Congenital heart disease (CHD), by adversely influencing vascular dynamics, jeopardizes maternal and fetal well-being. Transposition of Great Artery (TGA) with associated anomalies constitute less than 5% of the total. Reports of successful pregnancies with co-existing TGA are anecdotal.
MethodsTwo pregnants with TGA who were earlier advised against the continuation of pregnancy by cardiologists were admitted for safe confinement. Severe hypoxemia and associated features of CHD were markedly noticed in both of them. Both patients were administered titrated lumbar epidural labor analgesia with levobupivacaine for vaginal delivery.
ResultsBoth parturients underwent successful vaginal deliveries. However, hypoxemic status was reflected by significantly elevated blood lactate levels in both patients.
ConclusionContinuation of pregnancy could entail unacceptable risk in patients with TGAs. Patients should be made aware of the risk to life borne for the sake of the unborn; and termination should be advised at the earliest convenience in case the patient agrees.
La cardiopatía congénita pone en riesgo el bienestar materno-fetal debido al potencial efecto hemodinámico del bloqueo regional. La trasposición de las grandes arterias (TGA) constituye menos del 5% del total de las enfermedades cardíacas y pocos casos han sido reportados exitosamente en embarazadas sometidas a anestesia neuroaxial.
MétodosDos pacientes gestantes portadoras de TGA con indicación de anticoncepción por riesgo de vida fueron tratadas. En ambas pacientes se observó hipoxemia severa, habiendo sido intervenidas con técnica epidural lumbar con levobupivacaína para el trabajo de parto.
ResultadosLos nacimientos fueron satisfactorios en ambos casos a pesar de que la condición hipoxémica se reflejara en los niveles de lactato sanguíneo.
ConclusiónLa continuación del embarazo podría entrañar riesgo inaceptable en pacientes con TGA. La paciente debe ser consciente del riesgo de vida fetal y la terminación debe ser aconsejada con la mayor brevedad posible si el paciente está de acuerdo.
Pregnancy, as it advances, is accompanied by a slew of alterations in maternal hemodynamics. Congenital heart disease (CHD), by worsening vascular dynamics, jeopardizes maternal and fetal wellbeing. The uncommon association of uncorrected maternal cyanotic CHD and pregnancy does contribute to a significant maternal mortality rate.1 Maternal and fetal mortality to the tune of 12–33% and 30–54% respectively have been reported in Eisenmengers syndrome.2 Transposition of Great Artery (TGA) with associated anomalies constitute less than 5% of the total, and successful pregnancies with coexisting TGAs have hardly been reported. A ‘Medline’ search revealed scarce reports linking TGA and dextrocardia with normal delivery, labor analgesia or lumbar epidural. We herein report uneventful successful vaginal deliveries under lumbar epidural labor analgesia in two parturients complicated by TGAs.
