The growing demand for imaging tests and the progressive aging of the population have led to a progressive increase in the detection of indeterminate adrenal lesions. Once an adrenal incidentaloma is detected, clinical and hormone tests together with a battery of imaging techniques (CT, MRI, PET/CT…) make it possible to determine the cause in most cases. In this article, we discuss the advantages and limitations of each technique. We show the imaging characteristics of the most common adrenal lesions and propose a diagnostic algorithm to enable their diagnosis.
La creciente demanda de pruebas radiológicas y el envejecimiento progresivo de la población ha llevado al aumento progresivo en la detección de lesiones suprarrenales indeterminadas. Una vez detectado el incidentaloma suprarrenal, disponemos actualmente de pruebas clínicas y hormonales y de una batería de técnicas de imagen (TC, RM, PET/TC…) que hacen posible el diagnóstico etiológico de la mayoría de estos incidentalomas. En este artículo presentamos las ventajas y limitaciones de cada técnica, las características por imagen de las lesiones suprarrenales más frecuentes y proponemos un algoritmo diagnóstico que permita el diagnóstico de las mismas.
Adrenal incidentalomas are clinically silent adrenal masses that are discovered during the study, treatment or follow-up of unrelated clinical conditions. This definition excludes patients imaged for cancer staging or follow-up.1,2
In autopsy studies, the mean prevalence of adrenal incidentalomas is approximately 2.3%, with no significant differences between men and women, and higher rates in older patients.3 In the current setting of increasing demand and use of high-resolution diagnostic imaging techniques, there has been a significant increase in the detection of these lesions. Adrenal lesions are found in 4–5% of computed tomography (CT) studies performed for unrelated reasons.3–7
Seventy per cent of all adrenal incidentalomas are non-functioning adenomas; 5–16% are functioning adenomas; 6% are pheochromocytomas; 5% are adrenocortical carcinomas; 2% are metastatic carcinomas, and the rest, other types of lesions (myelolipomas, hematomas, cysts or lymphoma).3,8,9
When an adrenal incidentaloma is discovered during an imaging examination, the major issues are whether the lesion is hormonally functional and whether the lesion is likely to be benign or malignant. The results from these tests will determine whether lesion resection or conservative management is indicated.
Although the majority of adrenal incidentalomas are non-functioning, a fair number of these patients present with a subclinical form of hormonal dysfunction and may represent a population at higher risk of metabolic disorders and cardiovascular disease. For this reason, when an incidentaloma is found, a complete medical history and physical examination, a hormonal evaluation and, in some cases, additional radiologic studies are required. Screening for pheochromocytoma, primary hypercortisolism and hyperaldosteronism is routinely recommended for hypertensive patients, unless there are unequivocal features of myelolipoma, hemorrhage or adrenal cyst.1,10,11
Radiologists have at their disposal a variety of imaging techniques for characterizing adrenal incidentalomas, from CT and magnetic resonance (MR), which allow for the diagnosis of most adrenal lesions, to more sophisticated techniques such as positron emission tomography/computed tomography (PET/CT) and MR-spectroscopy, the latter still at an experimental stage. However, a small proportion of adrenal lesions remain undetermined and often represent a major diagnostic and therapeutic challenge given that there is no consensus in the literature as to when fine needle aspiration (FNA), surgery or follow-up (clinical, biochemical, and radiologic) is indicated.
This article examines the advantages and limitations of the different imaging techniques used in the characterization of incidentalomas and proposes a diagnostic algorithm that includes clinical, biochemical and, especially, imaging parameters.Although the definition of incidentaloma excludes patients undergoing imaging procedures as a part of staging or follow-up for cancer,1,2 we have included information on the diagnosis and management of adrenal lesions in oncologic patients, given that 50% of adrenal lesions in these patients are metastatic.12 Additionally, the characterization of these lesions is important for noninvasive tumor staging and for formulating a therapeutic plan and predicting the prognosis.8
Imaging techniquesComputed tomographyAt CT, parameters such as a size larger than 6cm, rapid growth, irregular or nodular margins and heterogeneity may be suggestive of a malignant adrenal incidentaloma, although these features are not very specific.13,14 However, the unenhanced CT attenuation measurements, the histogram analysis and the values of contrast-enhancement washout allow for adrenal lesion characterization in a high percentage of cases.6,15,16
The appropriate technique for the evaluation of adrenal nodules involves a study without intravenous (IV) contrast (baseline) in all patients, followed if necessary by a contrast-enhanced CT (portal phase at 60s and delayed phase at 15min). A thin slice thickness (2–3mm) is required, as well as attenuation measurements obtained through regions of interest covering a significant portion of the lesion (1/2 to 2/3 of the lesion area), but avoiding the peripheral edges of the mass to prevent partial volume artifacts.14,17
The quantification of the mean attenuation values on unenhanced (baseline) CT is a simple and highly sensitive task to detect fat within the tumor, which makes it the most useful parameter in the initial assessment of adrenal lesions.18,19
Other tool that may be useful in the characterization of adrenal lesions is the histogram analysis, that is, a graphical representation that displays the individual analysis of the attenuation values for each pixel in a given area. This method is highly sensitive for the detection of fat, represented as pixels with negative attenuation values.8,17,20,21
The most commonly used parameters in contrast-enhanced CT are:
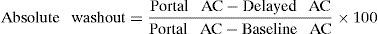
Absolute washout: quantifies the delayed washout compared to portal-phase enhancement.
where AC is the attenuation coefficient (HU).Relative washout: is an estimated calculation of the absolute washout when an adrenal lesion is discovered on enhanced CT (portal and delayed phase) and no previous baseline study is available.
Washout values are of little use in the characterization of adrenal masses with heterogeneous areas of low attenuation (necrosis or cystic areas).
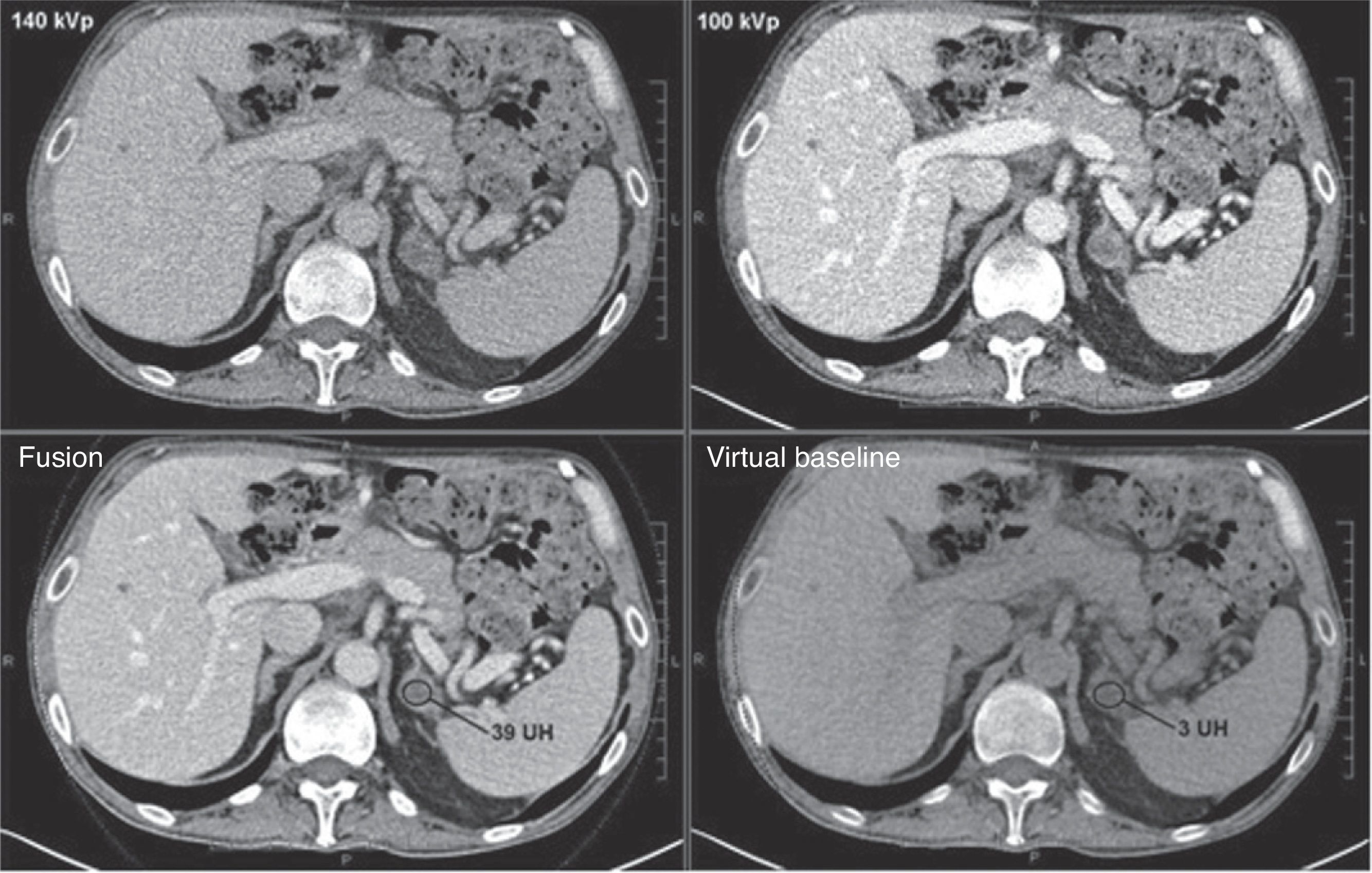
The recent emergence of dual energy CT allows us to subtract, using a postprocessing algorithm, the iodine contrast agent from the abdominal images obtained after contrast administration and generate a virtual unenhanced study that can be used to estimate the baseline attenuation values of an adrenal lesion.22
Magnetic resonanceChemical shift imaging is the mainstay of MR evaluation of solid adrenal lesions and is based on the detection of cytoplasmic lipid using in-phase and opposed-phase gradient-echo T1-weighted Images.23–26 This method relies on the differences in resonance frequency of lipid and water molecules. On opposed-phase images, the phase of the lipid signal is opposite to that of the water, resulting in a drop of signal in those voxels containing both elements, which microscopically correlates with the presence of intracellular lipid.27
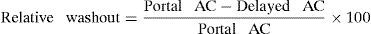
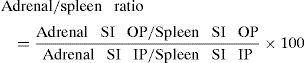
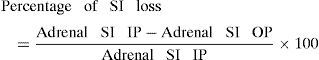
The chemical shift phenomenon can be assessed either qualitatively, by visual comparison of the adrenal lesion intensity with that of the spleen, or quantitatively, through one of the following formulas28,29:
where SI is the signal intensity; IP the in-phase; and OP the opposed-phase.Additionally, the protocols may include T1-, T2- and fat-suppressed T1-weighted sequences obtained before and after contrast administration, providing data on the morphology and behavior of the adrenal lesions comparable to those provided by CT.
