Complete anatomical myocardial revascularization is associated with better angina control and lower rates of cardiac events. However, in a significant number of patients treated by percutaneous coronary intervention (PCI), complete revascularization is not achieved. Thus, the aim of this study was to evaluate factors associated with incomplete myocardial revascularization (IMR) in multivessel PCI patients.
MethodsThis was a cohort study involving 1,049 prospectively and consecutively revascularized patients through PCI with treatment of two or more vessels, between 2012 and 2014, divided into two groups: IMR (n = 324; 30.9%) and complete myocardial revascularization (n = 725; 69.1%).
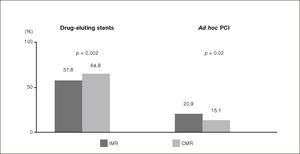
ResultsIMR was significantly associated with older age (66.5 years vs. 64.1 years; p = 0.003), arterial hypertension (92.2% vs. 86.0%; p = 0.006), chronic renal failure (36.4% vs. 26.0%; p < 0.001), acute coronary syndrome (26.3% vs. 21.0%; p = 0.05), previous surgical revascularization (16.1% vs. 7.1%; p = 0.001), saphenous venous graft lesions (3.4% vs. 1.0%, p < 0.001), and chronic occlusions (3.3% vs. 1.4%, p = 0.005), as well as lower access to drug-eluting stents (57.8% vs. 64.8%; p = 0.002). In-hospital clinical outcomes did not differ between the groups.
ConclusionsIMR occurred in approximately one-third of treated cases, and a significant association was observed with a higher-risk clinical profile and with target lesion interventions commonly associated with lower procedure success. The degree of revascularization had no impact on in-hospital clinical outcomes.
A revascularização miocárdica anatômica completa está associada a um melhor controle dos sintomas anginosos e a menores índices de eventos cardíacos maiores tardios. No entanto, em substancial número de pacientes tratados por meio de intervenção coronária percutânea (ICP), não logramos sua obtenção. Assim, nosso objetivo foi avaliar os fatores associados à revascularização miocárdica incompleta (RMI) em casos de ICP multiarterial.
MétodosEstudo de coorte envolvendo 1.049 pacientes revascularizados de forma prospectiva e consecutiva por meio de ICP com tratamento de dois ou mais vasos, entre 2012 e 2014, divididos em dois grupos: RMI (n = 324; 30,9%) e revascularização miocárdica completa (n = 725; 69,1%).
ResultadosA RMI foi significativamente associada a faixa etária maior (66,5 anos vs. 64,1 anos; p = 0,003), hipertensão arterial (92,2% vs. 86,0%; p = 0,006), insuficiência renal crônica (36.4% vs. 26.0%; p < 0,001), síndrome coronariana aguda (26,3% vs. 21,0%; p = 0,05), revascularização cirúrgica prévia (16,1% vs. 7,1%; p = 0,001), lesões em enxertos venosos (3,4% vs. 1,0%; p < 0,001) e oclusões crônicas (3,3% vs. 1,4%; p = 0,005), bem como a menor acesso a stents farmacológicos (57,8% vs. 64,8%; p = 0,002). Os resultados clínicos hospitalares não diferiram entre os grupos.
ConclusõesA RMI ocorreu em cerca de um terço dos casos tratados, tendo sido observada associação significativa, com um perfil clínico de maior risco e com intervenções em lesões alvo comumente associadas com menor sucesso do procedimento. O grau de revascularização não gerou impacto nos resultados clínicos da fase hospitalar.
When compared to surgical treatment, percutaneous coronary interventions (PCI) currently account for more than three-quarters of revascularization procedures performed in tertiary care hospitals. However, one of the limitations of this procedure, obtaining complete myocardial revascularization (CMR), still occurs despite great advancements in the technique.1,2
CMR, whatever the type of revascularization used, has been widely preferred as it is associated with higher event-free survival and a better quality of life in treated patients, due to better control of the symptoms caused by coronary heart disease.1,3,4 Recently, a randomized clinical trial that involved acute coronary syndrome (ACS) cases additionally suggested that even in this scenario, attaining a complete revascularization, treating non-culprit lesions early is more advantageous than incomplete myocardial revascularization (IMR), confirming the benefits of CMR.5
However, for a number of reasons, a significant number of patients do not achieve complete revascularization, as a result of clinical and angiographic factors, as well as variables related to the revascularization procedures themselves, resulting in IMR, which should be avoided whenever possible.1,3–7
The aim of this research was to identify the different factors associated with IMR in a series of patients with multivessel coronary heart disease submitted to PCI for the treatment of at least two vessels.
