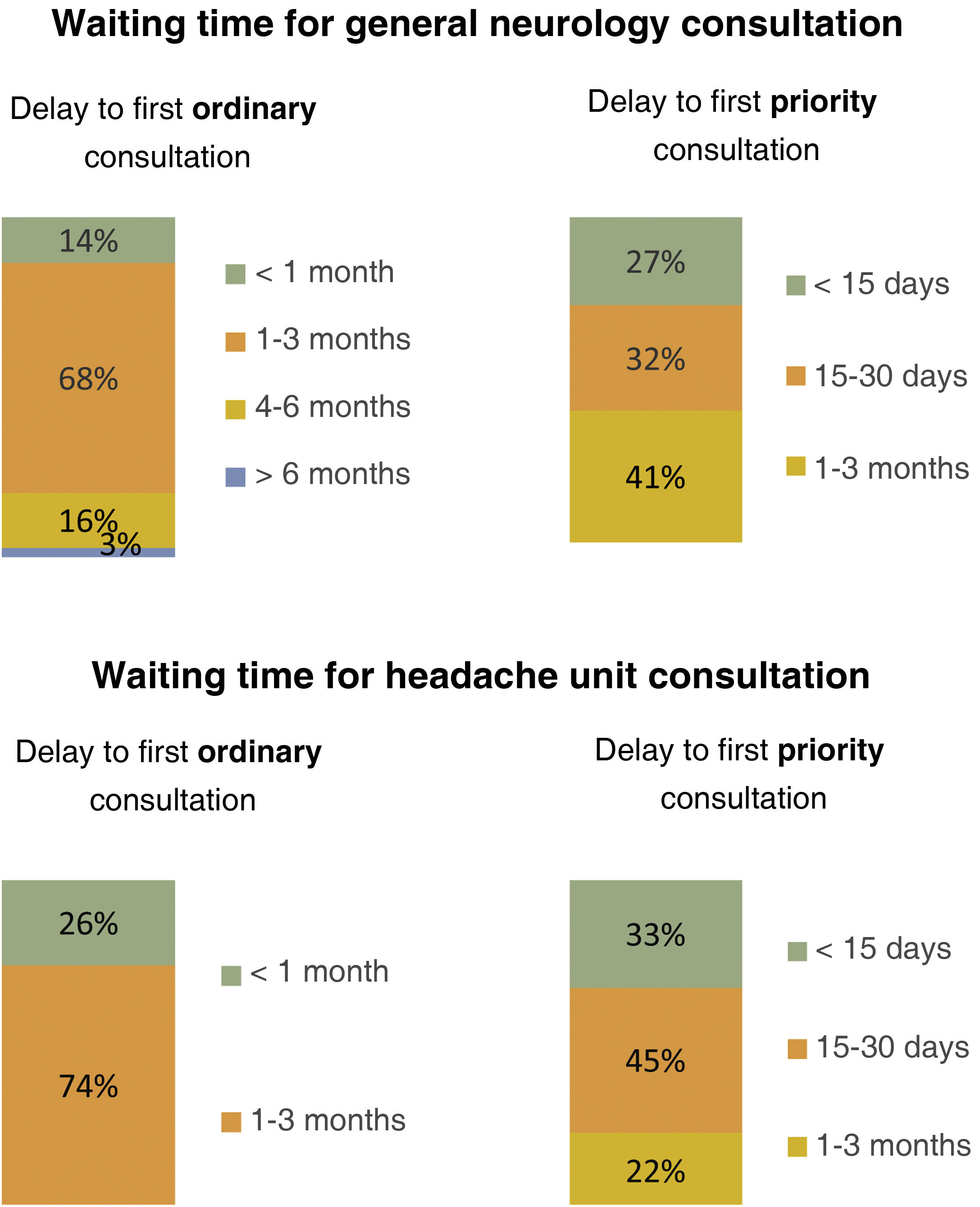
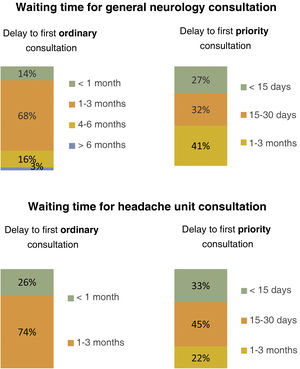
General neurologistsThe majority of general neurologists (65%) reported that most of their patients with headache were referred from primary care; the mean delay to the first ordinary assessment was 1–3 months (68%) (Fig. 4), with a mean of under 30 days for priority referrals (59%). In 54% of cases, these referrals were reviewed, with a waiting list in 49% of cases, both for ordinary and for priority assessment.
