We analyze the diagnostic utility of urgent EEG (electroencephalogram) performed in children under 16 years of age in our center.
Material and methodsDescriptive, retrospective, observational study of consecutive patients from 0 to 16 years of age, who underwent an urgent EEG for any reason, from January to December 2022.
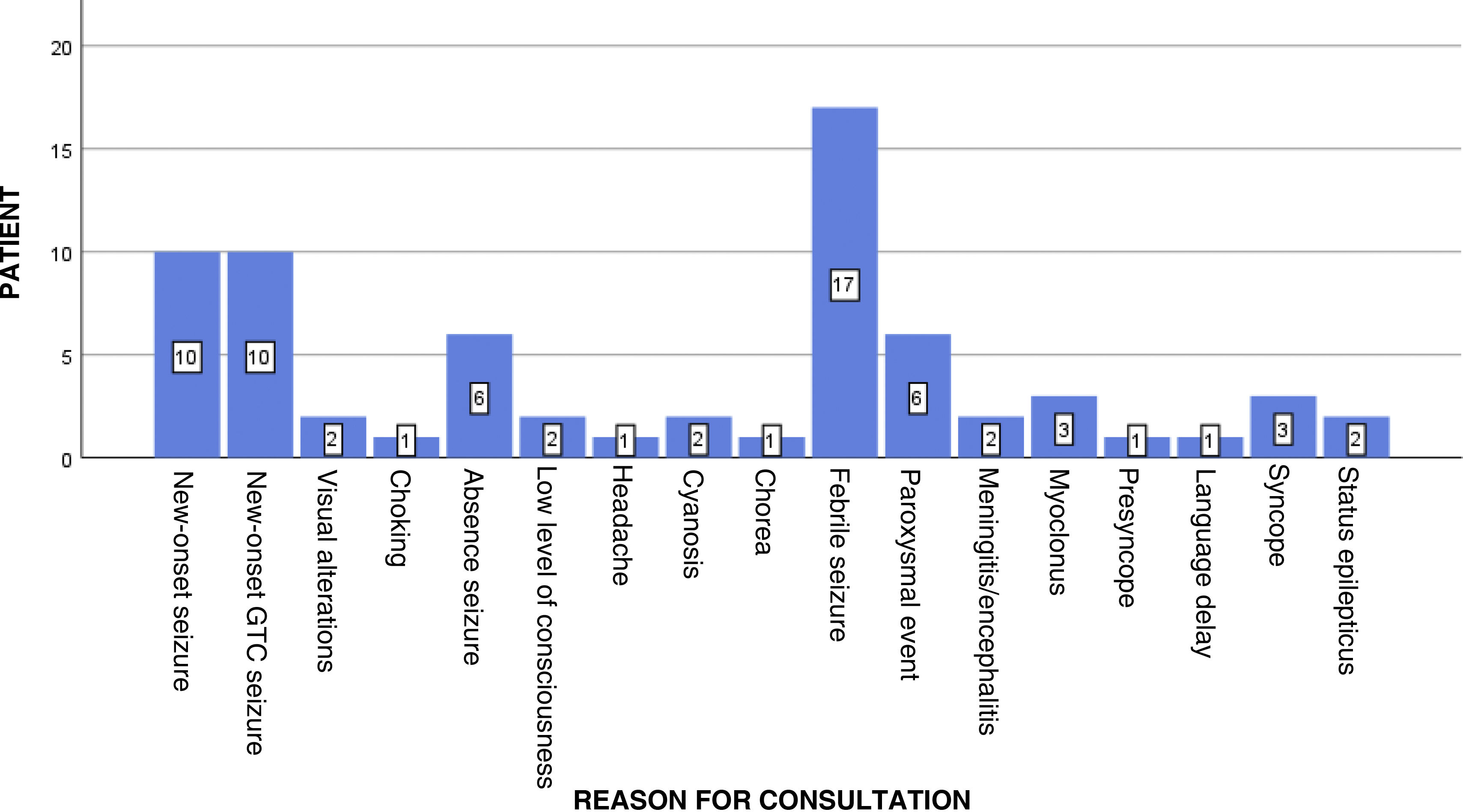
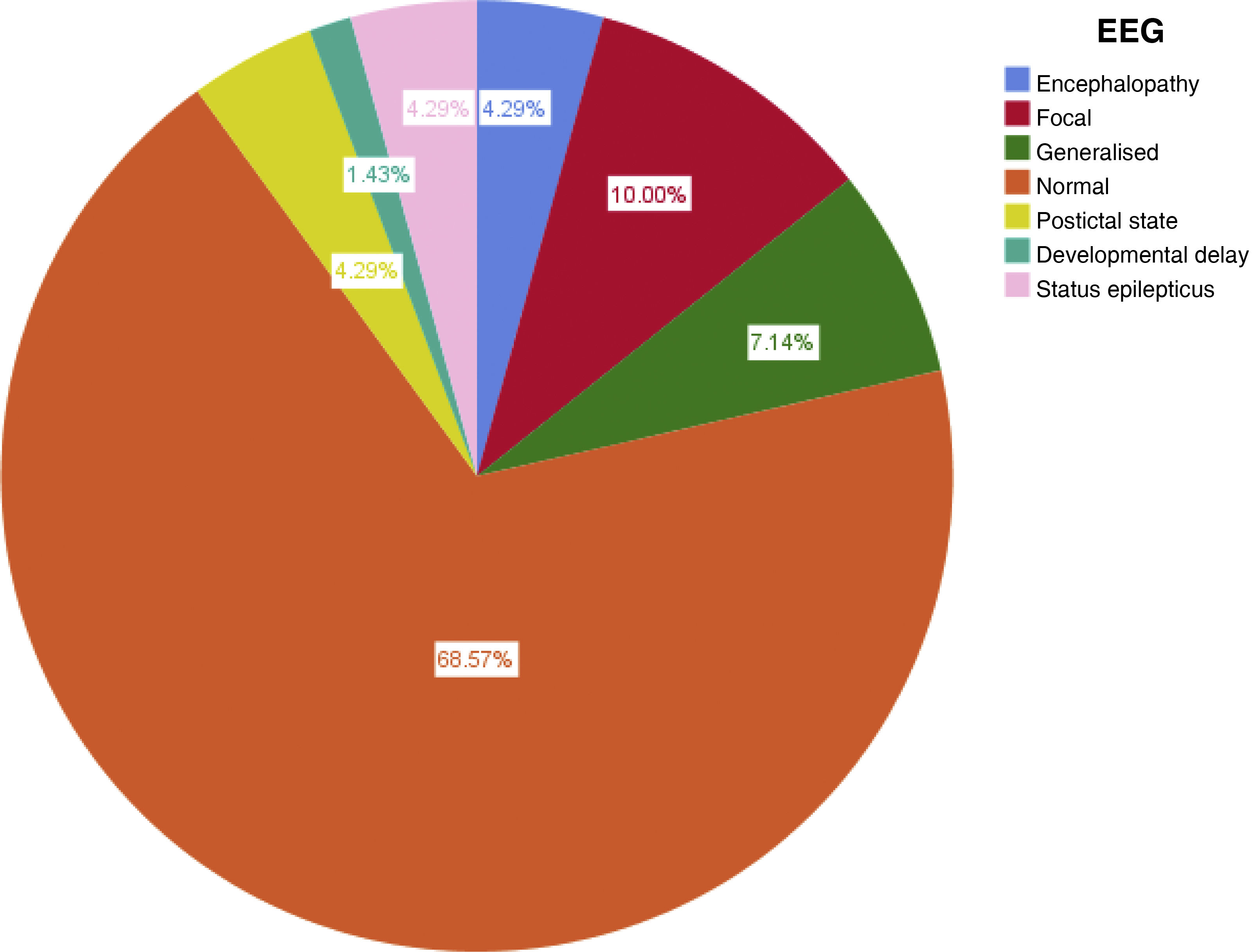
ResultsOf the 388 patients, 70 were children: 37 (52.85%) women, and 33 (47.14%) men. Average age: 6.27 ± 4.809. Of the 70 patients, 6 (8.57%) had previous epilepsy. Reasons for consultation: 17 febrile seizures, 10 first focal seizures, 10 first TCG seizures, 6 paroxysmal episodes, 6 absences, 3 myoclonus of extremities, 3 syncope, 2 SE, 2 visual alterations, 2 low level of consciousness, 2 cyanosis, 2 suspected meningitis or encephalitis, 1 choking, 1 atypical headache, 1 chorea, 1 presyncope, 1 language delay. Of the 70 patients, 47 had a normal EEG (67.14%). Of the 47 patients with a normal EEG, 10 were diagnosed with epilepsy, and 3 of them began receiving antiepileptic treatment upon discharge. None of the patients with suspected syncope or paroxysmal disorder (17 patients, 24.28%) had EEG abnormalities. Of the 17 patients with atypical febrile seizures, 3 had EEG abnormalities.
ConclusionsA third of the EEG records performed in the Emergency Department showed alterations, probably due to the time taken. Almost half of the patients with suspected epilepsy or EE showed EEG abnormalities, which confirmed the diagnosis in these cases and encouraged the clinician to start drug treatment. No case with a high suspicion of epilepsy was dismissed due to the normality of the EEG recording in our series. No patient diagnosed with syncope or paroxysmal disorder had EEG abnormalities. Nearly a quarter of patients with atypical febrile seizures showed EEG abnormalities. We barely register cases of status epilepticus, probably due to the degree of complexity of our center.
Analizamos la utilidad diagnóstica del EEG urgente realizado en niños menores de 16 años en nuestro centro.
Material y métodosEstudio descriptivo retrospectivo, observacional, de pacientes consecutivos de 0 a 16 años, a los que se ha realizado un EEG urgente de enero a diciembre de 2022.
