We report a case of a 41 year-old male patient, from the interior northern region of Portugal, with a past medical history of a left pulmonary resection at age of 16 (other hospital). He and his family were unable to give additional information about this past disease and medical records from the other institution were initially unavailable.
He was referred to the emergency department in August 2014 for neurosurgical evaluation due to recurrent symptoms of vomiting, headaches, anorexia and asthenia. A brain CT scan ordered by his general practitioner described a cystic lesion in the frontal lobe. The neurological exam was unremarkable and the patient was admitted for further studies.
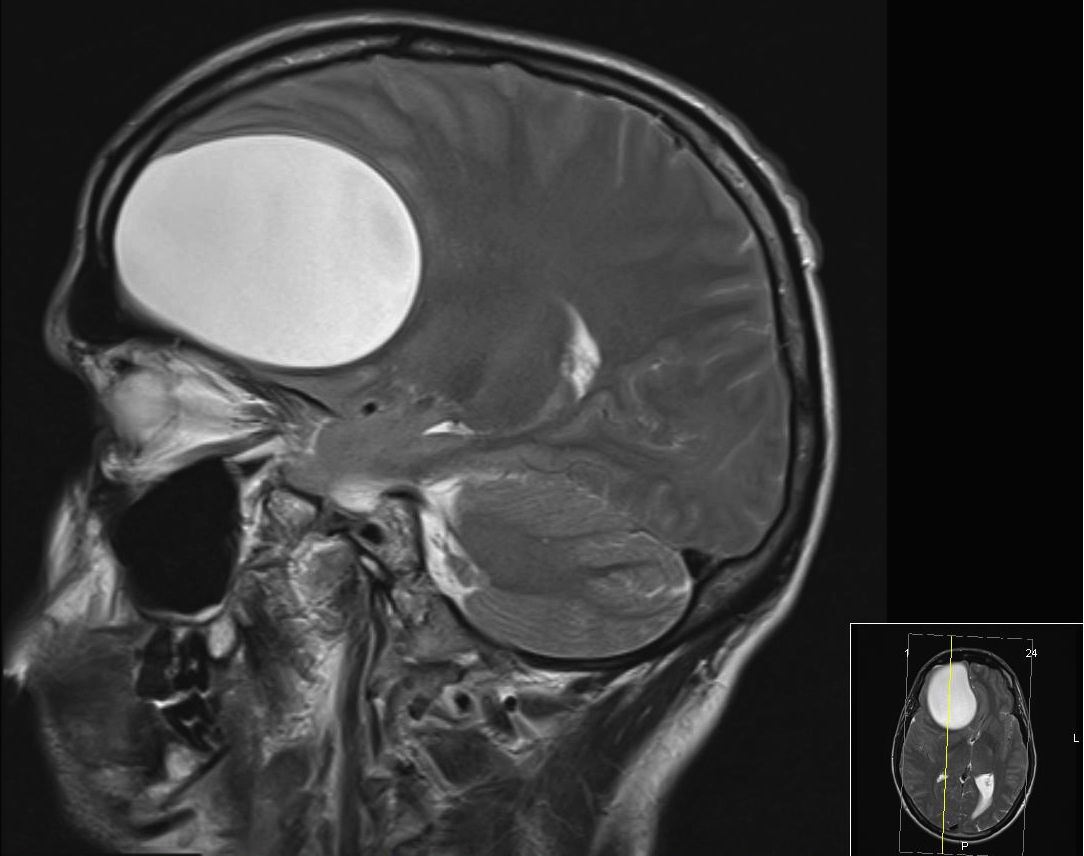
A brain MRI (Fig. 1) revealed a cystic lesion in the frontal lobe with 75×56×55mm exerting mass effect in the adjacent structures. The imaging features were suspicious for neuroglial cyst and he was submitted to frontal lobe pericystectomy. The postoperative period was unremarkable and the patient was discharged 3 days after. The pathological examination revealed a hydatid cyst with demonstration of protoscolices.