Gadolinium-enhanced dynamic MR imaging involves the IV administration of gadolinium contrast media and the acquisition of consecutive fast sequences at variable time intervals, depending on the protocol of each institution, in order to obtain a curve representing the absolute or relative variation in signal within a specific time frame.30,31
MR-spectroscopy has proved potentially useful in the differential diagnosis of adrenal lesions based on metabolite ratios, and has proved particularly useful in the characterization of pheochromocytomas32 and in the differentiation of adenomas and pheochromocytomas from carcinomas and metastases.33,34
Thus far, diffusion MR imaging has not proved useful to differentiate benign from malignant lesions.31
UltrasonographyUltrasonography does not allow for the characterization of most adrenal incidentalomas. It has been recently reported that the use of contrast-enhanced ultrasonography may improve the diagnostic accuracy since malignant lesions are usually hypervascular. This would translate into early contrast enhancement in the arterial phase and rapid washout.35
Nonetheless, its systematic use is limited by the difficult visualization of the adrenal glands with this technique.
Positron emission tomography/computed tomography18F-fluorodeoxyglucose PET/CT (18F-FDG PET/CT) protocols vary among institutions. This technique is highly sensitive for differentiating benign from malignant lesions,28,36 being particularly useful in the identification of metastatic adrenal masses in the workup of oncologic patients.37
The metabolic activity can be evaluated by qualitative analysis, that is, visual comparison between the uptake of the adrenal lesion and that of the liver, or by quantitative analysis based on the determination of the mean and maximum SUVs (Standardized Uptake Values) and SURs (Standardized Uptake Ratios), obtained through the adrenal/liver ratio.
The usefulness of 11C-metomidate (MET) PET/CT imaging in the detection of non-necrotic primary adrenal tumors38 is being validated, as well as that of 11C-hydroxyephedrine and of 18F-dihydroxyphenylalanine in the detection of pheochromocytomas.8
MIBG (a radiotracer taken up by chromaffin cells) scintigraphy allows pheochromocytoma detection in a significant percentage of cases.28,36
Fine needle aspirationIn the algorithms for the management of adrenal incidentalomas, FNA is indicated for the characterization of actively growing lesions, in cases of equivocal radiologic findings depending on the clinical setting and of high suspicion of metastasis27 (in patients with a known primary cancer), and only if the definitive diagnosis changes the treatment approach.
FNA is particularly useful in the differentiation between adrenal and non-adrenal tissue (metastasis or infection). Nonetheless, FNA cytology has low or no diagnostic yield in the differentiation of adenomas from adrenal carcinomas. FNA can be performed under CT, MR or ultrasound guidance and its diagnostic accuracy varies from 83% to 93%, with a complication rate of approximately 3% (most commonly pain, hemorrhage and pneumothorax).39,40 Hormonal evaluation must be done before FNA is undertaken in order to rule out the possibility of pheochromocytoma, as the puncture may precipitate a hypertensive crisis.
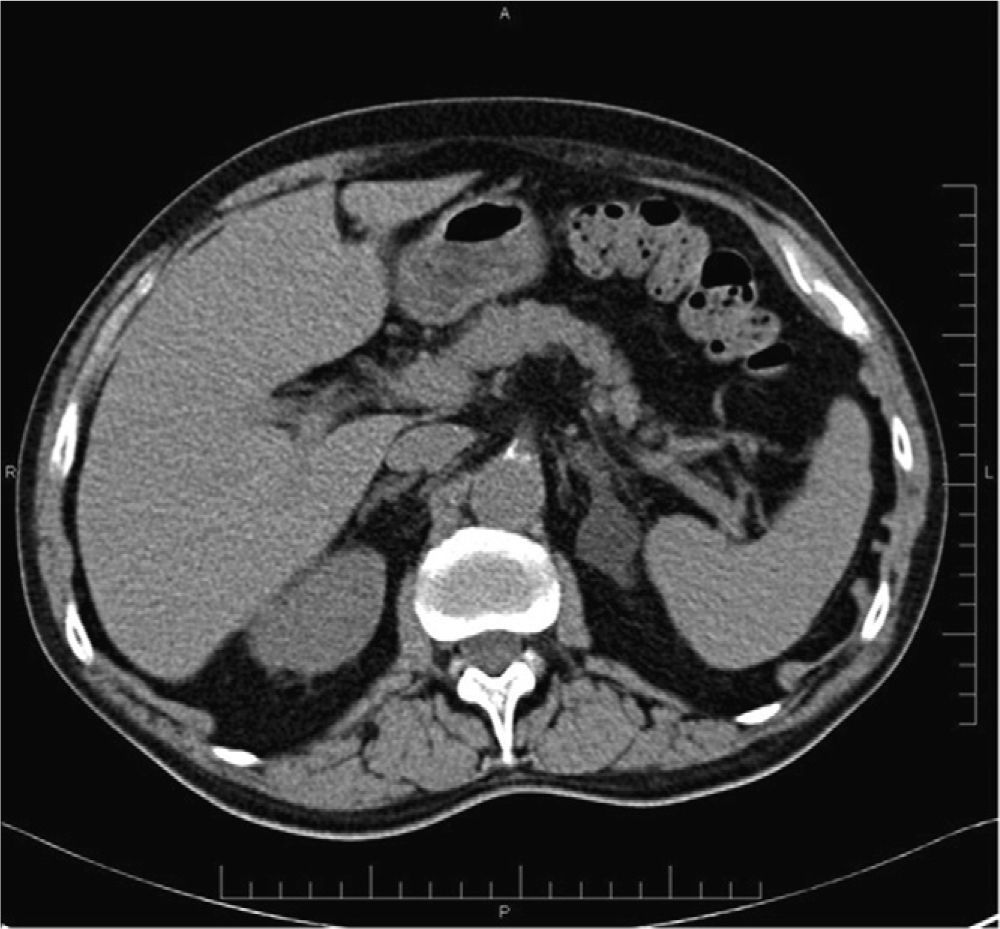
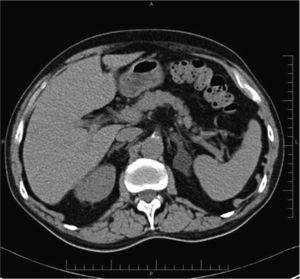
Most common adrenal incidentalomasAdenomasOne of the key points in the diagnosis of adenomas is the presence of a variable proportion of intracellular lipid, whose detection allows a highly accurate diagnosis. A maximum threshold of 10HU at unenhanced CT for adenoma characterization (Figs. 1 and 2) yields a sensitivity of 71% and a specificity of 98%. These parameters are close to 100% when size, growth and shape are also taken into account.16,18,19
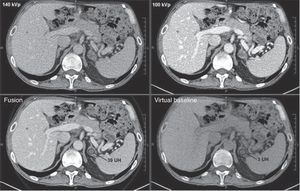
Adrenal adenoma. Abdominal dual energy CT scan in a 63-year-old patient with a history of colorectal carcinoma; no unenhanced study was performed. The portal-phase enhanced CT scan (fusion 140kVp+100kVp) shows a nodular lesion in the left adrenal gland of 39HU. With the dual energy technique, a virtual unenhanced study could be obtained and this showed that the attenuation of the lesion was 3HU, compatible with an adenoma.
