Optical coherence tomography (OCT) can provide essential information on unclear coronary angiography images. In current consensus documents of OCT imaging interpretation, calcium is usually described as a signal-poor or heterogeneous region with a sharply delineated border, but it may have atypical features, such as the proposed “calcified nodule” entity. In this case, a stable patient presented a hazy intracoronary angiographic image. OCT imaging showed an odd-looking convex, protruding lesion with irregular borders and high attenuation likely related to a calcified nodule. The lesion had a complex relation to the left circumflex artery take-off, which was better understood after three-dimensional reconstruction.
A tomografia de coerência óptica (TCO) pode fornecer informações essenciais sobre imagens de angiografia coronária pouco claras. Em documentos de consenso atuais de interpretação de imagem de TCO, o cálcio é geralmente descrito como uma região de sinal óptico de baixa intensidade ou heterogêneo, com uma borda bem delineada, que pode ter características atípicas, como a que caracteriza o nódulo calcificado. Neste caso, um paciente estável apresentava uma imagem angiográfica intracoronária nebulosa. A imagem da TCO mostrava uma lesão convexa protuberante de aparência estranha, com bordas irregulares e alta atenuação, provavelmente relacionada a um nódulo calcificado. A lesão tinha uma relação complexa com a origem da artéria circunflexa, o que foi melhor compreendida após a reconstrução tridimensional.
Optical coherence tomography (OCT) is an invaluable tool for assessing in vivo morphological characteristics of unclear intracoronary findings in angiography. Therefore, it may provide crucial information to guide treatment decisions. Some optical characteristics are associated with different plaque components, such as fibrous tissue, lipid and calcium. Calcium is usually described as a signal-poor or heterogeneous region with a sharply delineated border.1 Other proposed calcium-related images include small spotty calcifications, large superficial calcific arches (both associated with plaque instability)2,3 and large protruding lesions with hyper-intense borders and high attenuation, resembling red thrombus, but in stable patients.4
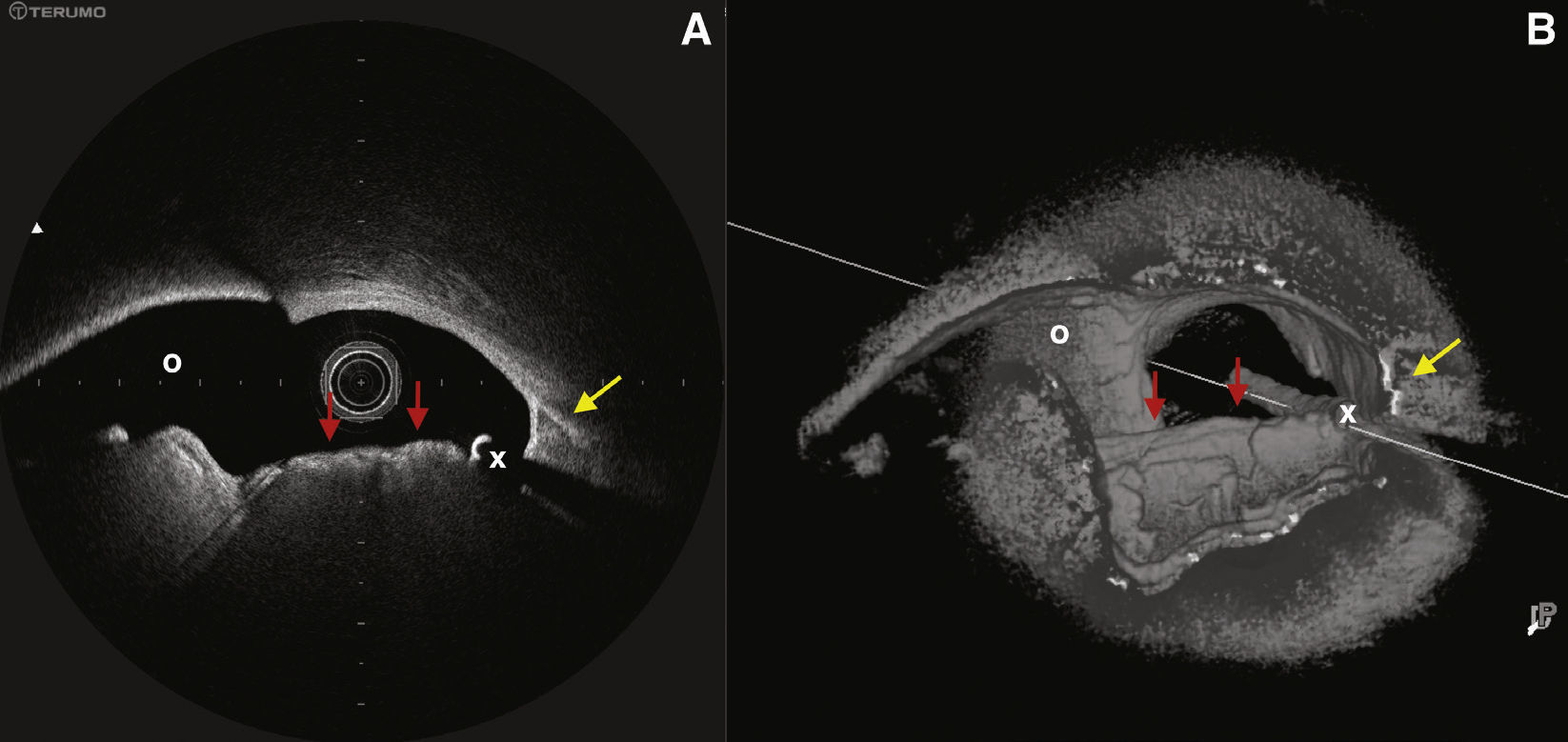
Case reportWe present a case of an 83-year-old male patient referred for coronary angiography during the evaluation for an aortic valve replacement due to severe aortic stenosis. He had neither angina nor any symptoms other than breathlessness attributable to the aortic stenosis. He had history of percutaneous coronary intervention (PCI) in the left main coronary artery (LMCA), left anterior descending (LAD) and right coronary (RCA) arteries 5 years ago, performed in the context of a non-ST elevation myocardial infarction. He also had previous history of hypertension, dyslipidemia, insulin-treated diabetes mellitus, chronic obstructive pulmonary disease (former smoker), lower digestive tract haemorrhages, and peripheral artery disease. Angiography showed a good result of the stent in the LMCA but with a large hazy image in the distal LMCA, causing a mild stenosis of the LAD ostium and an apparently severe stenosis in the left circumflex artery (LCx) ostium. The LAD and RCA stents showed no significant restenosis and there were no significant de novo lesions (video 1 – supplementary material). OCT (Lunawave®, Terumo, Tokyo, Japan) was performed to clarify anatomy and severity of the distal LMCA plaque (Video 2 – supplementary material). The stent in the LMCA was shown to be slightly underexpanded and oval-shaped due to an eccentric calcified plaque, but it was well apposed with full endothelization. At the distal LMCA, a protruding mass of irregular, convex border, was