ResultadosDe los 388 pacientes, 70 niños: 37 (52,85%) mujeres, y 33 (47,14%) hombres. Edad media: 6,27 ± 4,809. De los 70 pacientes, 6 (8,57%) tenían epilepsia previa. Motivos de consulta: 17 crisis febriles, 10 primeras crisis focales, 10 primeras crisis TCG, 6 episodios paroxísticos, 6 ausencias, 3 mioclonías de extremidades, 3 síncopes, 2 EE, 2 alteraciones visuales, 2 bajo nivel de conciencia, 2 cianosis, 2 sospechas de meningitis o encefalitis, 1 atragantamiento, 1 cefalea atípica, 1 corea, 1 presíncope, 1 retraso del lenguaje. De los 70 pacientes, 47 tuvieron un EEG normal (67,14%). De los 47 pacientes con EEG normal, 10 fueron diagnosticados de epilepsia. Ningún caso de los pacientes con sospecha de síncope o trastorno paroxístico (17 pacientes, 24,28%) tuvo alteraciones en el EEG. De los 17 pacientes con crisis febriles atípicas, 3 tenían alteraciones en EEG.
ConclusionesUn tercio de los registros EEG realizados en Urgencias mostraron alteraciones. Casi la mitad de pacientes con sospecha de epilepsia o EE mostraba anomalías en el EEG, lo que confirmó el diagnóstico en estos casos y favoreció que el clínico iniciara el tratamiento farmacológico. Ningún caso con alta sospecha de epilepsia fue descartado por la normalidad del registro EEG en nuestra serie. Ningún paciente con diagnóstico de síncope o trastorno paroxístico tuvo alteraciones en el EEG. Casi una cuarta parte de los pacientes con crisis febriles atípicas mostraron alteraciones en el EEG.
Electroencephalography (EEG) is a well-known and widely used diagnostic tool, mainly indicated for the analysis of new-onset seizures, status epilepticus (SE; focal or generalised), seizure clusters, high-risk epilepsy, encephalopathy, and low level of consciousness.1–13 Its accuracy increases the sooner it is performed after the acute seizure (first 24−48 hours). At the emergency department, it is especially useful for diagnosing SE, and particularly non-convulsive SE.
EEG is increasingly being used in other indications not directly associated with epilepsy. Given the challenge of history taking in paediatric patients, and especially in infants and children younger than 5 years, the availability of a technically simple, painless test not requiring sedation may be very useful for other conditions.
Most published studies focus on the usefulness of EEG in specific patient groups, and do not provide an overall view of its value for different aetiologies at a paediatric emergency department.14–23 Assessing the accuracy of neurological diagnostic tests performed in each centre is very useful, not only for physicians working there but also for other professionals to assess and compare the results.
We analyse the diagnostic usefulness of EEG recording at the emergency department in children aged 16 years or younger at our hospital.
Materials and methodsThis is a descriptive, observational, retrospective study of consecutive patients aged 0 to 16 years who underwent emergency EEG at our hospital for any reason, either at the emergency department, on the inpatient ward, or in outpatient consultations. The inclusion period was from January to December 2022.
The variables analysed were: age of the patient, sex, history of epilepsy, age at epilepsy diagnosis, previous treatment with antiepileptic drugs (AED), reason for consultation, time of EEG performance (24 or 48 hours), EEG alterations, final diagnosis, emergency treatment received, treatment at discharge, hospital or ICU admission, department requesting the study, and death.
The duration of the EEG study at the emergency department was 20 minutes in all cases, with longer studies (30 minutes) reserved only for cases of suspected SE.
Data were processed using the SPSS statistics software, version 25.0 (IBM). Categorical variables are expressed as frequencies and percentages, and continuous variables as mean (standard deviation [SD]). The chi-square test was used to evaluate associations between qualitative variables, and the t-test was used for quantitative variables. A specific database was created for the statistical analysis, and data were anonymised and grouped in accordance with Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016.
This study was approved by our centre’s research committee (May 2023).
ResultsWe identified a total of 418 emergency EEG studies during the study period. Of this total, 388 are different patients, and 20 are registries of patients who underwent another emergency study on the same day or very soon after.