MethodsBetween June 2012 and June 2014, 2,572 patients were consecutively submitted to PCI at our institution, a large tertiary hospital, of which 1,049 (40.7%) had multivessel coronary artery disease and had two or more treated vessels. These cases were divided into IMR (n = 324; 30.9%) and CMR (n = 725; 69.1%) groups. Patients were identified using a computer database and were prospectively included. The study was observational. There were no specific exclusion criteria, i.e., all cases that underwent multivessel PCI with the minimum treatment of two vessels were included in the analysis.
Drug-eluting and bare-metal stents were used. PCI was performed using the conventional technique, with direct stent implantation or pre-dilation left to the discretion of the interventional cardiologist responsible for its performance. Adjunctive pharmacology consisted of unfractionated heparin at a dose 70 to 100 IU/kg, administered immediately before the procedure, in order to achieve an activated clotting time ≥ 250seconds; acetylsalicylic acid (loading dose of 200mg and was maintenance dose of 100mg daily) started at least 1 day before the intervention and was maintained indefinitely; and clopidogrel (loading dose of 300 or 600mg, and maintenance dose of 75mg daily). In some ACS cases, prasugrel or ticagrelor was prescribed in usual doses. The dual antiplatelet regimen was maintained for 30 days in bare-metal stent patients, and for 6 to 12 months in drug-eluting stent and/or ACS patients.
For PCI to be indicated, patients had to have symptomatic or induced myocardial ischemia and at least one lesion with diameter stenosis ≥ 70% by the visual criteria in two or more target vessels. The treated vessels were differentiated into major epicardial vessels (left anterior descending, right coronary and left circumflex arteries), secondary branches, or venous grafts. Left ventricular function was assessed by visual analysis in the right anterior oblique view, and moderate-to-severe impairment was considered with 45% or lower ejection fraction.
The decision regarding the degree of revascularization to be achieved was established by individual analysis of clinical characteristics, the results of functional tests, and the characteristics of target lesions observed at coronary angiography. In some selected patients, techniques such as intravascular ultrasound and fractional flow reserve were used as auxiliary methods in the therapeutic decision-making process.
Procedures were considered successful when residual stenosis < 20% was obtained by the visual criteria in the absence of major complications (death, myocardial infarction, or urgent bypass surgery). Acute myocardial infarction was characterized as the development of pathological Q-waves in at least two contiguous leads in the 12-lead electrocardiogram and/or an elevation in creatine kinase-MB fraction more than three-fold higher than normal levels. CMR was defined as treatment of all coronary artery vessels (main or secondary) > 2.0mm in diameter and ≥ 70% diameter stenosis,6 and IMR was defined as the inability to treat all coronary vessels >70% diameter stenosis.
Statistical analysisQuantitative variables were described as absolute numbers and percentages, and compared with the Chi-Squared test. Qualitative variables were shown as mean and standard deviation, and compared using the Student's t-test. The software Statistical Package for Social Sciences (SPSS) version 17, Minitab version 16, and Excel 2010 were used, considering significant values of p < 0.05.
ResultsSlightly over 40% of patients treated in the period met the study inclusion criteria and nearly one-third of them were of IMR.
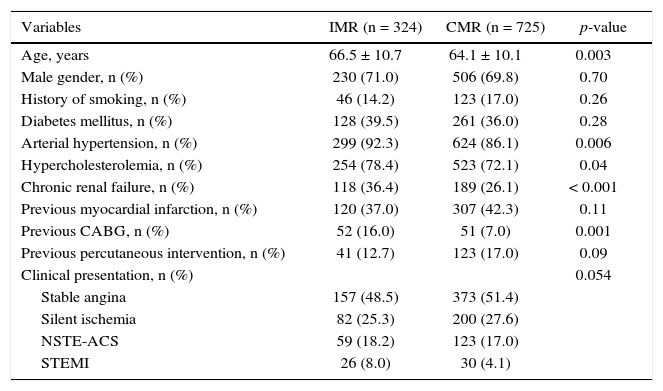
Table 1 depicts the main baseline clinical characteristics, which showed clear differences between the groups, confirming the more complex clinical profile of the IMR group. There was a predominance of older age, previous surgical revascularization, and chronic renal dysfunction. The ACS clinical presentation also prevailed in the IMR group.