Most adenomas, even lipid-poor adenomas, supposedly contain enough amounts of cytoplasmic lipid to allow for their characterization.20 Histogram analysis may be useful in the characterization of lipid-poor adenomas. At unenhanced CT, the histogram analysis with a cutoff of 10% negative pixels yields a specificity of 100% and a sensitivity of 46–91%.17,20,21,41 When using an unenhanced CT attenuation threshold of 10–20HU, the finding of more than 10% negative pixels yields a sensitivity of 92% for the diagnosis of adenoma. For unenhanced CT attenuation values of 20–30HU and >30HU, the sensitivity drops to 10% and 0%, respectively.21 The combination of values ≤10HU or >10% of negative pixels yields a sensitivity of up to 91% compared with 68% sensitivity when attenuation values are used alone, while the specificity remains at 100%.20
Therefore, the histogram analysis of unenhanced CT improves the overall sensitivity for the characterization of adenomas, particularly in lesions with attenuation values of 10–20HU on unenhanced CT.
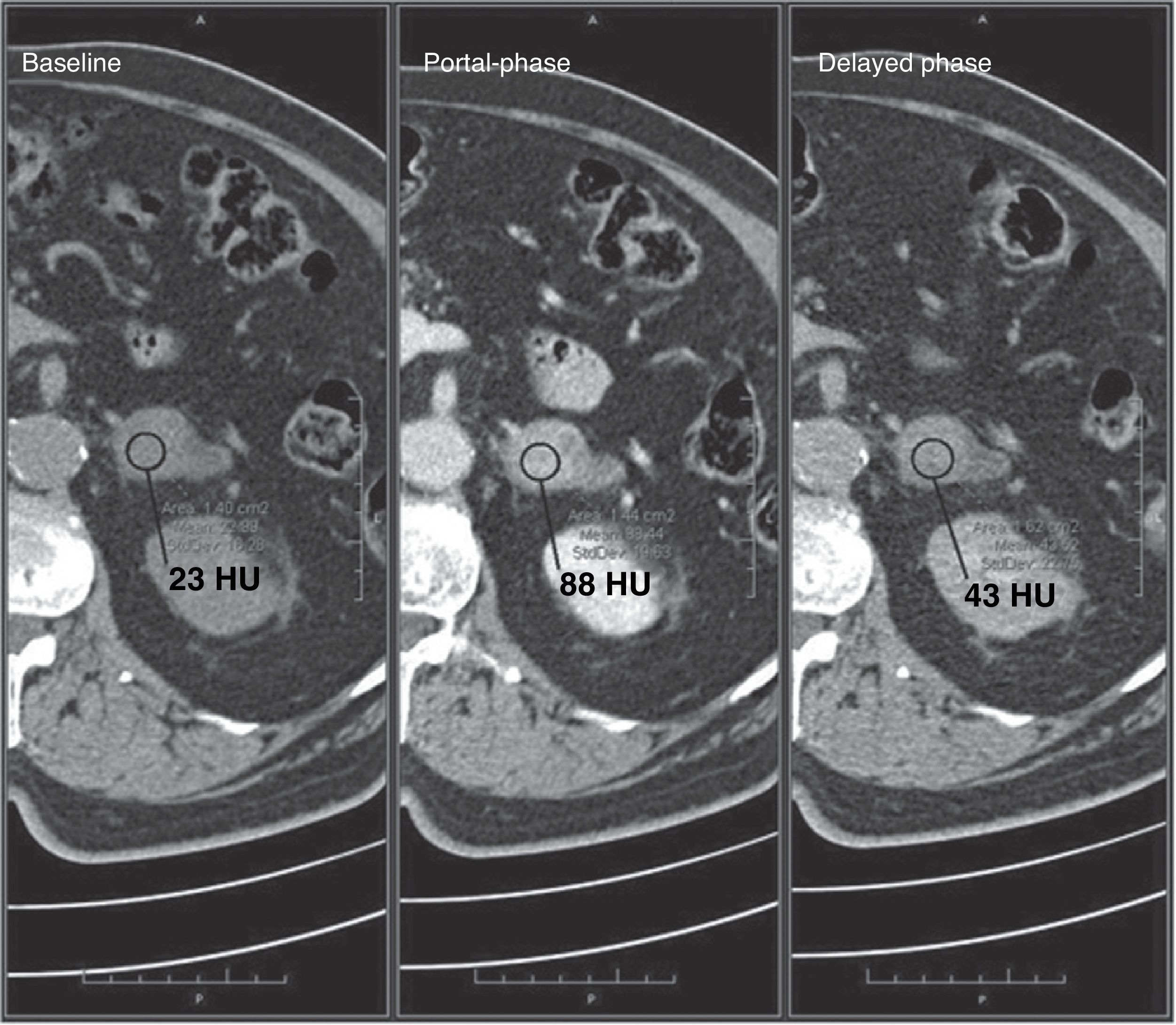
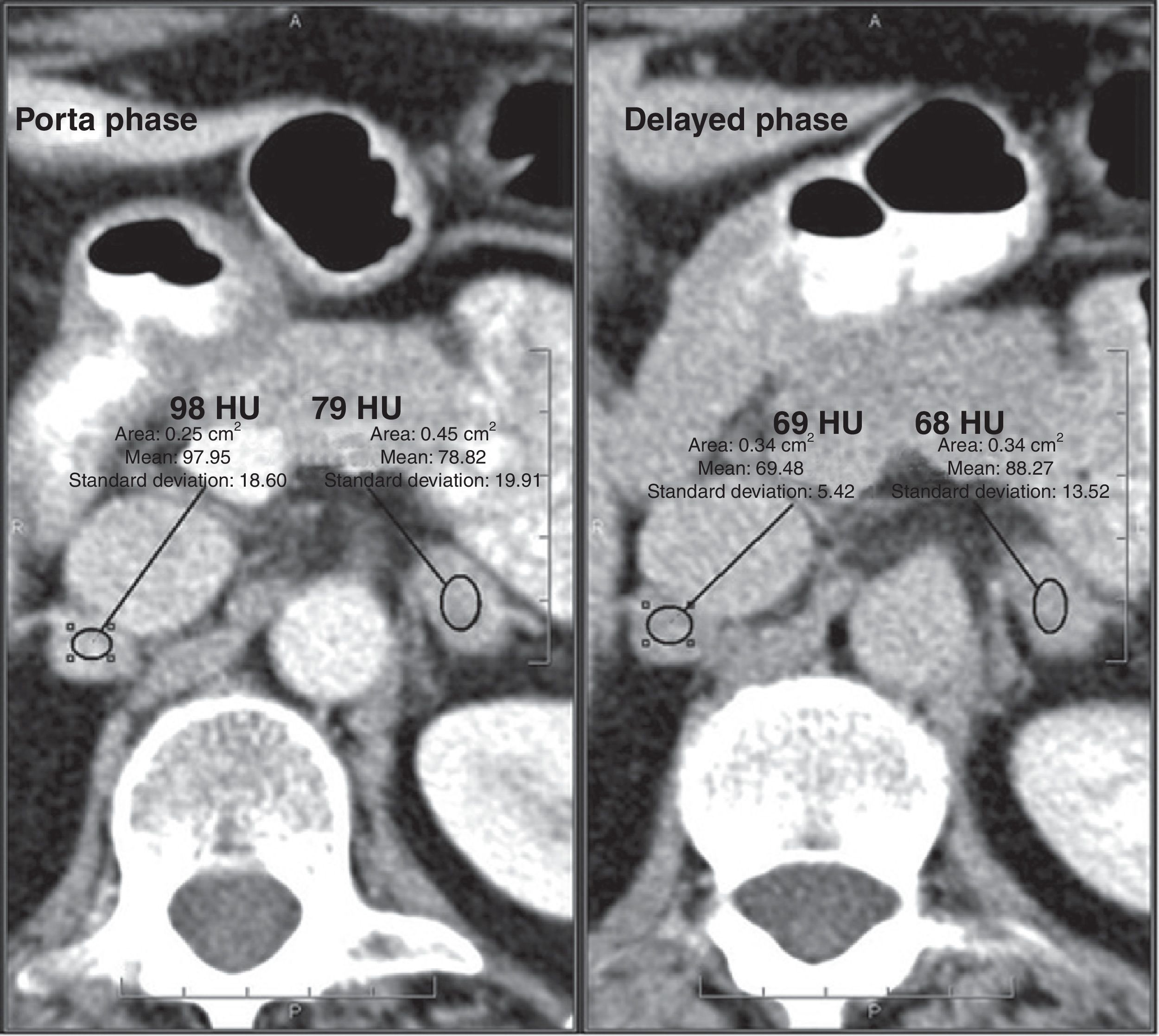
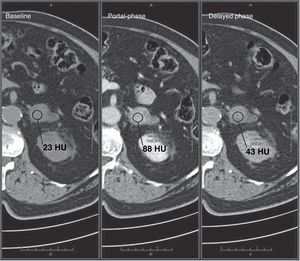
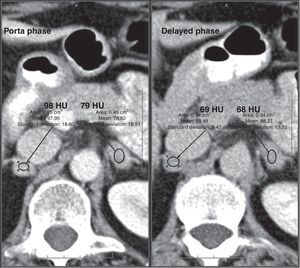
Approximately 70% of adenomas are lipid-rich42–44 and 30% are lipid-poor. Both types show a more rapid washout of contrast medium than malignant tumors, therefore the calculation of the washout may be useful.6,15,16,42,43,45,46 Absolute washout ≥60% (88% sensitivity and 96% specificity) or relative washout ≥40% (96% sensitivity and 100% specificity) are suggestive of adenoma16,42,43,45–47 (Figs. 3 and 4). It should be noted that these values are set for delayed images obtained 15min after contrast administration. Park et al.48 analyzed the relative washout values of adrenal lesions at 3min after contrast administration and reported that values >25% were diagnostic for adenoma, and values ≤5% were compatible with non-adenomatous lesions. Lesions with values between 5% and 25% were considered unspecific. However, the study had some methodological limitations and further research is thus required to validate these results.