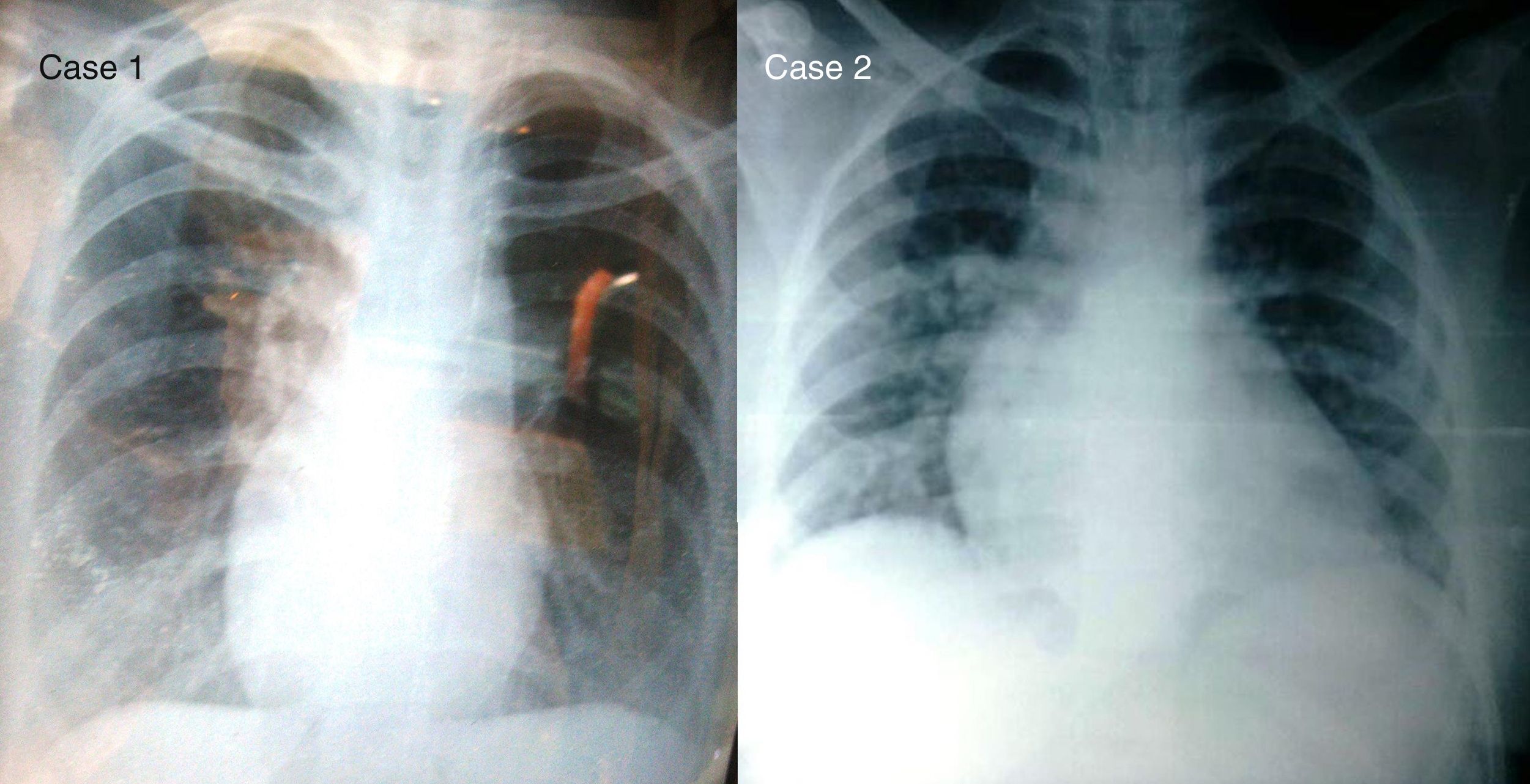
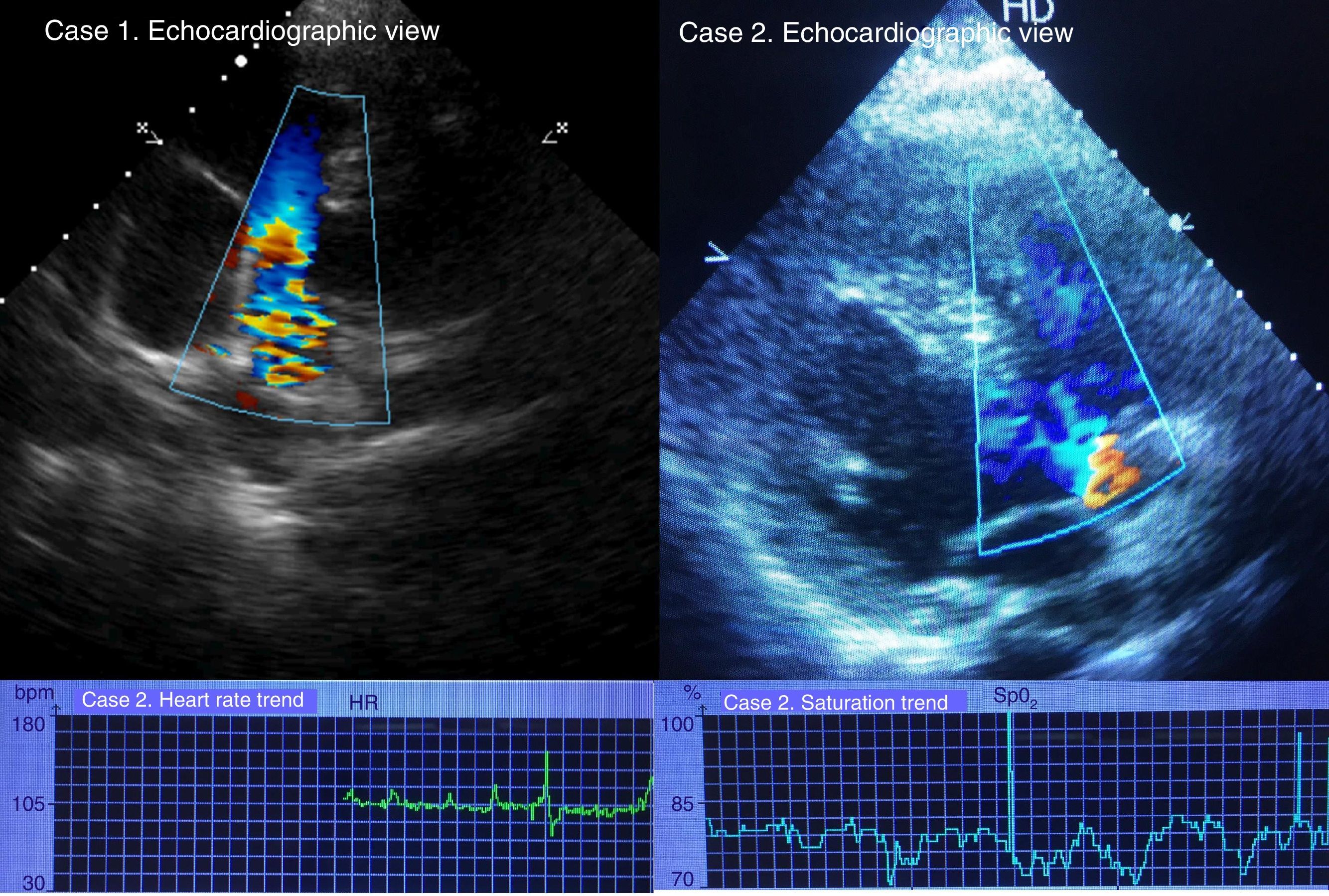
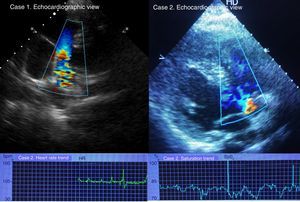
Case presentationCase 1A 28-year-old, 62kg, who was admitted at 32 weeks of gestation, for safe confinement, gave history of intermittent palpitations and breathlessness; New York Heart Association grade II. Physical examination revealed central cyanosis and a grade 3/6 ejection systolic murmur (ESM), saturation of 86% in room air. Her investigations revealed normal renal functions, electrolytes, coagulation functions and albumin 3.5. Blood gas analysis showed pH of 7.47, pCO2 29mmHg, pO2 of 59.5mmHg, base excess (BE) of −1.4 and bicarbonate of 23.9 on room air. Her serum lactate (La−) level was 19.6mg/dl. Electrocardiogram (ECG) showed normal sinus rhythm but axis deviations. The chest skiagram (CXR) was unremarkable (Fig. 1). Echocardiogram revealed dextrocardia, TGA and double outlet right ventricle (DORV), large sub-aortic ventricular septal defect (VSD) with bi-directional shunt, severe infundibular pulmonary stenosis (PS) and dilated right atrium and RV (Fig. 2).