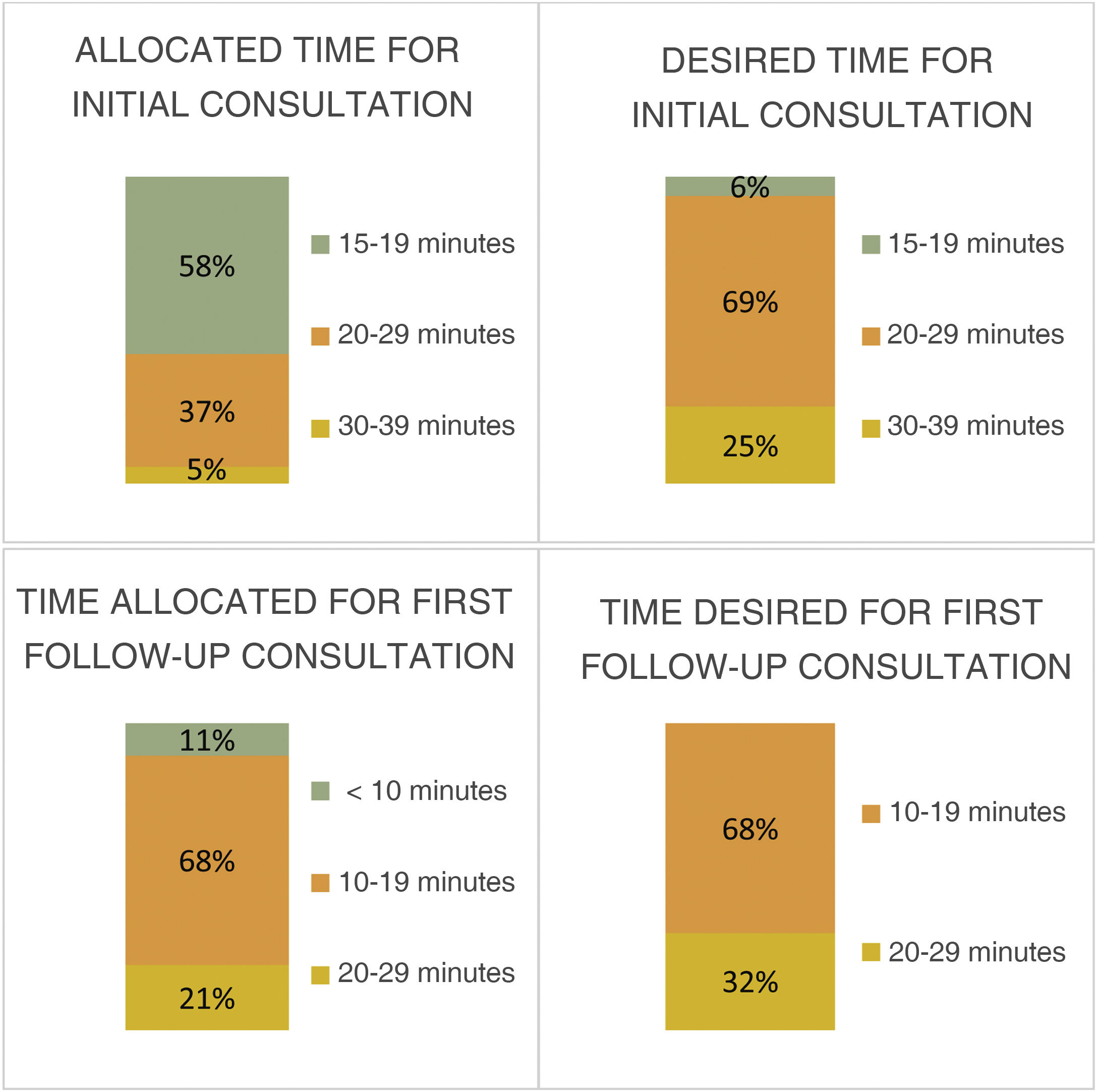
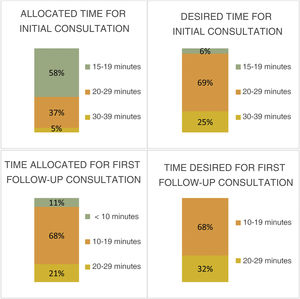
Fifty-seven percent of respondents considered the time allocated for the first assessment (less than 20 minutes) to be insufficient; 35% reported that 20–29 minutes were allocated for the initial assessment, with a further 8% reporting time slots of 30–39 minutes. Furthermore, 84% of respondents expressed a wish for more time to conduct these initial assessments (57%, 20–29 minutes; 27%, 30–39 minutes). However, they were satisfied with the time allocated for the first follow-up assessment (95%; less than 20 minutes).
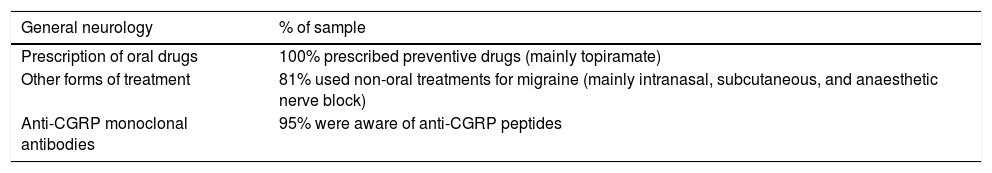
The most frequent reason for consultation was migraine, with 46% of respondents reporting that this disorder accounted for 50%–75% of all monthly patient assessments; all respondents were aware of and prescribed preventive drugs for migraine (topiramate was the most widely used option, followed by such other drugs as flunarizine and amitriptyline). Eighty-one percent of respondents used administration routes other than the oral route (subcutaneous, intranasal, nerve block, etc.), and 95% were aware of the new monoclonal antibodies and considered them a treatment option (Table 2).
Headache management by general neurologists.
| General neurology | % of sample |
|---|---|
| Prescription of oral drugs | 100% prescribed preventive drugs (mainly topiramate) |
| Other forms of treatment | 81% used non-oral treatments for migraine (mainly intranasal, subcutaneous, and anaesthetic nerve block) |
| Anti-CGRP monoclonal antibodies | 95% were aware of anti-CGRP peptides |
The existence of protocols for the referral of patients with headache from primary care to the neurology department were reported by 62% of the sample, with protocols for referral from emergency departments reported by 49% of respondents and referral from other departments reported by 16%. A total of 81% of respondents reported that their hospitals had headache units, with 70% reporting the existence of criteria for referral to these units. Ninety-two percent of respondents considered the existence of these specialist units to be necessary to improving care provision for these patients, and 95% had referred patients to headache units in the past.
Finally, all respondents considered that they provided their patients with sufficient information to understand and manage their headache, with 60% also sharing reliable sources of information on the disorder. All respondents were interested in attending training courses on headache.