Adrenal adenoma. A 56-year-old patient investigated for a left renal mass. Intravenous contrast-enhanced abdominal CT scans, portal phase at 60s and delayed phase at 15min, show a nodular lesion in the left adrenal gland. No unenhanced scan is available and, therefore, the absolute washout cannot be estimated. Nonetheless, the relative washout of 96% is suggestive of adenoma.
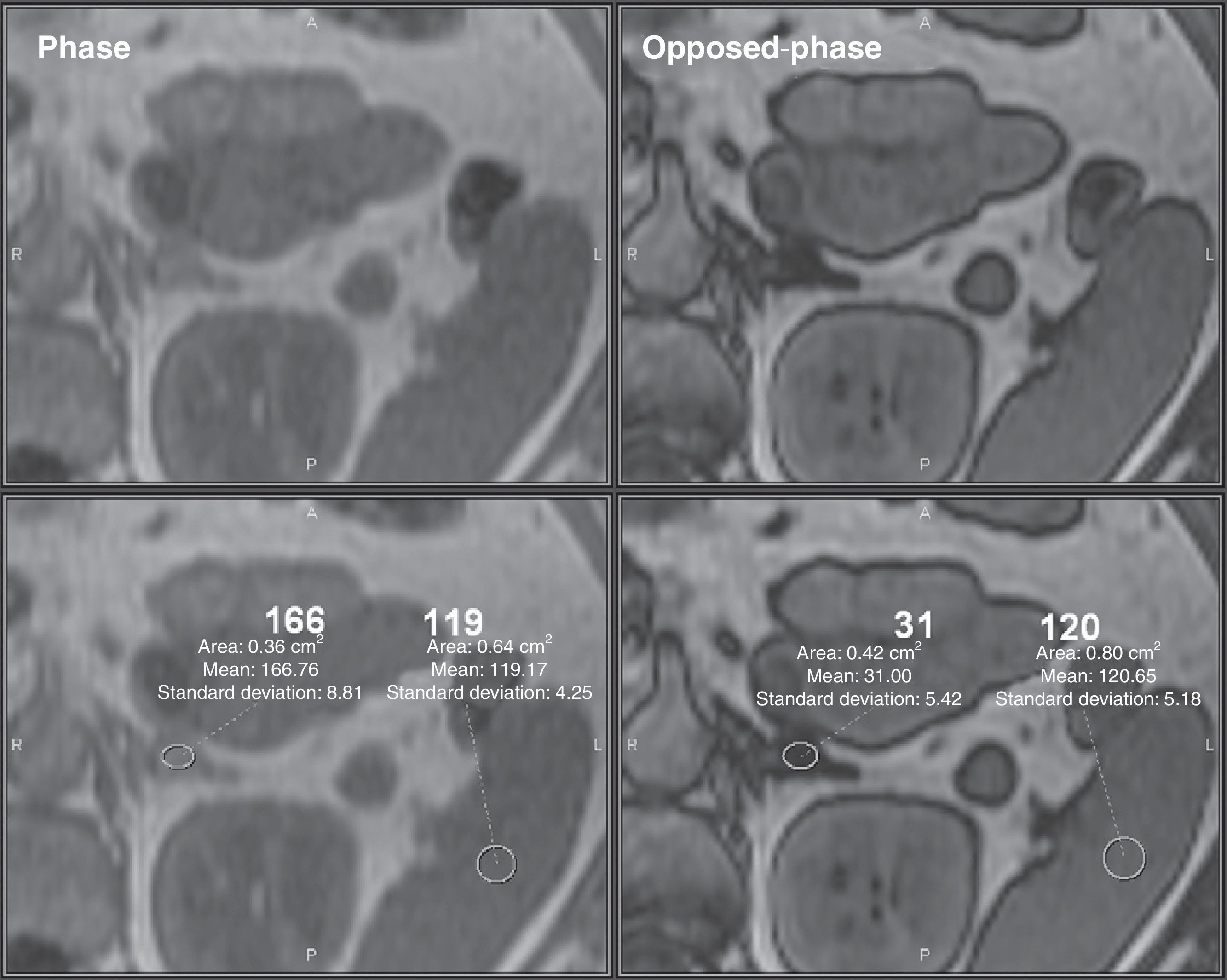
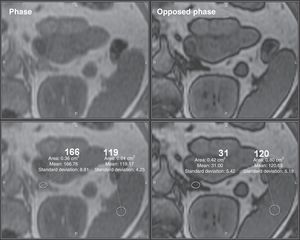
At MRI, on gradient-echo in- and opposed-phase sequences, the signal loss on opposed phase (known as chemical shift) is indicative of cytoplasmic lipid content,24–26 which yields a sensitivity of 81–100% and a specificity of 94–100% for the characterization of adenomas.24,26,49 In quantitative terms, an adrenal/spleen ratio ≤70%50,51 or a signal intensity loss >16.5 is compatible with adenoma.52 However, visual analysis of chemical shift imaging compared with splenic intensity is an easier method of adrenal lesion analysis and has been reported to be comparable to quantitative assessments28,29 (Fig. 5).
Adrenal adenoma. Abdominal MRI in a 52-year-old patient investigated for an incidentally discovered adrenal nodule on CT in the left adrenal gland. Opposed-phase gradient echo sequence shows a significant signal loss of the nodule in comparison with the in-phase sequence, which is highly suggestive of adrenal adenoma.
Chemical shift imaging is not effective in adenomas with unenhanced CT attenuation >30HU and is as effective as unenhanced CT in adenomas ≤10HU.23,25,50,52 Although the sensitivity for adenomas with attenuation 10–30HU is lower than the calculation of contrast washout on CT, chemical shift imaging is indicated for these attenuation values because it yields a higher sensitivity than unenhanced CT and avoids the radiation associated with the three contrast-enhanced CT sequences.
After administration of gadolinium contrast media, adenomas show mild enhancement and rapid washout, while malignant lesions and pheochromocytomas show marked enhancement with slower washout.53 There is no consensus on the usefulness of the quantitative assessment of contrast enhancement curves30,53; nonetheless, significant differences in the time-to-peak have been described between adenomas and malignant lesions.31
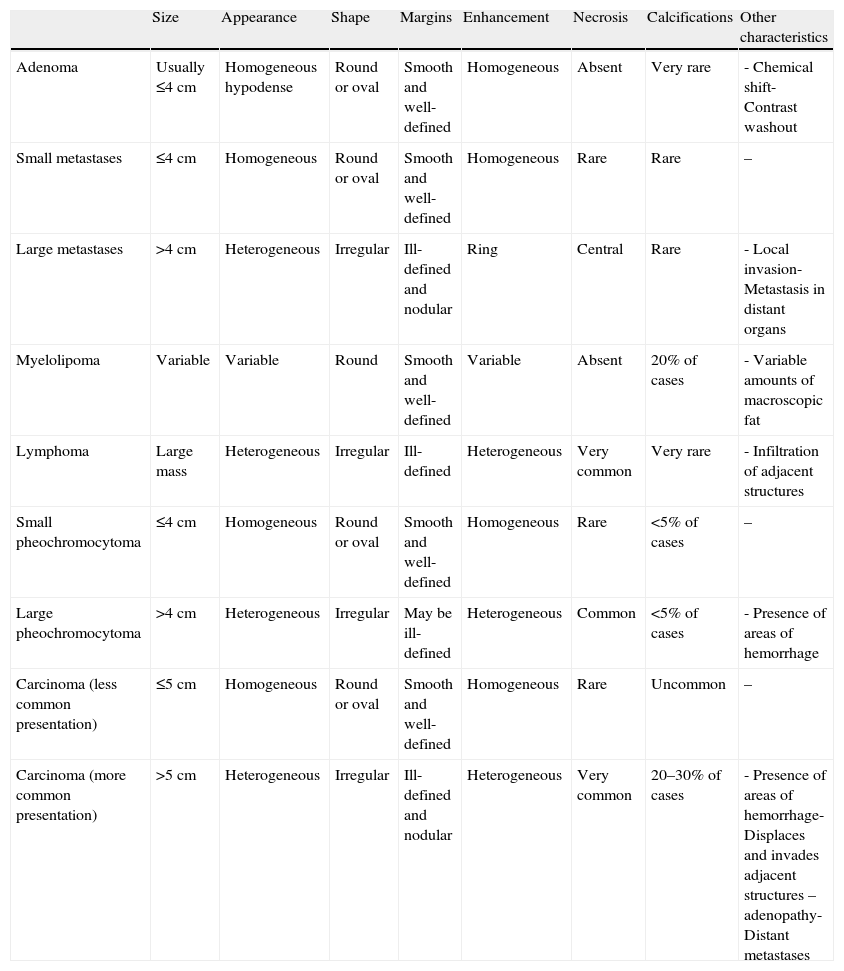
MetastasisLarge adrenal metastases are usually accompanied by data suggestive of malignancy on CT and MR imaging (Table 1), while the appearance of small lesions makes them frequently indistinguishable from adenomas.6,13,15
Imaging findings of the most common adrenal lesions.