causing a focal mild stenosis of the LAD ostium and a more severe, but focal, stenosis of the left circumflex artery ostium (Fig. 1). The image had bright, high-intensity borders with high signal attenuation, or shadow. This could be compatible with the classical description of red thrombus or, rarely, to lipid rich fibroatheroma (albeit fibroatheroma is not usually seen as a protruding mass).1 The mass was contiguous to typical calcium image in the LMCA and LAD. Luminal areas were difficult to measure due to the irregular shape of the bifurcation lesion, but three-dimensional reconstruction helped to understand its morphology (Video 3 – supplementary material).
(A) Image obtained by optical coherence tomography at distal left main coronary artery bifurcation. (B) Three-dimensional reconstruction of the same region. Red arrows: irregular-bordered protruding image with high signal attenuation, compatible with calcium nodule; yellow arrow: contiguous typical calcified area (continues along the left anterior descending artery and left main coronary artery in the longview). O: left circumflex artery ostium; X: wire artifact.
Analysing the angiogram and OCT images of the lesion and surrounding plaque, as well as the stable situation of the patient, the mass was interpreted to be a calcified nodule. Given the limitations of fractional flow reserve in the setting of aortic stenosis and the absence of angina, we decided not to perform PCI and to proceed to aortic valve replacement. Left ventricular function was in the lower normal limits (50%), without segmental defects of contractility. The patient was discussed in a heart team meeting and we decided to undergo transcatheter aortic valve implantation (TAVI). The procedure was uneventful. However, the patient had a complicated post-procedure course, with renal failure requiring dialysis, lower digestive tract haemorrhage and decompensated heart failure in spite of no changes in left ventricular function. He eventually died 5 weeks after the procedure. No ischemic events were documented during peri and post-TAVI procedure, but the impact of the coronary artery disease on the outcome cannot be ruled out.
This case illustrates several important aspects of modern interventional cardiology. OCT was a useful tool in assessing the nature and severity of the intriguing lesion. However, the images were not pathognomonic of a particular etiology. The presence of a red thrombus cannot be completely ruled out. However, a calcified nodule seems to be the most likely nature of this intracoronary mass, given the stability of the patient, the angiography images and the OCT findings. It is noteworthy the resemblance to a previously reported case, which had pathologic demonstration of a calcified nodule with full endothelial coverage and no evidence of thrombi.4 Calcium may present with different histological patterns (and therefore different OCT features), probably reflecting different pathophysiological background, stage of plaque development or the presence of associated features, such as subtended neovascularization4 or recent intra-plaque hemorrhage.5 The unfortunate clinical outcome of this case was probably due to previous comorbidities, although the impact of the coronary artery disease cannot be ruled out. Much is still to be known regarding the phenomenon of calcium deposition in coronary arteries. Different patterns probably reflect different physiology, and maybe in the future this will dictate different treatment approaches. OCT is an invaluable tool for providing pathophysiological information, but images must always be interpreted with caution.
Supplementary material associated with this article can be found in the online version.
None declared.
The authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.