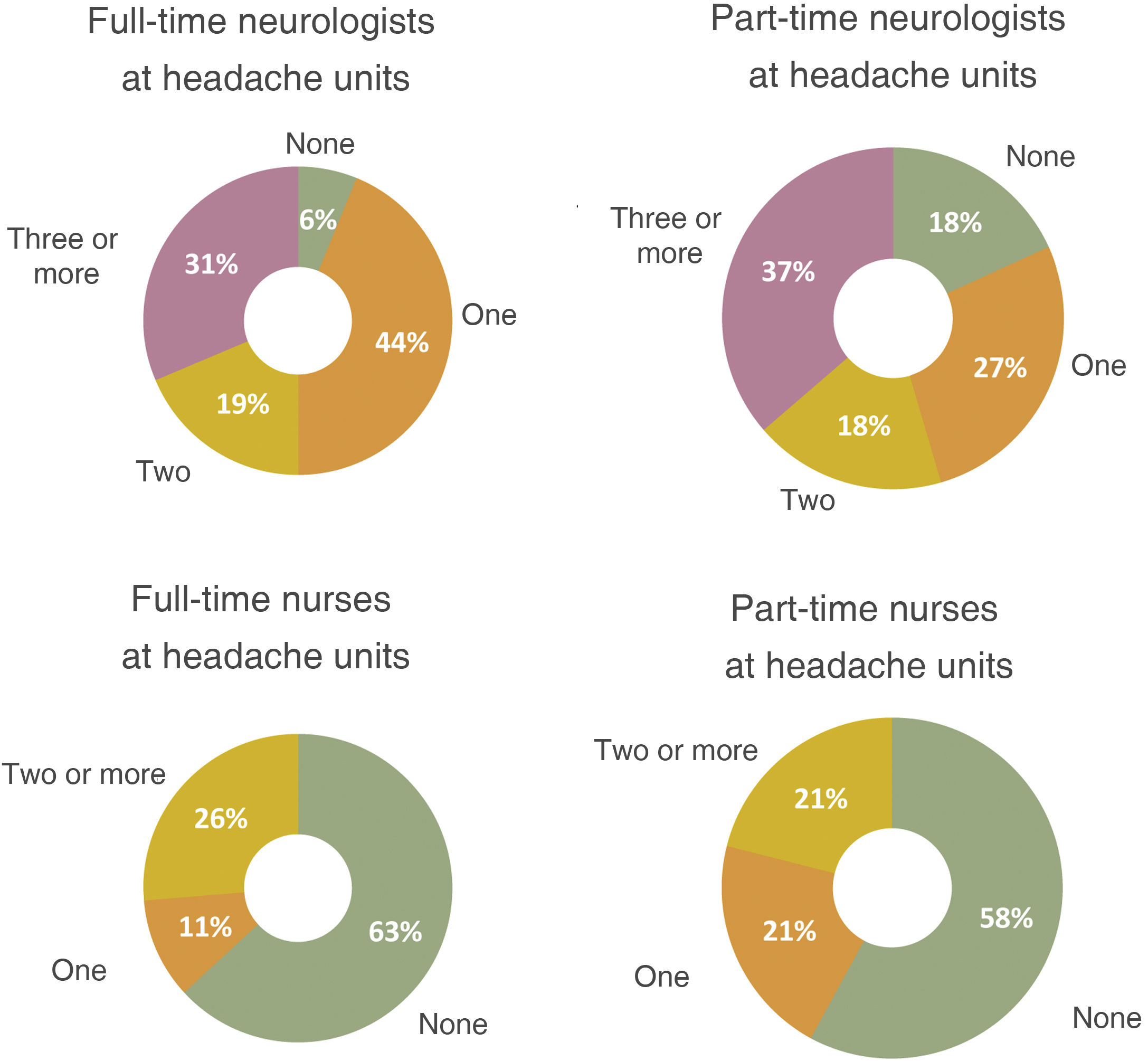
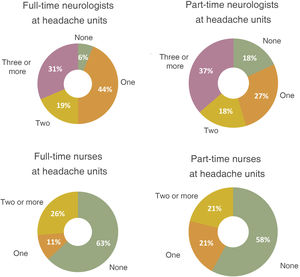
Headache unit neurologistsThe majority of headache units/clinics represented in our sample (94%) had at least one full-time neurologist on their staff, had a specific consultation room (79%), and held at least one or 2 specific consultation sessions per week (74%). However, over half of these units did not have full-time nursing staff (63%) or a nursing consultation room (79%) (Fig. 5).