| Size | Appearance | Shape | Margins | Enhancement | Necrosis | Calcifications | Other characteristics | |
| Adenoma | Usually ≤4cm | Homogeneous hypodense | Round or oval | Smooth and well-defined | Homogeneous | Absent | Very rare | - Chemical shift- Contrast washout |
| Small metastases | ≤4cm | Homogeneous | Round or oval | Smooth and well-defined | Homogeneous | Rare | Rare | – |
| Large metastases | >4cm | Heterogeneous | Irregular | Ill-defined and nodular | Ring | Central | Rare | - Local invasion- Metastasis in distant organs |
| Myelolipoma | Variable | Variable | Round | Smooth and well-defined | Variable | Absent | 20% of cases | - Variable amounts of macroscopic fat |
| Lymphoma | Large mass | Heterogeneous | Irregular | Ill-defined | Heterogeneous | Very common | Very rare | - Infiltration of adjacent structures |
| Small pheochromocytoma | ≤4cm | Homogeneous | Round or oval | Smooth and well-defined | Homogeneous | Rare | <5% of cases | – |
| Large pheochromocytoma | >4cm | Heterogeneous | Irregular | May be ill-defined | Heterogeneous | Common | <5% of cases | - Presence of areas of hemorrhage |
| Carcinoma (less common presentation) | ≤5cm | Homogeneous | Round or oval | Smooth and well-defined | Homogeneous | Rare | Uncommon | – |
| Carcinoma (more common presentation) | >5cm | Heterogeneous | Irregular | Ill-defined and nodular | Heterogeneous | Very common | 20–30% of cases | - Presence of areas of hemorrhage- Displaces and invades adjacent structures – adenopathy- Distant metastases |
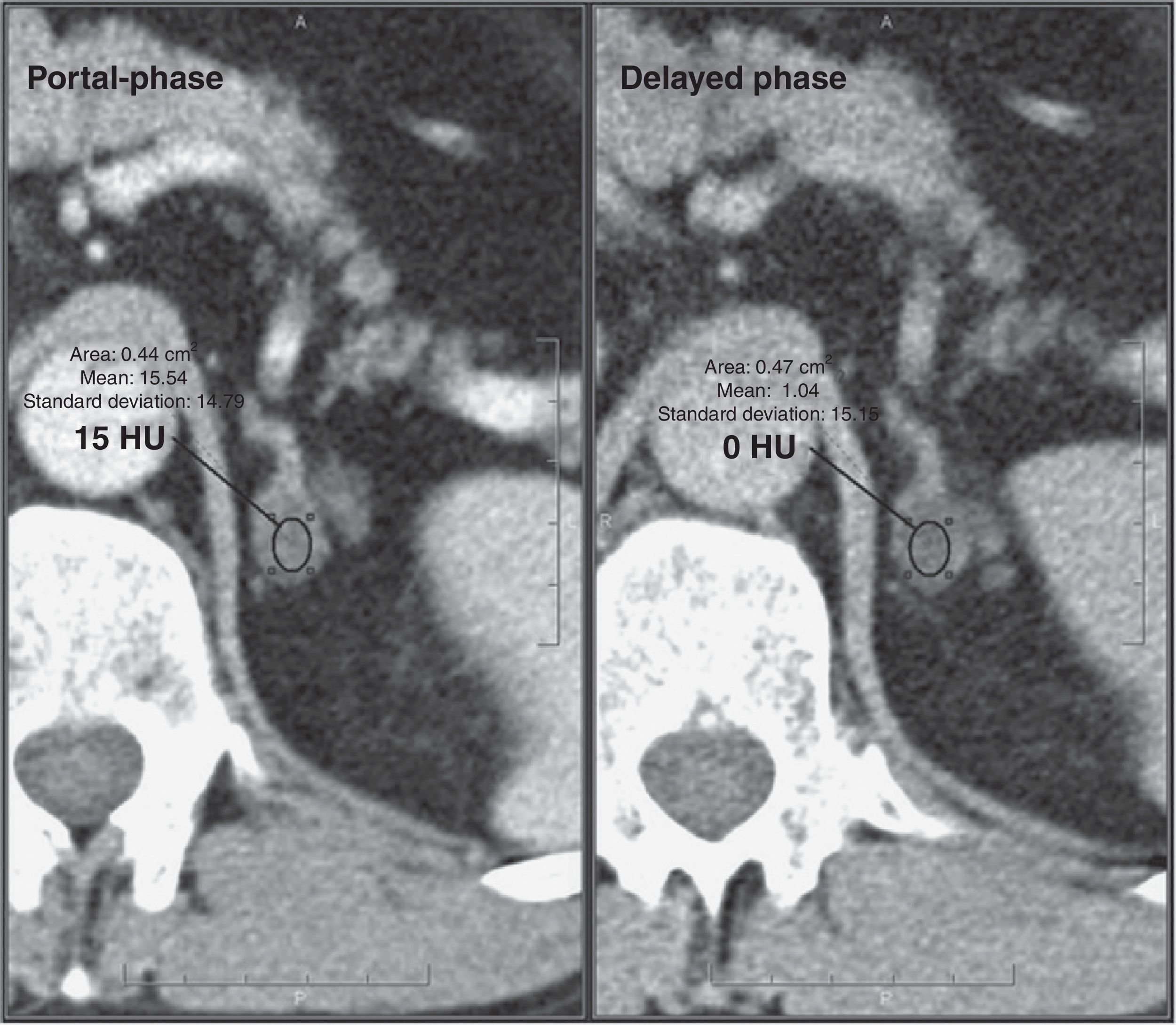
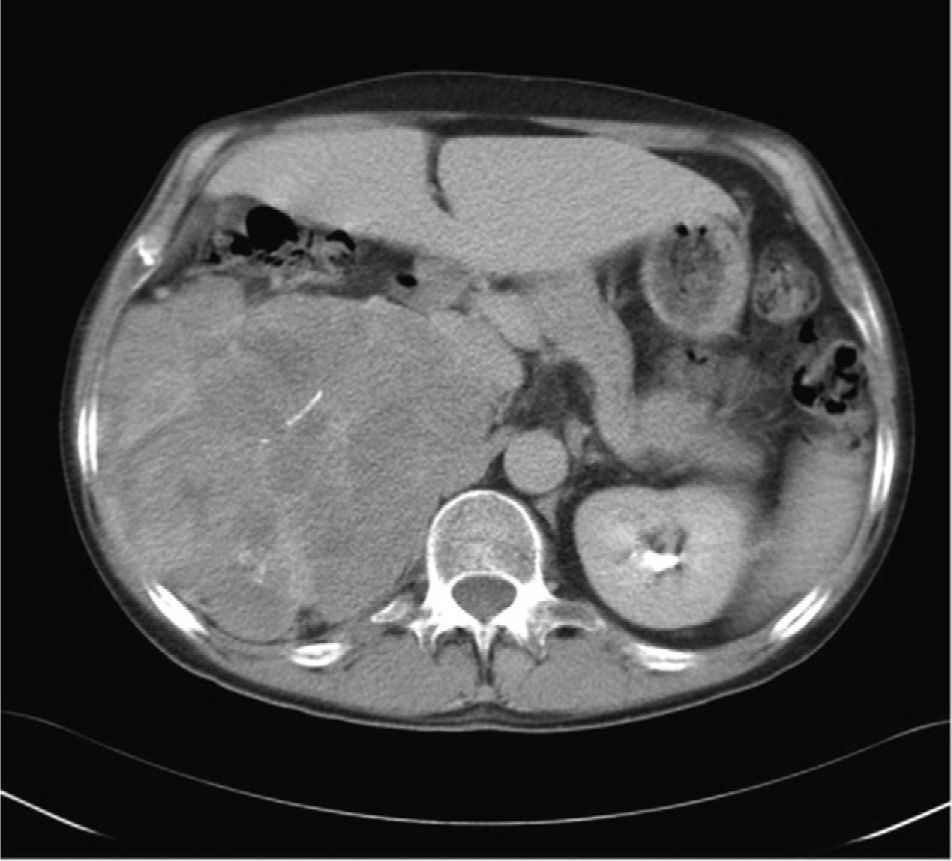
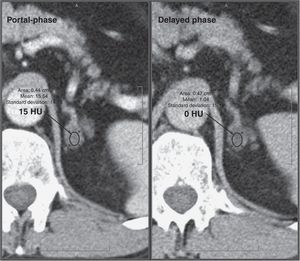
Metastases show low values of absolute washout (<0.6%) and relative washout (<0.4%) on dynamic contrast-enhanced CT studies (Fig. 6), and no signal loss on opposed-phase sequences in chemical shift MR imaging, but these are considered non-specific findings.
Adrenal metastasis. IV contrast-enhanced CT scan, portal phase at 60s and delayed phase at 15min, in a patient with a history of breast cancer shows round/oval homogeneous nodules with smooth, well-defined margins in both adrenal glands. The lesions show unspecific relative washout of 28% (right) and 12% (left). CT follow-up at 4 months demonstrated enlargement of the lesions, which confirmed the diagnosis of metastasis.