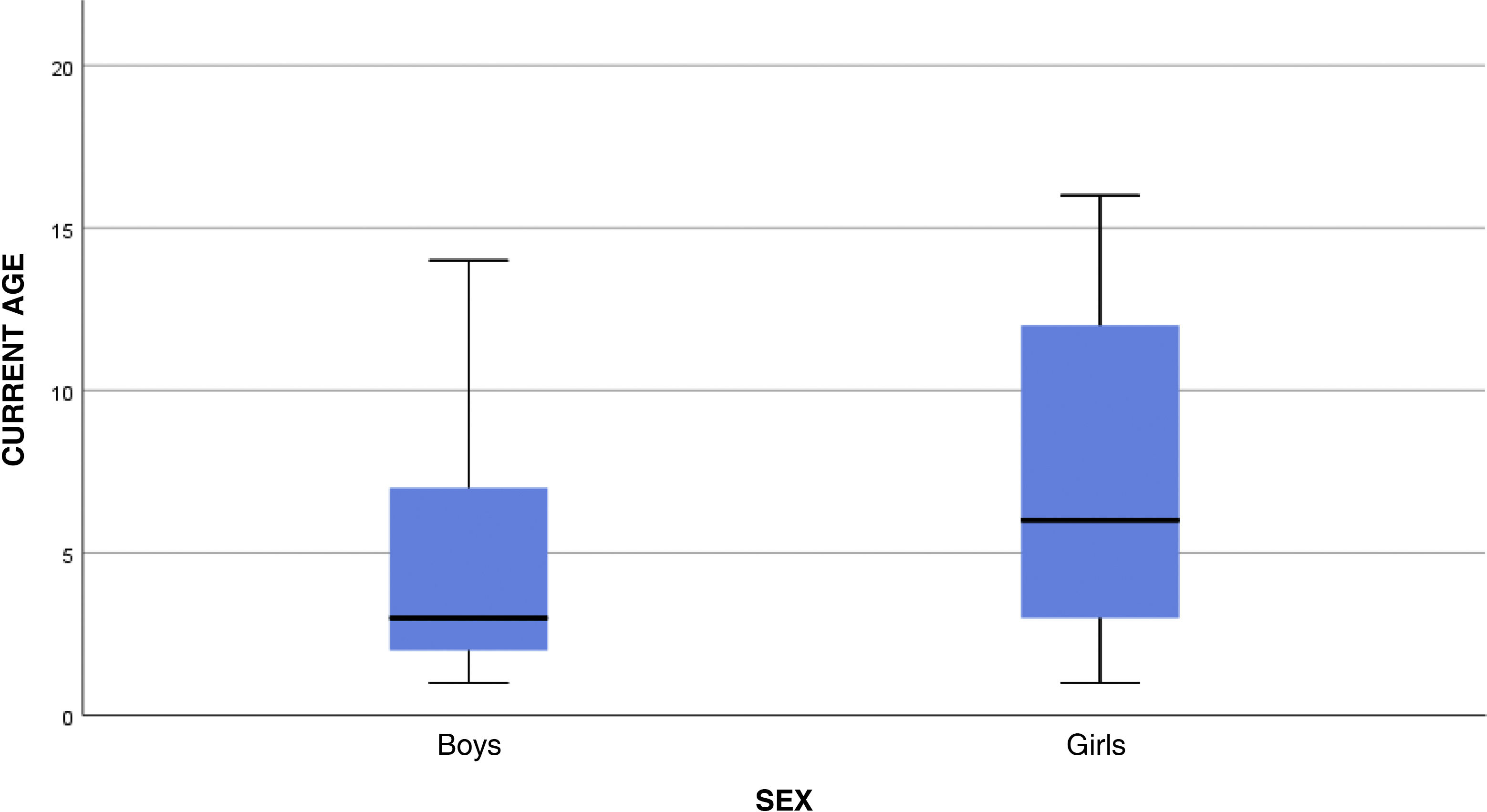
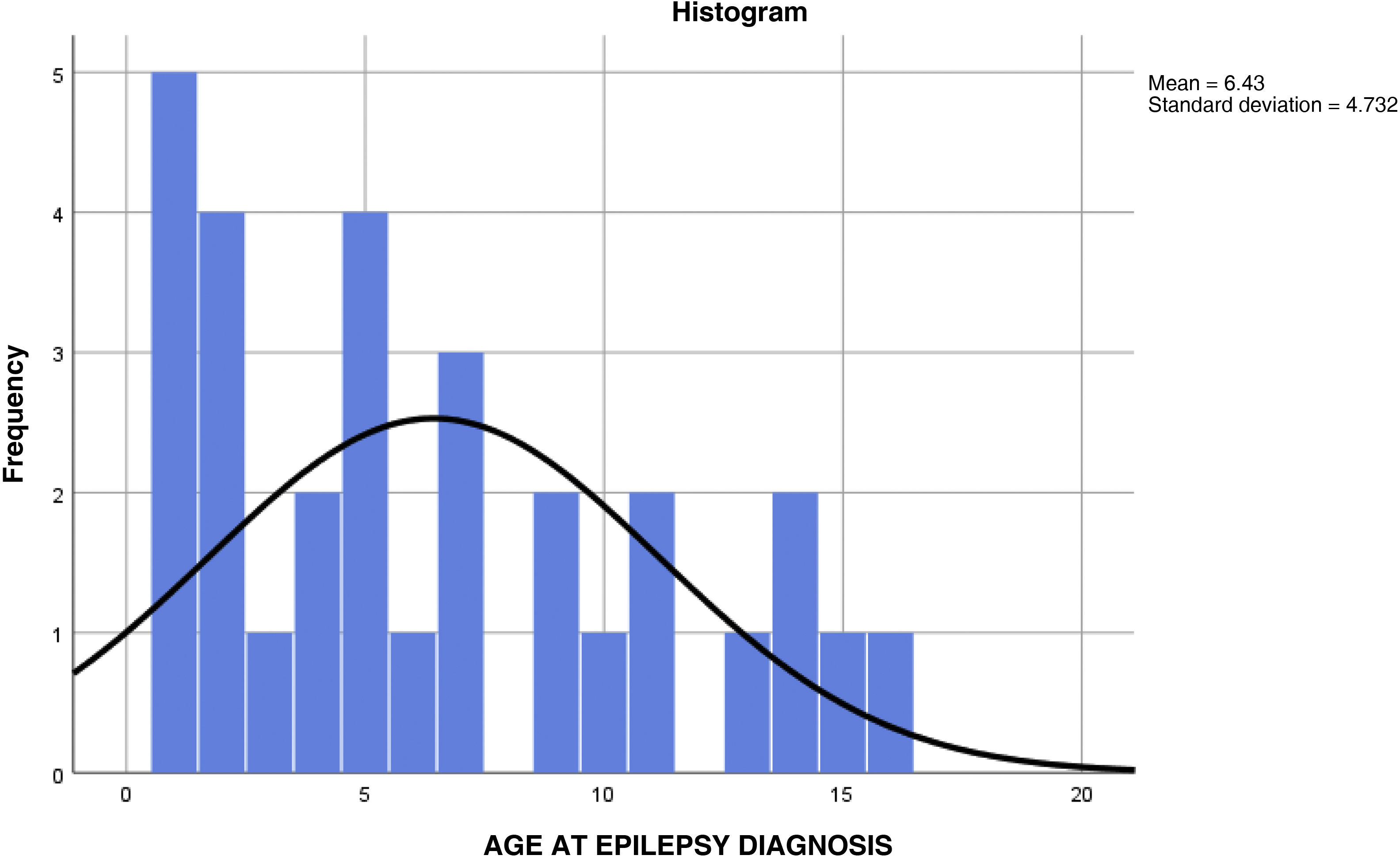
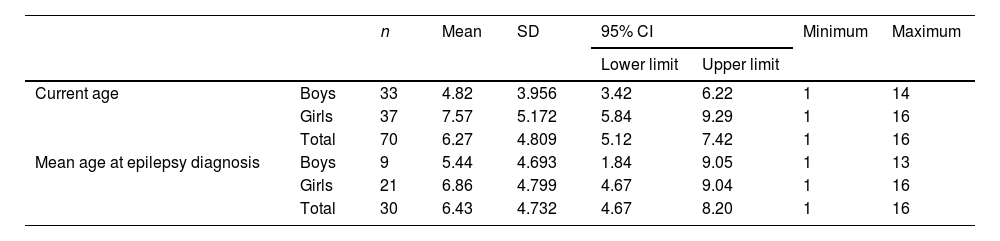
Of the 388 patients, 70 (18.04%) were aged 16 years or younger, and 318 (81.95%) were older than 16 years. Of these 70 paediatric patients, 37 (52.85%) were girls and 33 (47.14%) were boys. Mean age at the time of EEG performance was 6.27 (4.809) years (Fig. 1). Mean age at epilepsy diagnosis was 6.43 (4.732) years (Table 1).
Mean age at epilepsy diagnosis and at EEG performance at the emergency department, adjusted by sex.
| n | Mean | SD | 95% CI | Minimum | Maximum | |||
|---|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||||
| Current age | Boys | 33 | 4.82 | 3.956 | 3.42 | 6.22 | 1 | 14 |
| Girls | 37 | 7.57 | 5.172 | 5.84 | 9.29 | 1 | 16 | |
| Total | 70 | 6.27 | 4.809 | 5.12 | 7.42 | 1 | 16 | |
| Mean age at epilepsy diagnosis | Boys | 9 | 5.44 | 4.693 | 1.84 | 9.05 | 1 | 13 |
| Girls | 21 | 6.86 | 4.799 | 4.67 | 9.04 | 1 | 16 | |
| Total | 30 | 6.43 | 4.732 | 4.67 | 8.20 | 1 | 16 | |
CI: confidence interval; SD: standard deviation.
Of the 70 patients, 6 (8.57%) had history of epilepsy (2 focal epilepsy, one generalised epilepsy, one case of possible metabolic epilepsy under study, and 2 of parainfectious aetiology) (Fig. 2). Of these, 4 (5.71%) were previously receiving an AED (one lacosamide, one lamotrigine, one perampanel, and one levetiracetam).
Of the 70 EEG studies, 18 (25.71%) were performed in admitted patients, 48 (68.57%) at the emergency department, and the remaining 4 (5.71%) were requested by outpatient consultations. In terms of time of performance, 67 (95.71%) were performed within the first 24 hours, and 3 (4.28%) within 48 hours after the event.
Reasons for consultation included febrile seizures (17 patients), new-onset focal seizures (10), new-onset generalised tonic-clonic seizures (10), paroxysmal events (6), absence seizures (6), myoclonus of the limbs (3), syncope (3), clinical symptoms of SE (2), visual alterations (2), low level of consciousness (2), cyanosis (2), suspected meningitis or encephalitis (2), choking (1), atypical headache (1), choreic movements (1), presyncope (1), and language delay (1) (Fig. 3).