Clinical characteristics.
| Variables | IMR (n = 324) | CMR (n = 725) | p-value |
|---|---|---|---|
| Age, years | 66.5 ± 10.7 | 64.1 ± 10.1 | 0.003 |
| Male gender, n (%) | 230 (71.0) | 506 (69.8) | 0.70 |
| History of smoking, n (%) | 46 (14.2) | 123 (17.0) | 0.26 |
| Diabetes mellitus, n (%) | 128 (39.5) | 261 (36.0) | 0.28 |
| Arterial hypertension, n (%) | 299 (92.3) | 624 (86.1) | 0.006 |
| Hypercholesterolemia, n (%) | 254 (78.4) | 523 (72.1) | 0.04 |
| Chronic renal failure, n (%) | 118 (36.4) | 189 (26.1) | < 0.001 |
| Previous myocardial infarction, n (%) | 120 (37.0) | 307 (42.3) | 0.11 |
| Previous CABG, n (%) | 52 (16.0) | 51 (7.0) | 0.001 |
| Previous percutaneous intervention, n (%) | 41 (12.7) | 123 (17.0) | 0.09 |
| Clinical presentation, n (%) | 0.054 | ||
| Stable angina | 157 (48.5) | 373 (51.4) | |
| Silent ischemia | 82 (25.3) | 200 (27.6) | |
| NSTE-ACS | 59 (18.2) | 123 (17.0) | |
| STEMI | 26 (8.0) | 30 (4.1) |
IMR: incomplete myocardial revascularization; CMR: complete myocardial revascularization; CABG: coronary artery bypass grafting; NSTE-ACS: non-ST-elevation acute coronary syndrome; STEMI: ST-segment elevation myocardial infarction.
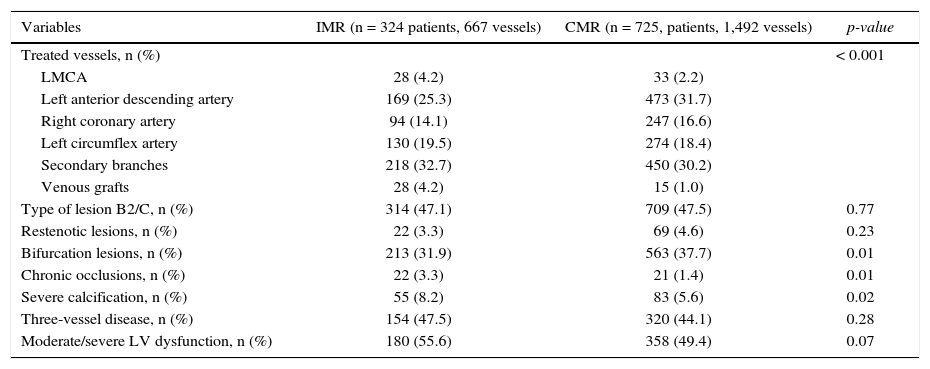
Among the data associated with pre-procedure coronary angiography (Table 2), this study observed a higher percentage of lesions with severe calcification, interventions in venous grafts, and chronic occlusions in the IMR group; on the other hand, in the CMR group, PCI predominated for the treatment of bifurcations and left anterior descending artery lesions. The other characteristics did not differ between the groups.
Characteristics of pre-procedure angiography.
| Variables | IMR (n = 324 patients, 667 vessels) | CMR (n = 725, patients, 1,492 vessels) | p-value |
|---|---|---|---|
| Treated vessels, n (%) | < 0.001 | ||
| LMCA | 28 (4.2) | 33 (2.2) | |
| Left anterior descending artery | 169 (25.3) | 473 (31.7) | |
| Right coronary artery | 94 (14.1) | 247 (16.6) | |
| Left circumflex artery | 130 (19.5) | 274 (18.4) | |
| Secondary branches | 218 (32.7) | 450 (30.2) | |
| Venous grafts | 28 (4.2) | 15 (1.0) | |
| Type of lesion B2/C, n (%) | 314 (47.1) | 709 (47.5) | 0.77 |
| Restenotic lesions, n (%) | 22 (3.3) | 69 (4.6) | 0.23 |
| Bifurcation lesions, n (%) | 213 (31.9) | 563 (37.7) | 0.01 |
| Chronic occlusions, n (%) | 22 (3.3) | 21 (1.4) | 0.01 |
| Severe calcification, n (%) | 55 (8.2) | 83 (5.6) | 0.02 |
| Three-vessel disease, n (%) | 154 (47.5) | 320 (44.1) | 0.28 |
| Moderate/severe LV dysfunction, n (%) | 180 (55.6) | 358 (49.4) | 0.07 |
IMR: incomplete myocardial revascularization; CMR: complete myocardial revascularization; LMCA: left main coronary artery; LV: left ventricle.