A recent meta-analysis37 has demonstrated that 18F-FDG PET/CT has a sensitivity and specificity of 97% and 91%, respectively, for differentiating between benign and malignant lesions, and that the qualitative analysis (visual comparison between adrenal and splenic uptake) is more accurate than quantitative analyses. The study suggests that PET/CT provides high diagnostic accuracy in lesions >1cm for distinguishing benign from malignant adrenal disease, particularly in the setting of oncologic patients, making the use of additional imaging studies unnecessary in this subgroup of patients.
However, PET/CT is not without limitations: false positive results have been reported in 9%37 of benign lesions,54,55 and 3% of false negative findings37 may be seen in adrenal metastatic lesions with hemorrhage or necrosis, small-sized (<10mm) lesions or hypometabolic tumors (bronchioloalveolar carcinoma or carcinoid tumors).54 Additionally, PET/CT is a costly technique with limited availability.28,54
MET PET/CT, still not in widespread use, can differentiate adrenal lesions (adenomas, carcinomas) from non-adrenal lesions (adrenal metastases, pheochromocytomas, lymphomas) with a sensitivity of 89% and specificity of 96%.38
Growth of an adrenal lesion over a period of less than 3–6 months or the presence of new lesions is suggestive of malignancy.
When dealing with an incidentaloma in a patient that presents without an identifiable primary tumor and non-conclusive imaging findings, FNA is rarely indicated given the low frequency of metastases, the risk of complications and the significant rate of false negative results. Surgical treatment or CT follow-up are thus recommended based on the characteristics of the mass and other clinical characteristics (patient's age, comorbidity).1,10,28,56 If the mass enlarges during the follow-up period, FNA can be performed before surgical planning.27
The primary indication for FNA is a known primary tumor and high suspicion of metastasis, provided that the definitive diagnosis changes the therapeutic approach.27
MyelolipomaMyelolipomas are tumors composed of varying amounts of mature adipose tissue and hematopoietic cells.
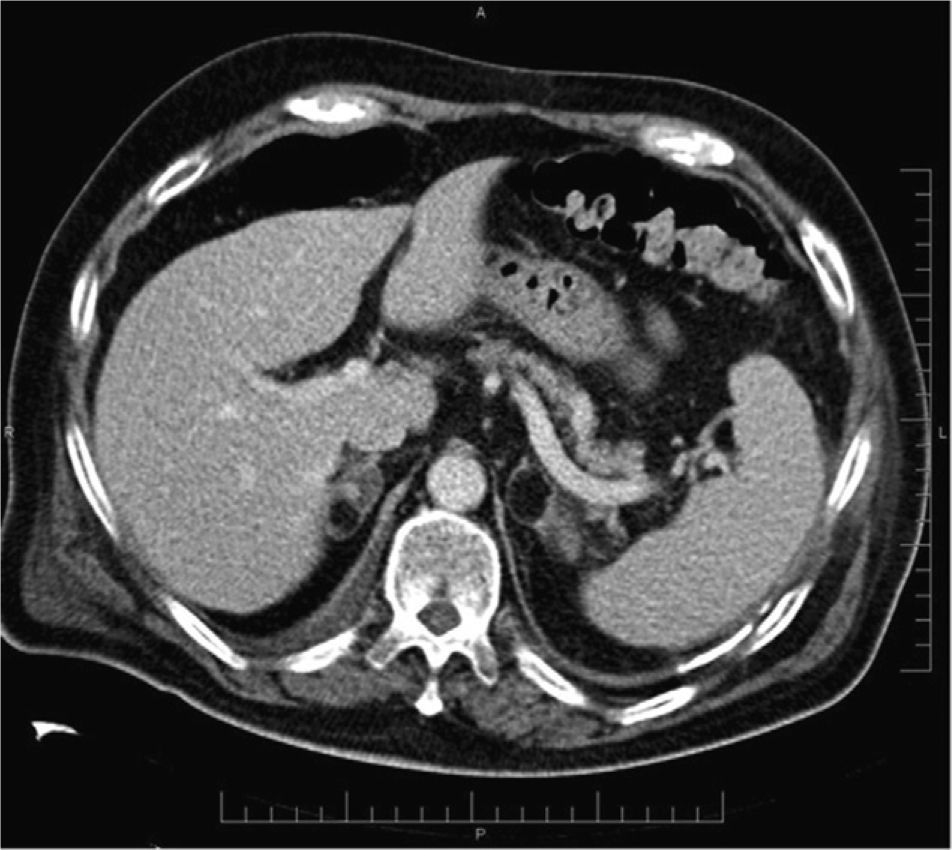
The key CT finding is the identification of macroscopic fat (<−20HU), a characteristic finding that makes unnecessary the use of additional techniques6,57,58 (Fig. 7).
FNA is rarely indicated and it is only used in doubtful cases for the characterization of malignant fatty tumors, especially liposarcomas.
The malignant transformation of myelolipomas has not been reported, and therefore follow-up or surgical treatment is not required. However, large myelolipomas (>10cm) are usually removed because of the risk of hemorrhage.57
LymphomaPrimary adrenal lymphoma is extremely uncommon, with only about 100 cases reported in the literature.59 Early diagnosis and intervention might dramatically affect patients’ survival.60
Most adrenal lymphomas are bilateral and adrenal insufficiency occurs in 50% of cases.
CT and MRI findings (Table 1) are not sufficiently specific to establish a correct diagnosis. Primary adrenal lymphoma shows increased 18F-FDG uptake on PET/CT, characteristic of malignancy.60 Given the low number of cases reported, there is no consensus on the preferred method for establishing a definitive diagnosis (surgery versus FNA).
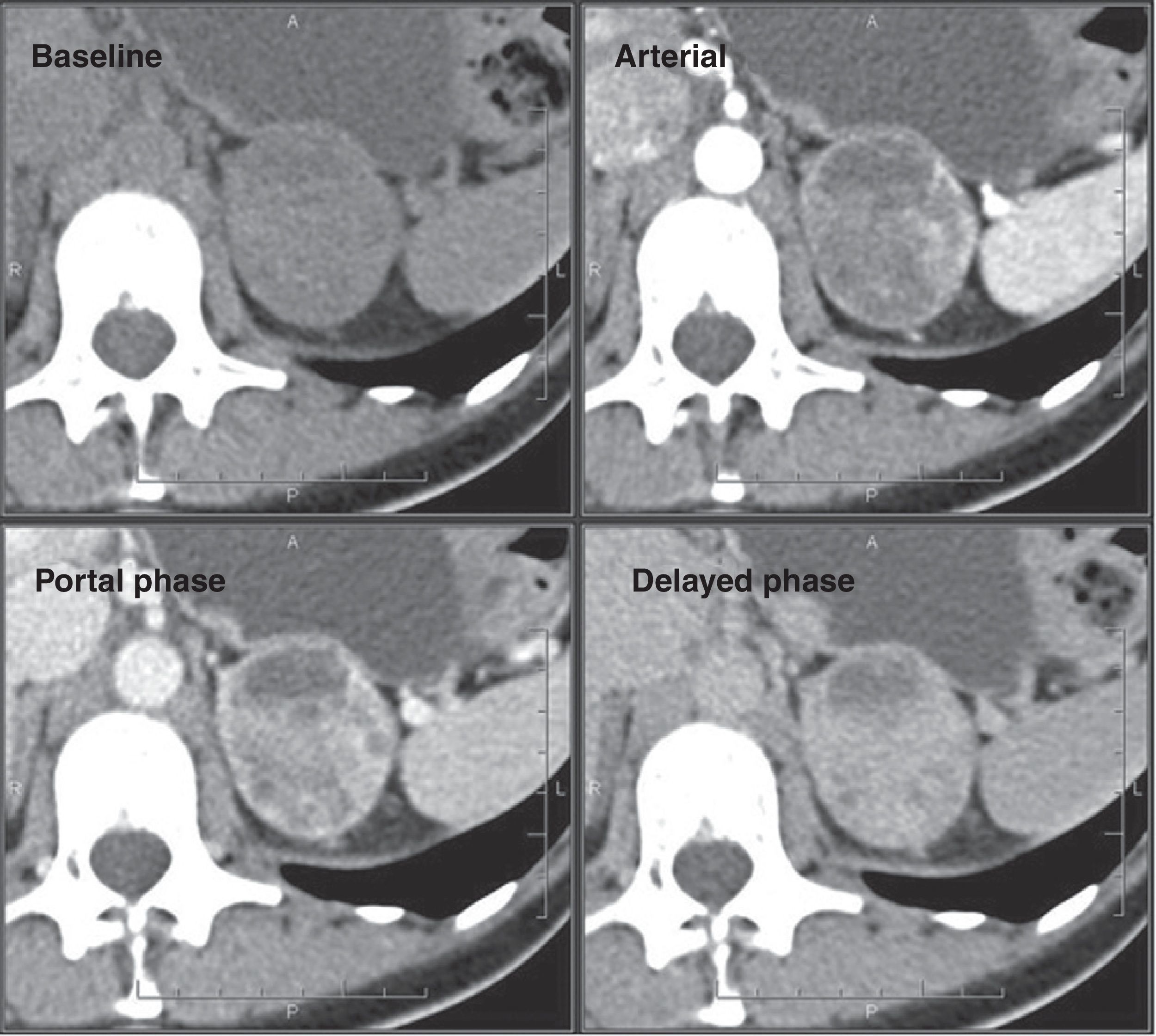
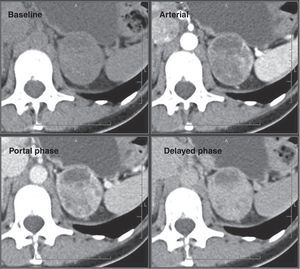
PheochromocytomaOn CT, small-sized pheochromocytomas appear as homogeneous, oval and well-defined masses.6,61 Larger lesions (>4–5cm) have a higher probability of containing areas of necrosis or hemorrhage, reflecting the hypervascularity of these tumors62 with heterogeneous enhancement that makes them indistinguishable from other adrenal neoplasms; biochemical correlation is thus required for diagnosis (Fig. 8).