The patient was then observed by an infecciologist: he was asymptomatic and he denied risk factors for hydatid disease such as close or frequent contact with animals (namely dogs or cattle), previous travels to endemic regions or ingestion of possible contaminated water or food. Albendazol (400+200mg id) was administered from September to December 2014. Blood tests in October 2014 detected eosinophily but IgG serology for Echinococcus granulosus was negative. The clinical files from the hospital where he was previously submitted to pulmonary resection were reviewed and confirmed a past pulmonary hydatid cyst, but the patient was lost for follow-up in that institution.
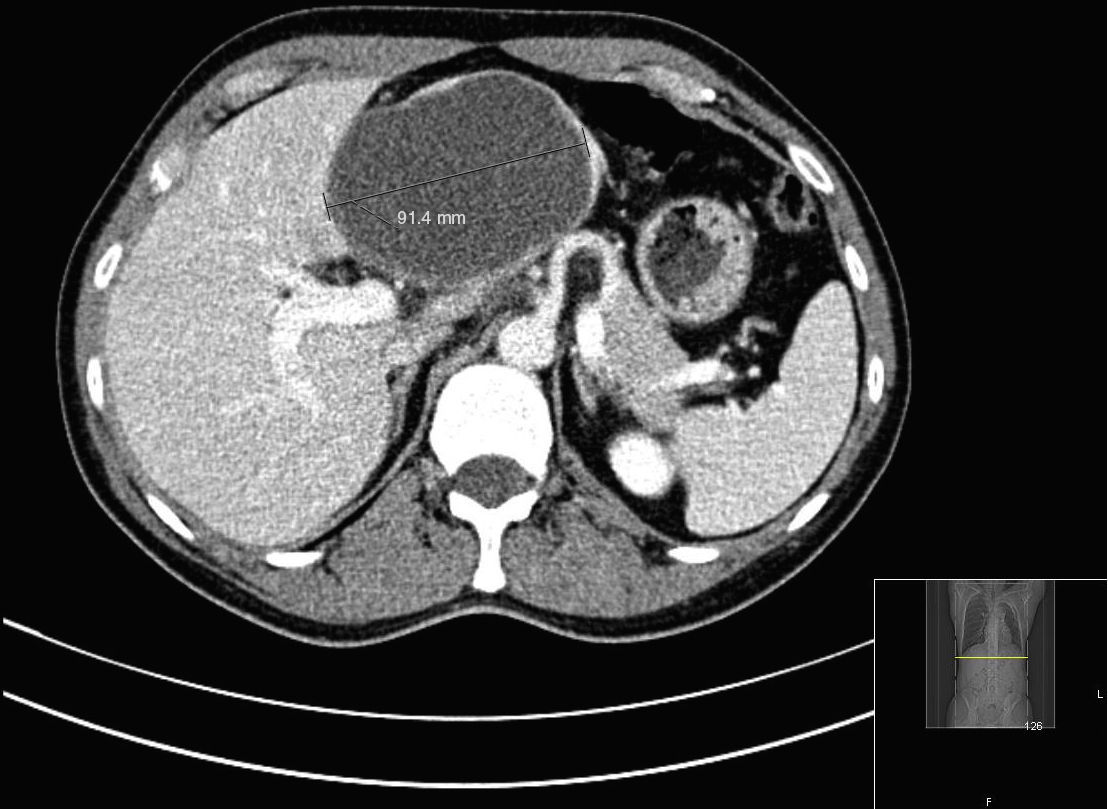
An abdominal ultrasonography in November 2014 revealed a 9cm hepatic cyst in the left lobe. A thoraco-abdominal CT scan (Fig. 2) was performed revealing a complex cyst with 9cm in the hepatic segment 3 suggestive of hydatid cyst. No other lesions were identified. After completing a month of albendazol, the patient was submitted to laparoscopic hepatectomy (bissegmentectomy 2,3) in May 2015. The postoperative period was unremarkable and the patient was discharged 6 days after surgery. The pathological examination confirmed hydatid cyst with observation of non-viable protoscolices.
One year after surgery he remains asymptomatic. Blood tests are normal and no other suspicious cysts were detected on sectional imaging.
In conclusion, hydatid disease is a rare but challenging condition that requires a multidisciplinary approach. Several medical and surgical treatments are often needed and a life-long follow-up is mandatory.
Conflicts of interestsThe authors declare no conflicts of interest.
Sources of fundingNone.