Of the 70 studies, 47 yielded normal results (67.14%). The findings in the remaining 23 were epileptiform abnormalities in the EEG in 15 patients (28.57%), metabolic encephalopathy criteria in 2 (2.85%), postictal state in 3 (4.28%), and diagnosis of electrical status epilepticus in 3 (4.28%) (Fig. 4). Of the 15 patients with epileptiform abnormalities, 3 showed generalised spike-wave discharges at 4−5 Hz, 5 presented polyspike or spike-wave abnormalities in the left temporal region, 3 showed alterations in the left frontal region, 2 presented right fronto-temporal abnormalities, and 2 displayed right parieto-occipital abnormalities.
Aetiology was metabolic in the 2 patients presenting symptoms of encephalopathy with altered EEG recording (generalised slowing with theta activity and generalised delta waves). The 3 patients diagnosed with SE showed a burst-suppression pattern of generalised activity in the EEG recording.
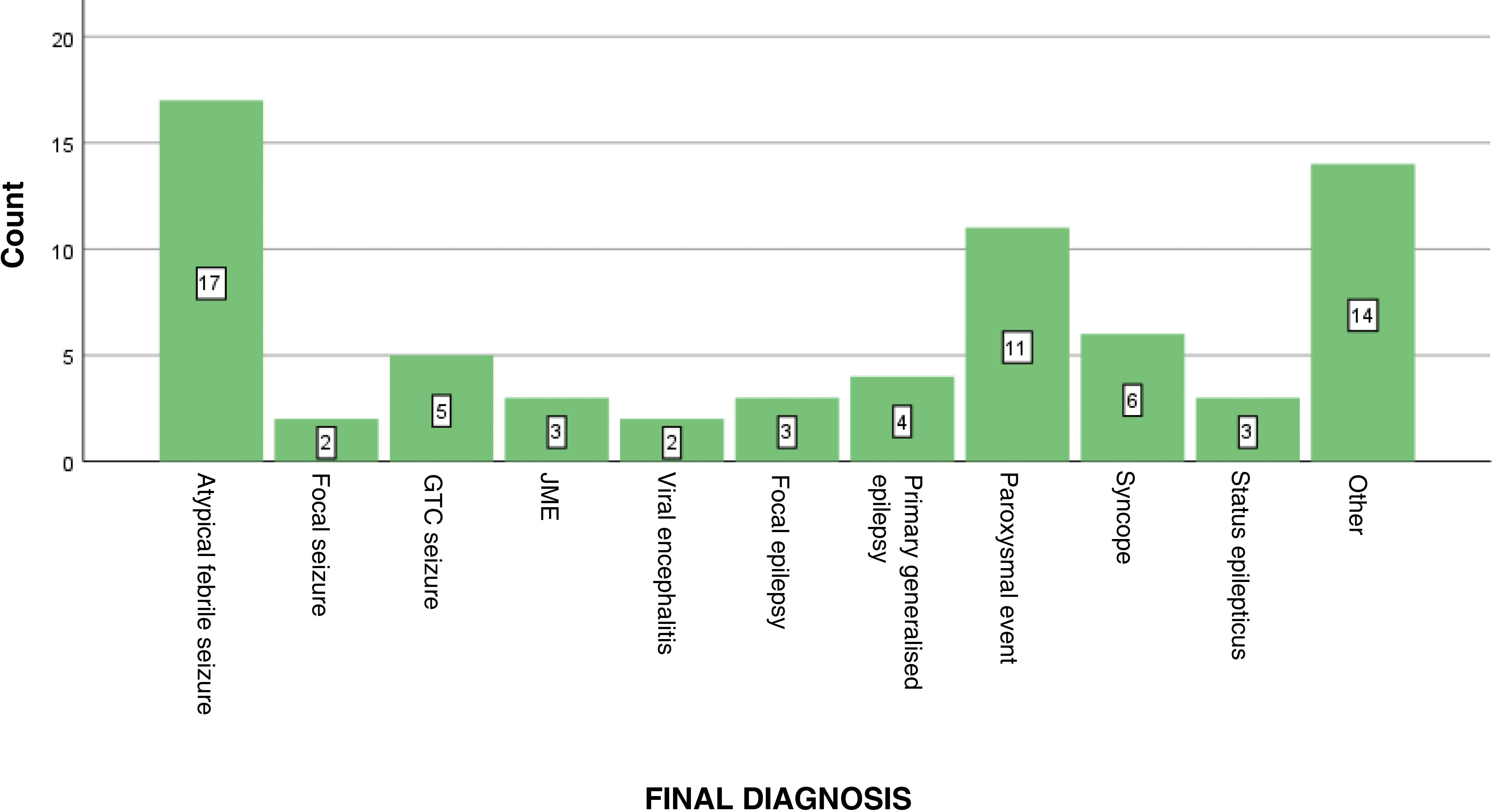
Final diagnoses were as follows: atypical febrile seizures in 17 patients, new-onset isolated focal seizures in 2, generalised tonic-clonic seizures in 5, juvenile myoclonic epilepsy in 3, viral encephalitis in 2, focal epilepsy in 3, primary generalised epilepsy in 4, paroxysmal events in 11, vasovagal syncope in 6, SE in 3, and other conditions in 14. These other conditions were milk allergy, visual hallucinations, ataxia and myoclonus under study, choking, atypical headache, probable chorea, probable confusional arousal, encephalitis of unknown aetiology, benign childhood epilepsy with paroxysms, acute gastroenteritis, Panayiotopoulos syndrome, post–COVID-19 paraesthesia, language delay under study, and diazepam intoxication (Fig. 5).