Most pheochromocytomas do not contain lipid; however, a small fraction of cases may contain sufficient intracellular lipid to have attenuation values <10HU, making them indistinguishable from adenomas.44,62–64 Absolute and relative contrast washout are <60% and <40%, respectively, in 84–89% of cases,43,45,64,65 and pheochromocytomas have attenuation coefficients on portal-phase CT usually higher than those of adenomas (up to 110–120HU), but there is overlap.45
Traditionally, the administration of iodinated contrast material to a patient with pheochromocytoma has been reported to precipitate a hypertensive crisis, if alpha-receptor blockade has not been instituted.66 However, Mukherjee67 suggests that non-ionic iodinate contrast agents with low osmolality are safe in these patients, even without alpha blockade. Current clinical practice would generally avoid the use of iodinated contrast material in a patient with suspected pheochromocytoma.62
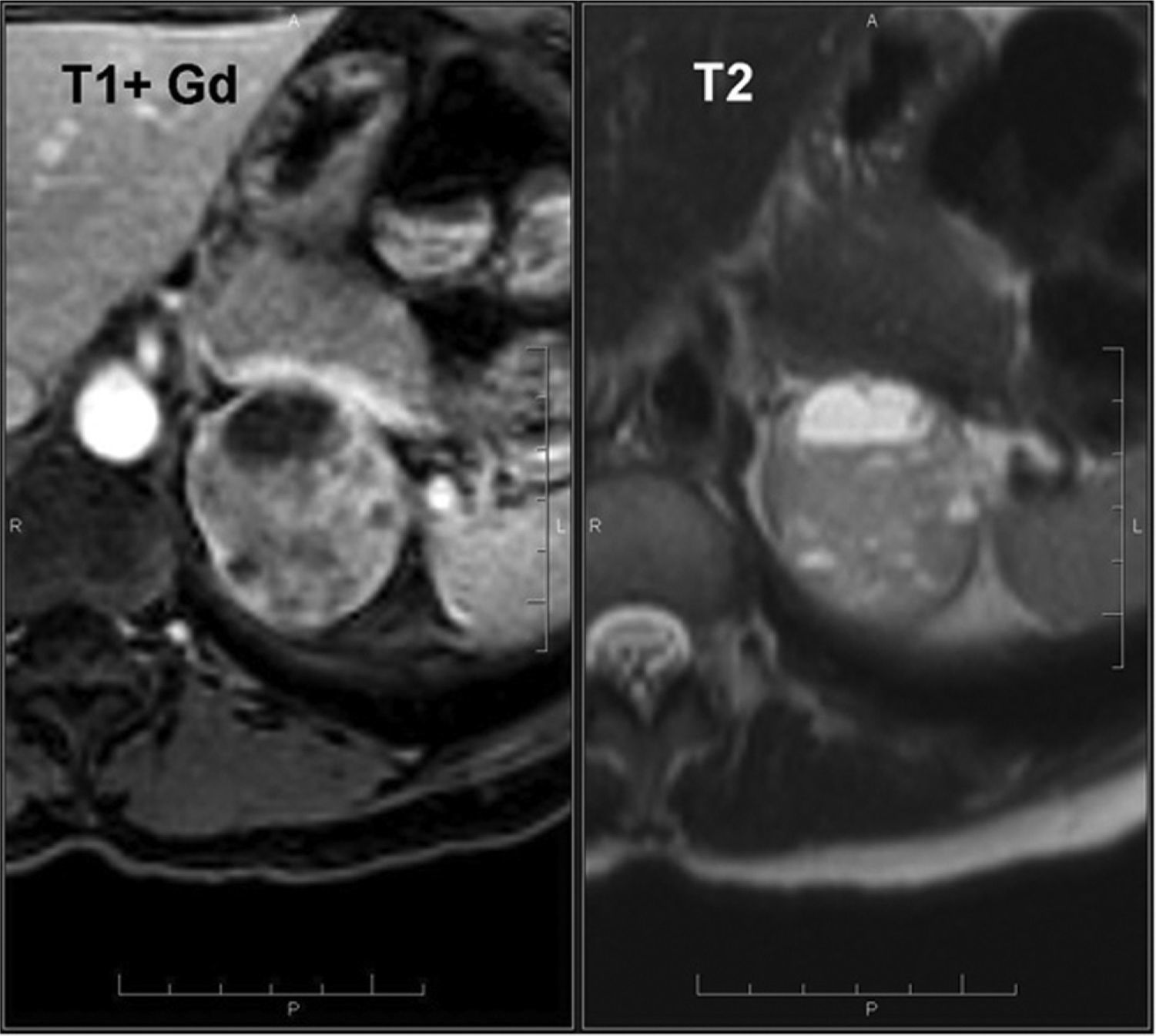
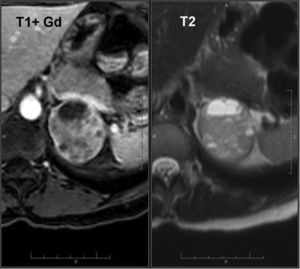
T2-weighted imaging is more specific than CT for the diagnosis of pheochromocytoma62 because of the hyperintensity secondary to the cystic component.68,69 Pheochromocytomas do not lose signal on opposed-phase T1-weighted sequences,44,62–64 with the exception of the few cases that contain microscopic fat. Intense and persistent enhancement appears after IV administration of gadolinium70 (Fig. 9).
Pheochromocytoma (same patient as Fig. 8). MRI with intravenous contrast material shows a heterogeneous mass with hypersignal areas on T2-weighted images, and heterogeneous areas of hyperintensity on arterial-phase T1-weighted images, suggestive of pheochromocytoma.
At MR spectroscopy, pheochromocytomas show a unique spectral signature with a 6.8ppm peak that may be attributed to the presence of catecholamines and catecholamine metabolites.32 However, further research is required to validate MR spectroscopy as a diagnostic tool for the characterization of pheochromocytoma.
MIBG scintigraphy and 18F-FDG PET/CT are used in the localization of biochemically suspected pheochromocytomas,28,36 but their use in incidentalomas is limited as lesions are already localized. Since MET PET/CT can differentiate adrenal metastases and pheochromocytomas from adrenocortical lesions,38 it could be useful when dealing with a suspected pheochromocytoma.
CarcinomaThe prevalence of adrenal carcinoma is clearly related to the size of the tumor (2% of tumors ≤4cm; 6% of tumors 4.1–6cm; and 25% of tumors >6cm), with larger tumors having a worse prognosis. Most studies report <50% 5-year survival, and many even report <50% at 2 years.2
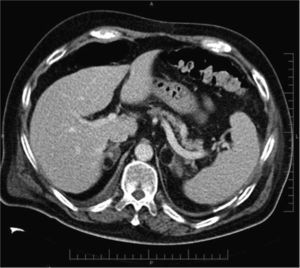
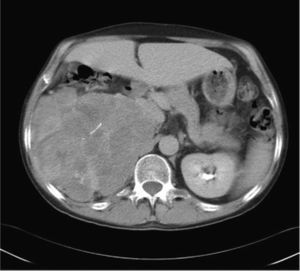
Carcinomas usually appear as large masses on CT and MR imaging (Fig. 10) accompanied by findings suggestive of malignancy (Table 1). Adrenocortical carcinomas may also extend directly into the vena cava and identification of such invasion is essential for surgical planning.71,72 Small carcinomas (<5cm) may have an appearance similar to that of adenomas,71 without invasion of adjacent structures.
Adrenal carcinoma. A 32-year-old patient investigated for hypercortisolism and hyperaldosteronism. Intravenous contrast-enhanced delayed-phase CT scan shows a large retroperitoneal mass in the right suprarenal area, with some calcifications and heterogeneous enhancement and pseudonodular areas of enhancement interspersed with low-attenuation areas. Cranial sections show signs of infiltration of the liver parenchyma, all compatible with adrenal carcinoma.
Since adrenal carcinomas have no fat content, these lesions do not lose signal intensity on opposed-phase chemical shift MR imaging. However, it has been reported one case of functioning adrenal carcinoma with intracellular lipid that contributed to the signal loss on opposed phase.73
The role of PET/CT has been already discussed in the Metastasis section.