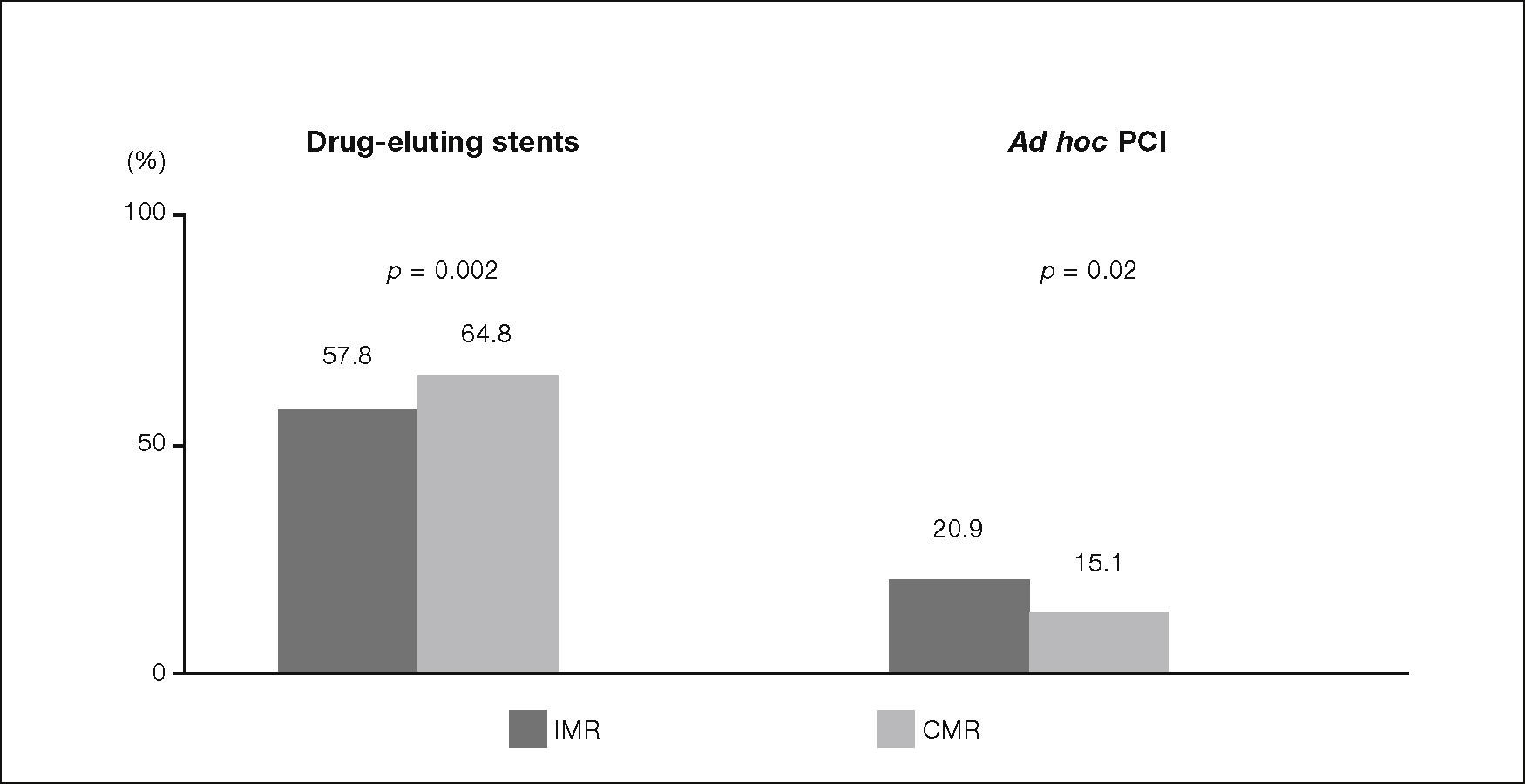
Regarding the variables of the procedure, the highest percentages of drug-eluting stents use were recorded in the CMR group, and of ad hoc PCI, in the IMR group (Fig. 1). The other data showed no significant differences between the groups, emphasizing that most PCI addressed two vessels (93.8% vs. 92.4%; p = 0.41); in the interventions, there was a predominance of stent implantation with a length of 18mm or longer (67.0% vs. 66.2%; p = 0.74). Almost 50% of the cases received stents < 3.0mm (49.3% vs. 46.2%; p = 0.19).