Case 2A 24-year-old known CHD was referred to our hospital with early labor pain. She had past history of Blalock Tausig shunt done 7years ago but without correction of TGAs. Physical examination revealed clubbing, central cyanosis, grade 2/6 ESM and room air saturation of 60%. She had Hb of 16.5g/dl, normal renal and coagulation profiles. Her blood gas analysis showed pH of 7.52, pCO2 19.4mmHg, pO2 of 69mmHg, BE of −4.2 and bicarbonate of 20.9 on 5liters/min oxygen flow. Her La− level was 23.9mg/dl. Echocardiogram revealed d-TGA, VSD with bi-directional shunt, severe PS with peak gradient across the valve 90mmHg and dilated right atrium and RV. She had OS-atrial septal defect (ASD) with shunt across (Fig. 2).
At admission, ultra-sonogram showed Intra Uterine Growth Retardation (IUGR) of the fetus in both of these patients and oligohydromniosis in case 1. While the decision to terminate the pregnancy was taken in maternal interest, vaginal delivery was preferred over a caesarian section in view of the surgical risks involved and a favorable utero-fetal environment in both patients. Lumbar epidural analgesia was planned for labor and delivery. Prostaglandin E1(PGE1) assisted labor induction was done under infective endocarditis prophylaxis in both. Uterine, fetal and patient's cardiovascular monitoring were carried out. A second PGE1 was instituted after cervical dilatation failure, 6h after the first in case 1. When signs of labor progression were noted, a lumbar epidural catheter was inserted at the level of L3–4 using air-syringe loss of resistance technique in sitting position in both cases. Co-loading of 200ml of ringer lactate and supine-lateral tilt position were simultaneously instituted. A radial artery catheter was used for hemodynamic monitoring in both patients.
A bolus epidural dose of levobupivacaine of 12ml of 0.0625% with 1μgm/ml fentanyl was administered over 10min. A T9/10 level of sensory blockade was achieved and patients had adequate pain relief. The maximum fall in heart rate and blood pressure was within 13% from base line values. Over subsequent 70min, a top up of 8ml of 0.1% of levobupivacaine with 2μgm/ml fentanyl was administered in case1 and 25ml of 0.125% (fentanyl, 2μgm/ml) over 2.5h in case 2. Furthermore, 0.1% of local anesthetic with similar concentration of fentanyl was infused at the rate of 8ml/h in case 1.
A repetitive trans-thoracic echocardiac evaluation was done for both. Invasive monitoring with central venous pressure was considered only if necessary. During labor, continuous oxygen was administered via face mask. The saturation and heart rate trend graphs are shown in Fig. 2 for case 2. The sensory and motor blockade was assessed continuously. No motor effects were observed and the level of T8–10 sensory blockade was maintained in both. During subsequent hours, with full cervical dilatation and vertex ‘zero’ station, successful vacuum assisted vaginal delivery was achieved in both patients. The babies had adequate APGAR scores. The blood La− level measured after delivery was higher (24.3mg/dl, 37mg/dl respectively for case 1 and 2). Total injected levobupivacaine and fentanyl were 80mg, 120μg (case 1) and 32.5mg, 70μg (case 2), respectively.