Regarding access to other specialties for multidisciplinary care, headache units worked in cooperation with neurosurgery departments in 100% of cases, ophthalmology in 100%, and neuro-radiology in 95%. Lower percentages were reported for mental health services (79%), with very limited access to psychology techniques and treatments (16%).
Patients were most frequently referred to these units from general neurology departments (74%), with a mean delay of 1–3 months until the first ordinary consultation (73%) and <30 days until the first priority consultation (78%); nearly half of units (47%) had differentiated waiting lists for each priority level (see Fig. 4 for further detail).
As observed among general neurologists, the majority of headache specialists considered the time allocated for the initial visit to be insufficient (58%, 15–19 minutes; 37%, 20–29 minutes; 5%, 30–39 minutes) and that more time was needed (69%, 20–29 minutes; 25%, 30–39 minutes) (Fig. 6).
Special access to these units was available for specific disorders, such as cluster headache (85%), headache during pregnancy (77%), and trigeminal neuralgia (62%). Referral protocols were in place in over half of units (53%). At all units, a diagnosis was established after the first assessment (100%), and subsequently reviewed (where necessary) at subsequent consultations (100%) according to the updated International Classification of Headache Disorders (95%).
Regarding daily practice, 95% of headache specialists used headache diaries at their consultations. The main method used to evaluate treatment outcomes in their patients was assessment of the response of their symptoms without using scales (69%), with 31% of specialists using disability scales and 19% using quality of life scales. All respondents stated that patients in their units received information about their disorders, through the recommendation of information sources (39%) or web pages (37%), or the provision of specific pamphlets developed by the staff of the unit (42%). The specific treatments that were most widely used at headache units included botulinum toxin infiltrations for chronic migraine (95%) and other indications (89%), anaesthetic pericranial nerve block (84%), trigger point block and myofascial dry needling (58%), and neurostimulator implantation (44%).
Overall, 75% of headache specialists conducted teaching activity, whereas fewer than half (47%) combined their care activity with clinical research. All headache specialists were members of SANCE, with 47% also being members of the Headache Study Group of the Spanish Society of Neurology (GECSEN, for its Spanish initials). Seventy-four percent of units recorded complications associated with the procedures and treatments used. In terms of administration, staff satisfaction surveys were conducted at 32% of headache units. More than half (52%) specifically measured the unit’s activity, whereas 6% tracked spending as part of a cost-efficiency policy. Twenty-two percent of headache unit neurologists drafted global reports of activity at their unit.
DiscussionOur results demonstrate that headache in general, and migraine in particular, are a frequent reason for consultation at all 4 of the levels of hospital care included in the study. Regarding the epidemiology of migraine in Spain, one of the first prevalence studies was conducted in 1986 in southern Madrid14; further studies have since been published. In 2006, the Spanish National Health Survey established the prevalence of migraine at 11.2%, considerably higher than the rates reported before 2003 (6.54%). The PALM programme, which began the same year,11,12 aimed to establish the status of migraine in Spain through a telephone survey developed and approved by a scientific committee according to the criteria proposed by Lipton et al.15 The survey was completed by 70 692 individuals, and yielded important data on the current situation of migraine in Spain, its prevalence and influence on patients’ work, the most commonly used treatments, and patients’ level of understanding of the disorder. The results of the present study underscore the status of migraine as a frequent reason for consultation at primary care centres and the magnitude of its societal repercussions, given the considerable overburdening of this branch of medicine. The percentage of patients consulting with migraine was somewhat lower in emergency departments, which we may interpret as the result of the population being mindful to avoid overburdening these services with an “unexceptional” disorder; it may also be the case that, despite the high prevalence of migraine, pain does not reach sufficient intensity for emergency consultation due to good medical/pharmacological control by the healthcare professionals surveyed.