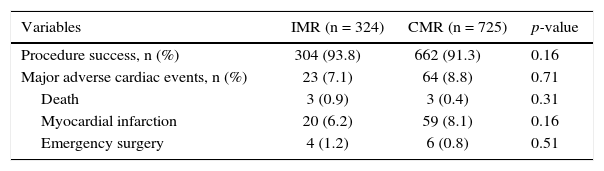
Finally, Table 3 shows the main clinical outcomes of the in-hospital stay, which did not differ between the groups.
In-hospital clinical outcomes.
| Variables | IMR (n = 324) | CMR (n = 725) | p-value |
|---|---|---|---|
| Procedure success, n (%) | 304 (93.8) | 662 (91.3) | 0.16 |
| Major adverse cardiac events, n (%) | 23 (7.1) | 64 (8.8) | 0.71 |
| Death | 3 (0.9) | 3 (0.4) | 0.31 |
| Myocardial infarction | 20 (6.2) | 59 (8.1) | 0.16 |
| Emergency surgery | 4 (1.2) | 6 (0.8) | 0.51 |
IMR: incomplete myocardial revascularization; CMR: complete myocardial revascularization.
Angiographic IMR is a common situation in routine cardiology practice, observed in slightly over 30% of the cases assessed in this study, lower than the almost 48% observed in the contemporary SYNTAX study (PCI group), and close to the 37% noticed in the ACUITY (Acute Catheterization and Urgent Intervention Triage StrategY) trial, i.e., both in the elective and in the unplanned scenarios, the percentages of IMR are significant.3–7
This observation is clinically relevant, as IMR is accompanied by higher rates of symptom recurrence and major cardiac events in the late phase, including mortality.3–9 The results of a recent meta-analysis involving nearly 90,000 patients confirm this statement, as, in cases in which CMR was obtained, significant reductions in mortality (29% reduction), myocardial infarction (22% reduction), and additional revascularizations (26% reduction) were observed, results that occurred regardless of the revascularization method used (PCI or surgery) and the definition employed (angiographic or functional criteria). Other reports have shown the same trend in both elective situations or in the presence of ACS.4 Thus, it becomes evident that, when feasible, CMR is preferable and beneficial. However, as explained before, due to a series of clinical, functional, and angiographic factors, the ideal degree of revascularization is not effectively achieved in many situations, characterizing incomplete revascularization.3–7
In this study, carried out in the real-world scenario of PCI, which evaluated only cases submitted to multivessel intervention, characteristics were identified that predisposed patients to IMR, as follows: older age, hypertension, chronic renal failure, prior coronary artery bypass surgery, ACS, saphenous venous grafts lesions or chronic occlusions, PCI of vessels other than the left anterior descending artery or bifurcation lesions, non-availability of drug-eluting stents, and ad hoc interventions.
The subanalysis of the ACUITY trial, carried out in the setting of ACS, showed similar results, except for cases of PCI in patients with previous coronary artery bypass surgery and, consequently, in target lesions located in saphenous vein bypass grafts. Possibly, because it is a trial performed only in cases of ACS, patients with elevation in pre-procedure cardiac biomarkers and patients with noninvasive risk stratification were identified as high risk.6
The SYNTAX study, in its subanalysis, found more discrepant results, as it mentioned dyslipidemias as the only clinical variable associated with IMR, together with angiographic characteristics such as chronic occlusions, severe tortuosity, presence of multiple stenoses in the same target vessel, and right coronary artery interventions. Because it is a comparative clinical trial with surgery, it also identified patients with higher surgical risk by the EuroSCORE as more likely to have IMR.7
Thus, our results show similarities and differences in comparison with other recent contributions that analyzed the same theme.6,7 Undoubtedly, the fact that the present study did not have exclusion criteria makes these cases much more comprehensive and representative of the real world with respect to patients included in randomized studies, which always have strict inclusion/exclusion criteria, to a greater or lesser degree.6,7
It is worthwhile to provide more details regarding these findings, as there appears to be coherent explanations for what was observed, in addition to the fact that clear interdependence between some of the factors was found.