Adrenal carcinomas are fast growing lesions and very rarely remain stable for more than 6 months if untreated. The stability of the lesions in serial follow-up (depending on the phenotype of the lesion) is usually useful to rule out a carcinoma.7,28
Management of adrenal incidentalomasScreening for pheochromocytoma and for autonomous cortisol secretion is recommended in patients with adrenal incidentaloma and no history of malignant disease. Screening for hyperaldosteronism is recommended in hypertensive patients. The exception to this includes those patients with unequivocal findings of myelolipoma.1,2,11 Routine screening for hypersecretion of androgens or estrogens is not indicated.1
Patients with asymptomatic or oligosymptomatic pheochromocytoma must undergo adrenalectomy. For the rest of subclinical functioning lesions, the surgical option will be based on the age (patients younger than 40 usually undergo surgery) and on the potential medical effects associated with excessive hormonal secretion.2,11
Although resection of non-functioning incidentalomas >6cm is the norm, there are some exceptions (acute hematomas, tuberculosis, myelolipomas and, possibly, non-functioning masses in the elderly). Conversely, resection of lesions <4cm with low risk of malignancy on imaging studies is usually not indicated. The strategy for lesions 4–6cm in size is not well established, and follow-up or resection can be considered.2,11
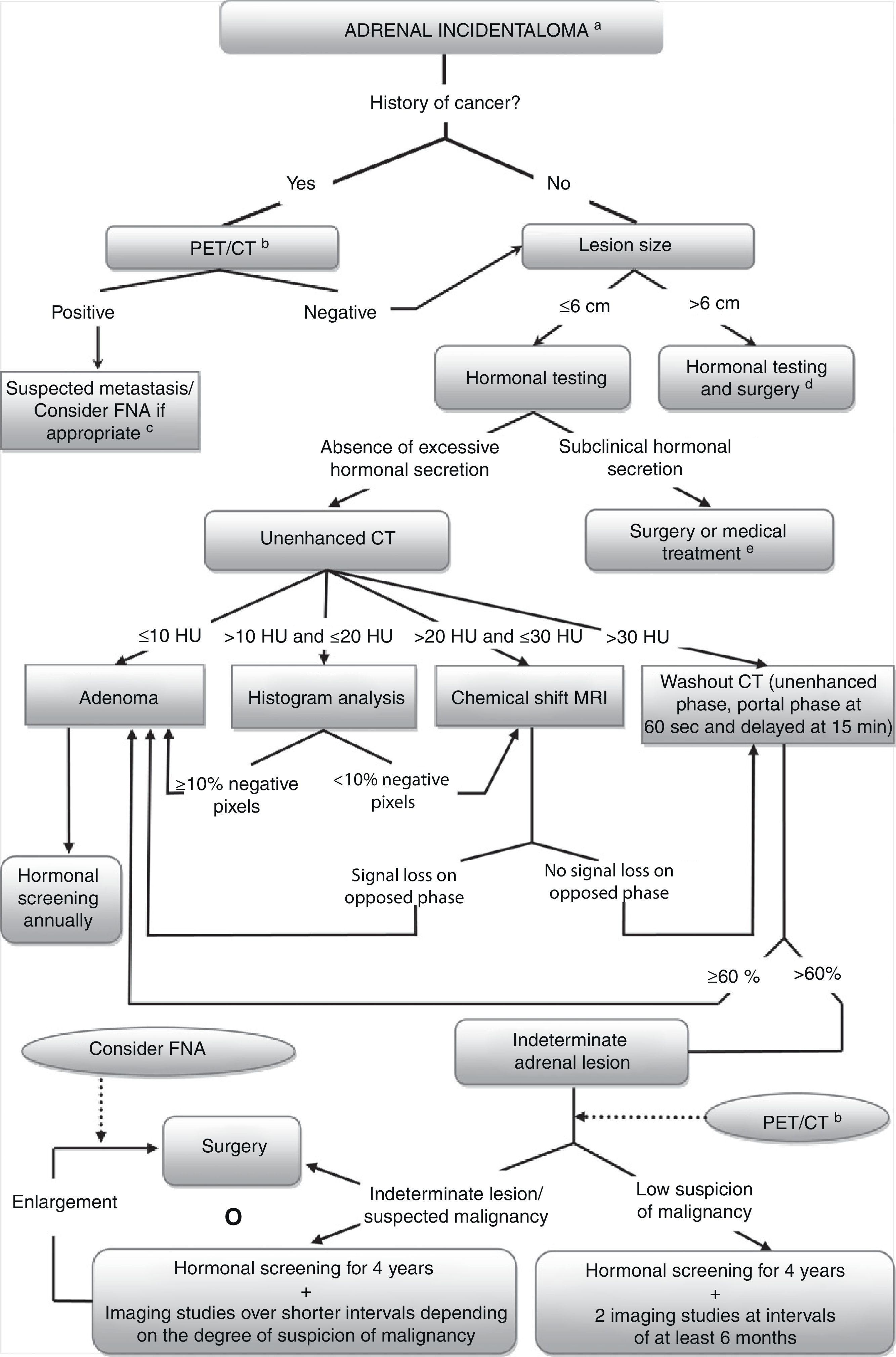
The mean attenuation values on unenhanced CT should be determined for non-functioning incidentalomas ≤6cm with no radiological evidence of malignancy. A lesion with attenuation values <10HU is diagnosed as adenoma.16,18,19 For attenuation values of 10–20HU, a histogram analysis can be performed, where a finding of >10% of negative pixels is diagnostic for adenoma.17,20,21,41 In cases of unenhanced attenuation values of 20–30HU or non-conclusive histogram, an MRI examination will be performed, where the loss of signal intensity on opposed-phase gradient-echo images is characteristic of adenoma.23,25,50,52 For lesions with attenuation >30HU, unenhanced and enhanced CT examinations (portal phase at 60s and delayed phase at 15min) and absolute washout determination are recommended. Values ≥60% are compatible with adenoma.16,42,43,45–47
A small amount of adrenal masses remains indeterminate after CT and MRI examinations, including atypical adenomas, metastases, adrenocortical carcinomas, lymphoma and pheochromocytomas. In these cases, 18F-FDG PET/CT (and MTO PET/CT in the future) is recommended; however, although this technique cannot provide accurate tissue characterization, it does help differentiate benign from malignant disease.28,36–38
If the lesion still remains indeterminate, follow-up is indicated in order to identify growth or possible hormonal hypersecretion. There is no consensus on the appropriate follow-up: for small (<3cm) non-functioning masses with benign appearance most authors1,2,11 recommend to repeat biochemical screening annually for 4 years and to perform two imaging studies with at least 6-month interval. For indeterminate lesions, in addition to the annual screening during 4 years, an early imaging study at 3–6 months is also recommended as well as subsequent studies based on the degree of suspicion.11 Lesions that have a rapid growth are usually considered malignant.7,28
Priority should be given to adrenalectomy in case of suspected malignancy (rapid growth, low lipid content, reduced washout values, heterogeneity, irregular margins).2,11
FNA is rarely indicated for an incidentaloma found in a patient without a history of malignancy and non-conclusive imaging findings.1,10,28,56 If the mass enlarges during follow-up, FNA may be performed before surgical decision-making.27
The use of 18F-FDG-PET is warranted as the initial imaging study for evaluation in oncologic patients because of the high risk of metastasis.37 A positive result is highly suggestive of metastasis, and FNA is indicated for confirmation (after hormonal testing to rule out pheochromocytoma), only if the definitive diagnosis could change the therapeutic approach.27 If the result of the PET/CT study is negative, it is recommended to follow the same approach suggested for adrenal incidentalomas in patients with no history of malignancy.
The algorithm for diagnosis and management of adrenal incidentaloma is shown in Fig. 11.
Algorithm for the management of adrenal incidentalomas. aNo additional examination is required in case of unequivocal characteristics of myelolipoma; bAdrenal uptake values greater than those of the liver on 18F-FDG PET/CT (visual analysis) are suggestive of malignant disease. cPrior to FNA, hormonal testing is recommended to rule out pheochromocytoma. dSome authors recommend resection of lesions 4–6cm in size, especially those with characteristics suggestive of malignancy (heterogeneity and irregular margins). ePatients with pheochromocytomas should undergo resection. For the rest of lesions, surgical decision-making will be based on the patient's age and on the potential medical effects associated with excessive hormonal secretion.
Radiologists should participate actively in the diagnosis of indeterminate lesions by using the appropriate imaging techniques. They have to be able to reach a conclusive diagnosis based on the behavior of the lesions, but also, they should give advice on the subsequent steps that a non-conclusive adrenal lesion requires based on the experience in the different techniques available at their institutions. Having an algorithm is essential as this allows for an appropriate management of adrenal incidentalomas.
Authorship- 1.
Responsible for the integrity of the study: ROC, RSI, CNM.
- 2.
Conception of the study: ROC, RSI, LBV, MCSC, CNM.
- 3.
Design: ROC, RSI, LBV, MCSC, CNM.
- 4.
Acquisition of data: ROC, RSI, LBV, MCSC, CNM.
- 5.
Analysis and interpretation of data: ROC, RSI, LBV, MCSC, CNM.
- 6.
Statistical analysis: ROC, RSI, CNM.
- 7.
Bibliographic search: ROC, RSI, CNM.
- 8.
Drafting of the manuscript: ROC, RSI, CNM.
- 9.
Critical review of the manuscript with intellectually relevant contributions: ROC, RSI, LBV, MCSC, CNM.
- 10.
Approval of the final version: ROC, RSI, LBV, MCSC, CNM.
The authors declare not having any conflict of interests.
Please cite this article as: Oliveira Caiafa R, et al. Manejo y diagnóstico del incidentaloma suprarrenal. Radiología. 2011;53:516–30.