In the management of these patients, the first priority is to establish at least a working diagnosis in order to provide appropriate treatment. In this regard, the results from primary care physicians are excellent, confirming that they prescribe different pharmacological and non-pharmacological treatments for migraine prevention (85%), and maintain these treatments for sufficient time to establish treatment response/lack of response (58%). The most commonly used drugs were amitriptyline and flunarizine, as was also the case in emergency departments. These high rates of prescription, together with the fact that only 20% of patient referrals to neurology departments were due to the lack of a definitive diagnosis, demonstrate the good understanding of migraine among primary care physicians. However, the great majority did refer patients to specialists (96%), with over half reporting that this was due to failure of a reasonable number of treatments (≥ 2 drugs in 55% of respondents); this situation is not aligned with the recommendations of the European Headache Federation, which establishes that non-specialist physicians should be able to provide satisfactory care to 90% of patients with headache and competently diagnose and manage the majority of cases of migraine and tension-type headache.16
Primary care physicians prescribed oral preventive drugs less frequently than emergency department physicians (60%); however, knowledge of other management techniques was similarly low in both groups (43% in primary care and 34% in emergency departments), with few professionals knowing and using preventive methods other than oral medication (acupuncture, botulinum toxin, lifestyle/dietary interventions, etc.). The limited knowledge of these “unconventional” techniques among primary care professionals is striking. For this reason, it would be beneficial to run training courses to broaden physicians’ knowledge about other techniques and treatments; the physicians surveyed expressed great interest in such courses (97% among primary care physicians and 100% among emergency department physicians).
The percentage of specialist referrals from the emergency department (14%) was also clearly lower than that observed in primary care; these numbers are too low and may have negative repercussions for patients. One potential explanation for these low percentages may be the lack of consensus referral protocols at the emergency departments included in the study (29%); implementation of these processes by hospital headache units would optimise the multidisciplinary management of these patients.
As observed in the study by Pérez-Pereda et al.17 and in the PALM study,11,12 primary care is the main source of referrals to neurology departments. However, we observed lower percentages than those reported by other authors (65%, vs 82% in the study by Pérez-Pereda et al. and 70% in the PALM study); this may be interpreted either positively (professionals are capable of managing these patients) or negatively (patients are not referred despite poor symptom control).
The most indicated strategy for migraine management is stratified care, which recommends tailoring treatment according to the degree of disability caused by migraine in each patient18; however, the use of clinical scales to evaluate treatment response is not widespread among healthcare professionals, as shown by several studies.11,12,19 Only 32% of headache specialists in our series reported using headache impact/disability scales, and just 21% used quality of life scales; these results are consistent with those reported in the PALM study,11,12 in which only 17% used such scales. However, up to 95% of respondents to our survey provided their patients with headache diaries, a clearly higher percentage than that observed in the PALM study (57%), enabling better follow-up.
Regarding organisational matters, waiting times for the first specialist consultation (mean of 1–3 months: 58% of general neurologists and 73% of headache specialists) are practically inevitable, given the lack of resources in our healthcare system. As mentioned previously, these waits could be reduced through the implementation of voluntary training courses to increase healthcare professionals’ autonomy in managing these patients, which would undoubtedly result in considerable reductions in the number of referrals and, consequently, in waiting lists. The economic limitations facing the healthcare system also negatively affect the time allocated for consultations; this was a generalised complaint among survey respondents, with over half considering the time allocated to be insufficient (57% of general neurologists and 58% of headache specialists reported time allocations of < 20 minutes per consultation); this stands in contrast to the findings of the PALM study,11,12 in which neurologists dedicated a mean of approximately 23 minutes to initial consultations with patients with suspected migraine. According to the Second National Strategic Plan for the Integral Treatment of Neurological Diseases, published by the Spanish Society of Neurology in 2017, the desired time allocation for an initial consultation would be at least 40 minutes, with a minimum of 20 minutes for follow-up consultations. These theoretical figures contrast with those observed in our study, with only 27% of general neurologists and 25% of headache specialists stating that they would desire time allocations longer than 30 minutes for the first consultation, probably because they are aware of the current overburdening of the healthcare system in Andalusia, which makes such long consultations seem somewhat implausible. Despite the consensus recommendations mentioned above, we may interpret this simply as a sense of resignation about the current lack of resources.20
The budgetary limitations of the healthcare system also have an impact on headache units. Only half of our sample of headache units had 2 or more full-time neurologists on their staff, which may be deemed insufficient in the light of the large volume of patients requiring care from this subspecialty. In this regard, headache and especially migraine constitute one of the areas with the greatest potential for growth and, in turn, an increasingly relevant area of clinical research in the coming years. Numerous studies and clinical trials suggest that nurses will play an increasingly important role in the staffing of headache units. Despite this, a high percentage of respondents (63%) stated that their units had no nursing staff involved in this clinical/research activity, although fewer than half of respondents (47%) conducted research activities at their respective centres.