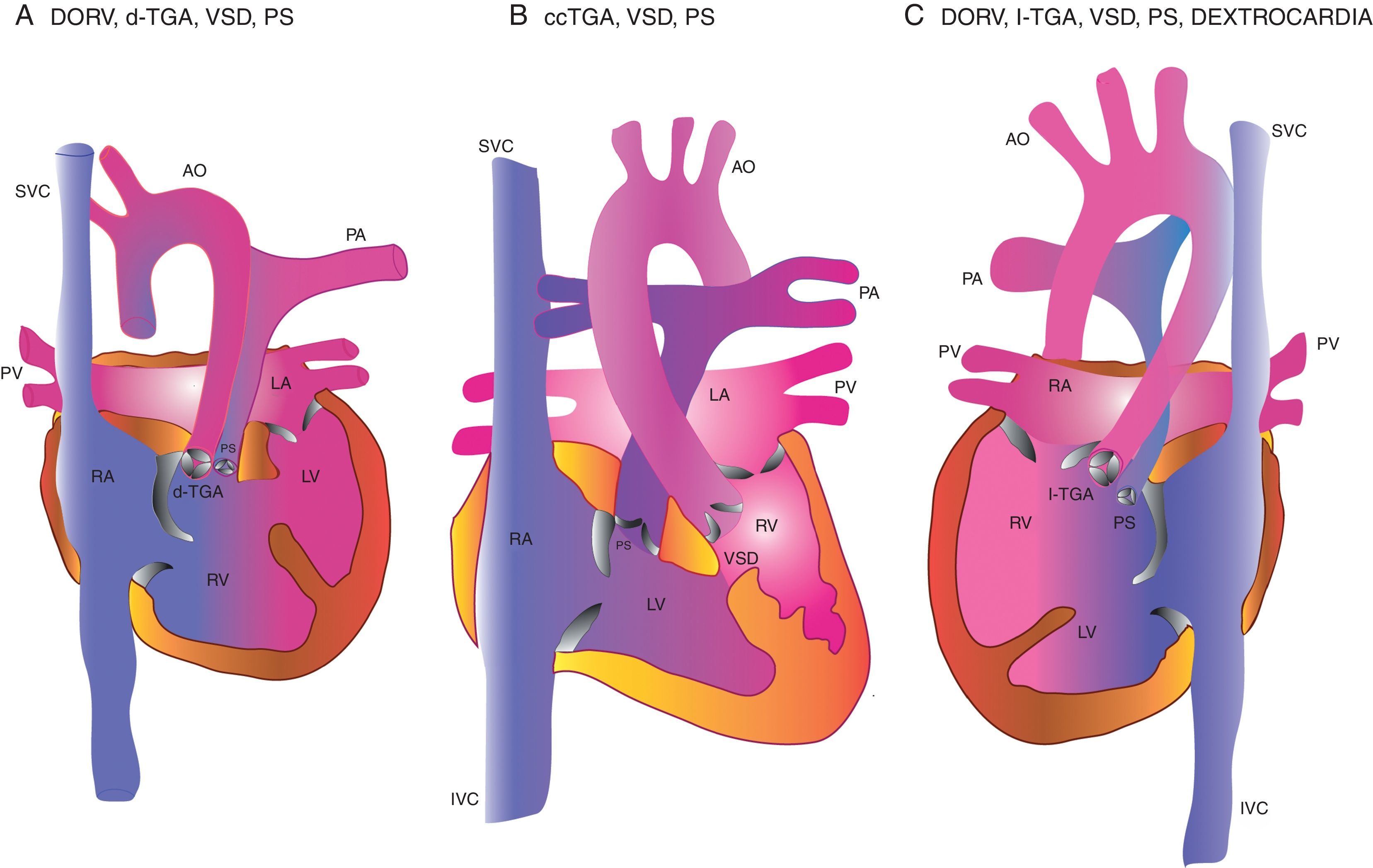
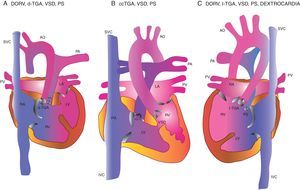
DiscussionAttempts to understand the variants associated with TGA anomaly are bewildering due to inconsistency in the use of nomenclatures. Katryn Rouine-Rapp classifies these as d-TGA and congenitally corrected TGA (ccTGA) based on nomenclature established by the European Association for Cardiothoracic Surgery.3 The former (d-TGA) is sub-classified into (a) TGA with intact ventricular septum, (b) TGA with VSD, (c) TGA with left ventricular outflow tract obstruction (LVOTO). To mention three types among the many variants described, (a) DORV with dextro-TGA, (b) congenitally corrected TGA [ccTGA], (levo-TGA) and (c) DORV, levo-TGA with dextrocardia are shown in Fig. 3.