Of the 47 patients with suspected epilepsy, 20 showed EEG abnormalities; in 19 of these, diagnosis was clinically confirmed and specific treatment started (epilepsy, encephalopathy/encephalitis, or SE). None of the patients with suspected syncope or paroxysmal disorder (17 patients, 24.28%) presented EEG abnormalities. Of the 17 patients with atypical febrile seizures, 3 presented EEG alterations (2 displayed epileptic foci, and the other met criteria for encephalopathy).
Of the 47 patients with normal EEG results, 10 were diagnosed with epilepsy, and 3 of these received antiepileptic treatment at discharge. The remaining patients were only indicated occasional benzodiazepines for new seizures.
At the emergency department, 10 (14.28%) of the 70 patients received pharmacological treatment: valproic acid (1 patient), clobazam (1), intravenous (IV) midazolam (1), IV levetiracetam (2), IV diazepam (2), and IV clonazepam (3).
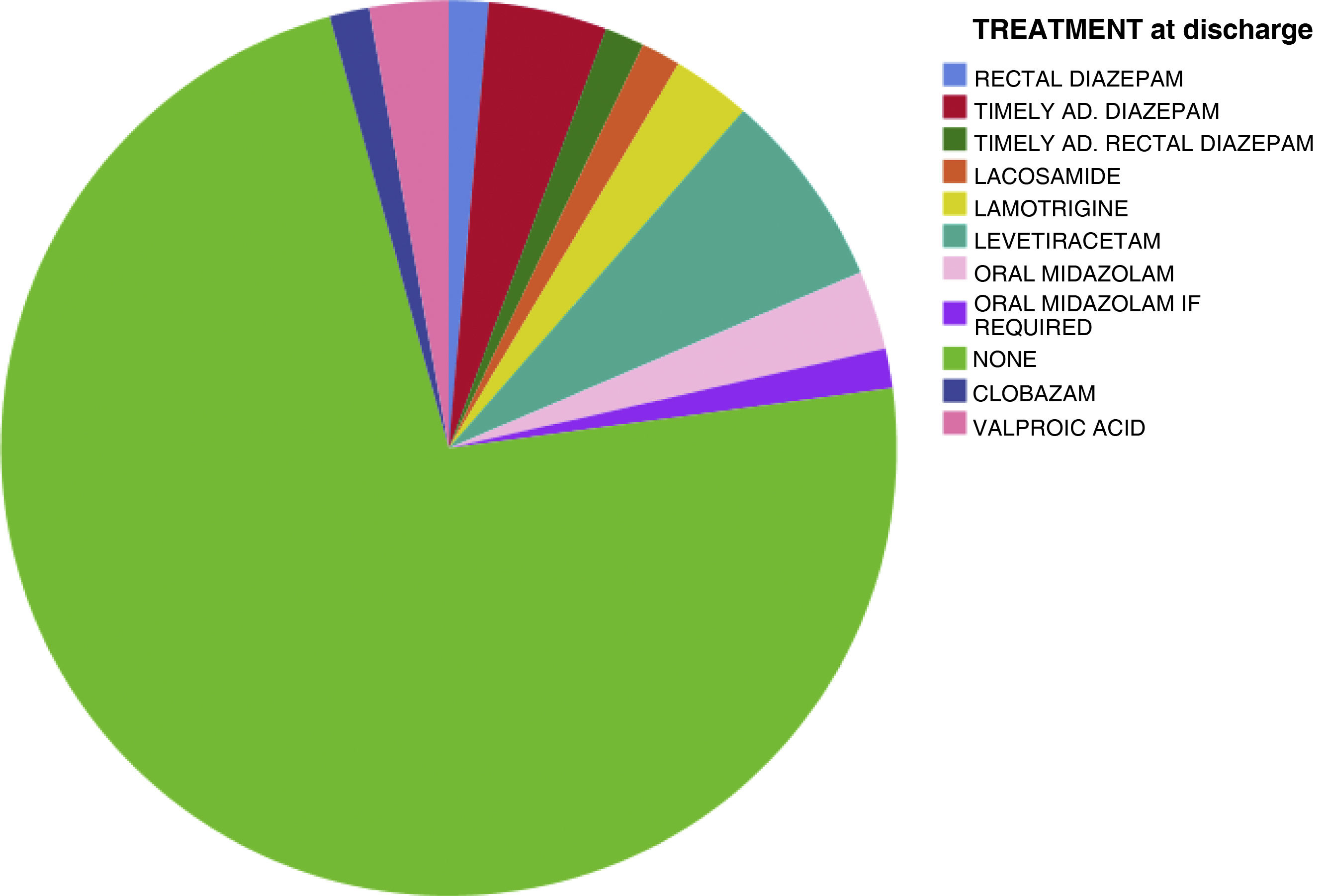
Of the 70 patients, 19 (27.14%) received antiepileptic treatment at discharge: valproic acid (2 patients), oral midazolam for new seizures (3), clobazam (1), occasional rectal diazepam for new seizures (5), oral levetiracetam (5), lamotrigine (2), and oral treatment with lacosamide (1) (Fig. 6).