Looking beyond migraine, we observed a higher degree of consensus between the different groups of professionals regarding other primary headaches, such as trigeminal neuralgia and cluster headache: practically all respondents knew how to recognise and diagnose these entities (96% for cluster headache and 98% for trigeminal neuralgia among primary care physicians; 91% for cluster headache and 100% for trigeminal neuralgia among emergency department physicians) and prescribed pharmacological treatment in accordance with the latest clinical practice guidelines.
Finally, our results as a whole show that healthcare professionals are highly interested in headache and in expanding their knowledge on the subject (97% in primary care, 100% in emergency departments, and 100% in general neurology departments), which is often limited due to a lack of economic resources enabling access to training. This situation can and should be addressed, and all of us, as members of the public health system, must take on our share of the responsibility. It would be interesting for each healthcare district to consider running training courses at different health centres and emergency departments; the content of such courses should be fundamentally practical, seeking to meet the training needs of healthcare professionals in these settings. Update sessions should also be held periodically.
Regarding this point, we have seen how, in addition to being the most frequent reason for neurology consultations, headache is also a frequent reason for primary care consultation; therefore, good organisation in both levels of care is essential. There is a need to find new forms of bilateral communication in order to improve coordination between the different care settings considered in our study. For instance, direct (electronic) contact between primary care centres and headache units would shorten administrative processes, avoiding unnecessary appointments and enabling the prioritisation of cases requiring fast access to care, thus promoting integral care for patients with headache.21,22 As part of the Pytes study, our research group has developed a telemedicine project including headache units and primary care centres.23,24 This approach is not a novelty, with similar initiatives having been implemented in other countries. For instance, Minen et al.25 evaluated primary care physicians’ level of knowledge of headache and training needs through 3 sessions, using their findings to design specific training programmes. In Spain, Pedraza et al.26 proposed an e-mail–based option promoting direct contact between primary care physicians and headache units.
The main limitation of our study is its cross-sectional design, evaluating information on past experience; the sample is small, and is made up of healthcare professionals who responded to an invitation to participate sent to all members of the SAN (56/250). Therefore, the study lacked clearly defined inclusion and exclusion criteria. Furthermore, questionnaires were not administered by a rater and included different questions depending on the specific target population, preventing us from performing a statistical comparison between groups to establish more general conclusions. Furthermore, the data presented do not contribute epidemiological information; rather, they are based on estimations made by survey respondents. The ordinal design of the questionnaire may have negatively affected the accuracy of some responses. All of the above, together with the good outcomes from headache management in primary care and at emergency departments, may reflect a special interest in headache disorders among the participating healthcare professionals.
ConclusionsAndalusia is Spain’s most populous and second-largest autonomous community; its economy is marked by disadvantages with respect to the wider Spanish and European contexts, which also affects the regional health service in general and neurology departments in particular.
The lack of economic and healthcare resources in Andalusia explains the high care burden on our professionals, with limited staffing, long waiting lists, and limited time for assessment of patients with headache, despite the disorder being a frequent reason for consultation.
It would be beneficial to consider introducing training courses on a large scale with a view to increasing the autonomy of healthcare staff in managing these patients, reducing the number of specialist referrals and the length of waiting lists. Direct (electronic) contact between primary care centres and headache units would accelerate administrative processes, avoiding unnecessary appointments and enabling the prioritisation of patients requiring fast access to care, thus promoting integral care for patients with headache.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.