Transposition of Great Arteries; few variants. Case 1 had the third variety and case 2 had the first.
SVC: superior vena cava; AO: aorta; PA: pulmonary artery; RA: right atrium; RV: right ventricle; LA: left atrium; LV: left ventricle; PV: pulmonary vein; IVC: inferior vena cava; VSD: ventricular septal defect; PS: pulmonary stenosis.
In our series, case 1 had the third variety and case 2 had the first variety (Fig. 3). In case 1, the aorta was anterior and to the left of the pulmonary artery (PA), but typically side-by-side in location. This variety constitutes only 7% of all types of the TGA anomaly where blood streaming specificity to a particular artery is favored.3 In both patients, both arteries arose from the RV. Presence of a large VSD channelizes oxygenated blood toward RV/aortic opening from the LV. This flow is further complemented by a severely stenosed pulmonary valve for similar redirection of deoxygenated blood to the PA. Pathophysiology and clinical manifestations vary greatly with the varieties and are definitely influenced by the type and severity of VSD and PS. Successful pregnancy and delivery under lumbar labor epidural, in few other variants of TGA (ccTGA) has been reported previously.4–6 The ‘ZAHARA’ pregnancy with CHD outcome research investigated 71 patients with varieties of TGA.7 Twelve and 6 had cardiac arrhythmia and heart failure, respectively, as peripartum cardiac complications. This incidence was higher than any other form of CHD described in the study (83 of 1302 CHD studied) and suggests TGA's association with cardiac events.
It is universally known that during the second stage of labor and delivery, the cardiac output increases up to 80%, and this may result in ventricular failure. Our patients had bi-directional shunt flow with mixing and this was worse in case 2 even with the earlier shunt procedure. The shunt will be the decider of adequacy of oxygenation in increasing oxygen demand status during labor and delivery. Clubbing and cyanosis was probably due to PS induced diminished PA blood flow. Accompanied with pregnancy-related additional fall of pulmonary resistance, detrimental effects can be encountered especially with sympathetic block of lumbar epidural. In contrast, pain, acidosis and hypoxemia can worsen preexisting low pulmonary flow status and the role of epidural analgesia is vital. Plasma lactate levels are measured with the intention of detecting the extent of tissue hypoxemia.8 The higher postpartum lactate levels compared to prepartum could be an indicator of a degree of hypoxemia during labor and delivery, partly offset by the pain relief.
Maintenance of SVR, intravascular volume, venous return and prevention of aortocaval compression were taken care during labor. The saline filled syringe is preferred over the air filled one while the ‘loss of resistance’ technique is being used; for the fear of paradoxical air embolism with use of the latter. Among many available monitors, LiDCOplus (lithium indicator dilution calibration system) monitor is the only minimally invasive continuous data provider which is currently recommended. However its use was limited by its availability.9 A continuous telemetry monitoring is preferred owing to the high incidence of arrhythmias.1 If an urgent cesarean delivery is planned, it is best performed in the cardiac operating room with immediate availability of cardiopulmonary bypass.10 We did not encounter hemodynamic fluctuations with epidural bupivacaine injections in our patients.
With the benefit of hindsight, logistics of subjecting a patient of CHD to a normal vaginal delivery should be discussed with the cardiologist when continuation of pregnancy could entail unacceptable risk. Patients should be made aware of the risk of maternal life undertaken for the sake of the unborn; and termination should be advised at the earliest convenience in case the patient agrees. It is advised that from 24 weeks gestation, the anesthesia team should be pro-actively involved to enable pragmatic planning for support during labor and delivery.11 The methodology used in our cases being the same as that performed in a healthy parturient, we believe that successful delivery in complex heart disease pregnants is possible and meaningful especially in developing countries.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestNone declared.
I express my sincere thanks to Dr. Kavitha D'Souza, M.D., Prof and HOD, Department of Obstetrics and Gynecology, AJIMS, Mangalore, for her kind assistance.