Older patients tend to have more comorbidities, such as chronic renal failure and lower level of physical activity in their daily lives, as well as more vessels with more extensive calcification and a higher percentage of chronic occlusions.10,11 Furthermore, in very debilitated patients and at the same time, very symptomatic ones, the isolated treatment of the stenosis apparently responsible for symptoms is usually chosen, aiming to improve quality of life over event-free survival. The latter situation is one of the few in which the choice of IMR is always preferred.10
Systemic arterial hypertension and chronic renal dysfunction coexist in many cases, as the first condition is a major predisposing factor for the second.12,13 In patients with chronic renal failure, the cardiologist faces a dilemma: if CMR is indicated, there must be a greater exposure to renal function impairment, which may, in severe cases of contrast-induced nephropathy, result in temporary or permanent dialysis, morbidities that are potentially very detrimental to the quality of life and for survival itself. Thus, in these situations, smaller branches or chronically occluded vessels are not commonly revascularized, resulting in IMR.1,11 Additionally, especially in cases submitted to dialysis, there is a greater chance of angiographic/clinical restenosis, which is also associated with a higher probability of incomplete revascularization, especially if it is not possible to implant drug-eluting stents.11
Individuals who were previously submitted to coronary artery bypass surgery tend to have more diffuse and complex coronary artery disease, both in the native vessels and in saphenous venous grafts. Chronic occlusions with unfavorable anatomy for PCI are commonly observed in these cases one of the most common causes of IMR. Moreover, many of target lesions located in saphenous venous grafts occur in very deteriorated vessels, preventing or hindering the performance of PCI, which often results in procedural failure.1,14
PCI in ACS patients is also associated with IMR.1,5,6 In these circumstances, many interventionists choose to treat initially only the culprit lesion, identified by several details. Many of the interventions are carried out as ad hoc procedures, with revascularization complementation depending on several factors, such as distal stenosis severity, symptom recurrence, and extension of the residual ischemia, which can be measured invasively or non-invasively.1,5,6 The patient's overall condition and any present comorbidities also influence subsequent therapeutic decisions. Logistic details, such as the patient's failure to return to undergo additional procedures, may also occur. Recently, the results of the PRAMI (Preventive Angioplasty in Acute Myocardial Infarction) study,5 which compared the isolated treatment of the culprit lesion with the preventive treatment of other significant large vessels, provided new data to help therapeutic decision-making. During the 2-year follow-up, there were significant reductions in acute myocardial infarction (68% reduction) and refractory angina (65% reduction), with a non-significant trend in mortality reduction (68% lower) in the preventive PCI group, confirming the clinical relevance of CMR, whenever feasible.
Finally, the availability of drug-eluting stents also plays a significant role in this context. These devices are definitively associated with lower rates of angiographic/clinical restenosis, and their positive impact is even more pronounced in those more likely to recur. Thus, in a situation of probable restenosis, such as a hypothetical case of a diabetic patient with a long lesion in a small-caliber vessel, the absence of these stents would almost certainly be accompanied by IMR. These statements can be demonstrated by the results of a large meta-analysis involving more than 270,000 patients published in 2009, in which the use of drug-eluting stents in a real-world scenario was accompanied by significant reductions in mortality, myocardial infarction, and additional revascularizations in late follow-up.14–16
LimitationsThe following limitations should be mentioned: (1) as the authors chose the angiographic criteria to define IMR, the observed results should not be extrapolated to situations that use other definitions, as differences could be observed in the same assessed population; (2) as the analysis included only cases of multivessel PCI, involving interventions in multiple vessels, the same care discriminated in the previous item should be taken into account for situations of IMR in cases undergoing PCI for the treatment of a single vessel – something common in clinical practice; (3) routine quantitative angiography was not performed in patients, i.e., the classification of the revascularization degree was based on the visual criteria for assessing target lesion severity, which is more inaccurate and may have influenced some of the observed results; (4) the sample size may have prevented the identification of other factors that could be associated with IMR, such as diabetes, a condition that usually causes severe and diffuse coronary disease, common characteristics in IMR situations;17 (5) as not all causes of PCI failure were clearly depicted in the database, situations such as exaggerated tortuosity and others, potentially able to predispose to IMR, could not be precisely assessed; (6) the lack of results of late clinical outcome prevented the analysis of the clinical benefit, possibly very significant, of CMR compared to IMR.
ConclusionsThis observational trial conducted at a tertiary center with a large flow of patients, involving percutaneous coronary intervention for multivessel treatment in a real-world scenario, found that incomplete myocardial revascularization occurred in approximately one of every three treated patients. The main factors significantly associated with this condition were higher-risk clinical profile and target-lesion interventions commonly associated with lower procedure success (venous grafts and chronic occlusions), and lower availability of drug-eluting stents. Finally, it was observed that the degree of revascularization achieved did not have an impact on in-hospital outcomes.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.