Of the total 70 patients, 3 (4.28%) required ICU admission, and 35 (50%) were admitted to the paediatric or neurology ward to complete the diagnostic study. No death was reported in our series.
DiscussionAfter reviewing the emergency activity at our hospital’s paediatric department, we identified a very high number of consultations (approximately 40,000 annual visits, with a mean of 100–110 patients daily, and peaks of 150 patients daily in winter) for the size of the centre (267 beds) and the assigned population (325,000 people in 2022). Fortunately, the percentage of patients admitted due to more severe diseases to any hospital with a paediatric emergency department is typically very low (2%–5%).20–23 Considering the volume of patients attended, the number of EEG studies requested is low; this raised the question of what the main indications were and how accurate the study was in these cases.
Less than a tenth of patients in our series had previously been diagnosed with epilepsy; therefore, EEG was mainly requested for a de novo diagnosis, which was achieved in more than one-third of the patients. In patients with known epilepsy, EEG was indicated due to a change in the type of seizure or unusually long seizure duration.
The most surprising finding is that almost 25% of patients with atypical febrile seizures showed EEG alterations. The accuracy of EEG in our series seems higher than in previous series, probably due to the proximity to the event (almost all EEG studies were performed in the first 48 hours). Patients with paroxysmal events or syncope presented normal EEG results, as in previous series.17–20
Almost half of patients with strongly suspected epilepsy or SE presented EEG abnormalities, and diagnosis was clinically confirmed in nearly all of them, leading to specific antiepileptic treatment (epilepsy, encephalopathy/encephalitis, or SE); therefore, the accuracy of the test in this group of patients seems clear, and influences the physician’s approach. In the single patient with clinical suspicion and EEG abnormalities in whom diagnosis was not confirmed, this was due to dissociation between clinical symptoms and location of the EEG focus. In the remaining patients, clinical suspicion prevailed despite a normal EEG recording, pending confirmation in a follow-up visit to the paediatric neurology consultation scheduled at discharge. No case of strongly suspected epilepsy was ruled out due to normal EEG recordings at the emergency department; thus, clinical judgement continues to prevail in doubtful cases.
The percentage of SE in our series is very low, in terms of both clinical suspicion and final diagnosis. Many cases of refractory epilepsies, epileptic encephalopathies, and syndromic/metabolic diseases in paediatric patients are referred to tertiary care centres, so the low prevalence of SE in our centre may be associated with this degree of complexity.
The final diagnoses are very heterogeneous, although they are the typical diagnoses at the paediatric emergency department.3,4,8,9 In patients diagnosed with probable epilepsy (focal or generalised), the majority of treatments consisted of timely administration of benzodiazepines rather than preventive treatment with AED, according to the typical recommendations for this age group. If clinical doubts remained after a first emergency EEG recording showing normal results, a longer, sleep-deprived EEG recording (90 minutes) was indicated. In this series, no patient was directly referred from the emergency department for overnight video-EEG monitoring, as this resource is reserved for specialists at the paediatric neurology department.
One limitation of our study, in addition to its small sample size, is the variability in the reasons for consultations and final diagnoses, which complicated the analysis of results. Although the reasons for consultations were fairly clear, and may be grouped into frequent causes (febrile or afebrile seizures, syncope, paroxysmal events, etc), the final diagnoses were rather heterogeneous.
Another important limitation is the lack of follow-up of cases of SE in our series, as a result of which we do not know the aetiology and final outcome (all cases were transferred to other centres with paediatric ICU). With this in mind, the absence of mortality in our series may be due to underestimation.
The usefulness of emergency EEG in epileptic seizures is widely reported; however, the technique is also used in children whose symptoms are less specific, or difficult to categorise due to the challenging task of history-taking in this age group. We consider the study to offer an added value in these cases.
The size of our series is similar to those reported in other single-centre studies,16,17 although the majority analyse the usefulness of EEG in specific diseases at the emergency department.1–13 Few studies provide an overview of all reasons for EEG requests by the paediatric department, as in our study.14,15 The presence of those diagnoses that may not be considered typical in the neurology consultation (allergic reaction to milk protein, choking, cyanosis, etc.) reflects the difficulty of clinical management during childhood.
ConclusionsOne-third of the EEG recordings at the emergency department showed alterations, which is higher than the rates reported in other published series, probably due to the time of EEG performance. Almost half of patients with suspected epilepsy or SE showed EEG abnormalities, which confirmed the diagnosis in these cases and favoured the onset of pharmacological treatment. Strongly suspected epilepsy was not ruled out due to normal EEG recording in any case in our series.
No patient diagnosed with syncope or paroxysmal disorder presented EEG alterations. Almost 25% of patients with atypical febrile seizures showed EEG alterations. Very few cases of SE were recorded, probably due to our centre’s high degree of clinical complexity.