Chiari malformation is a structural defect in the skull that causes part of the brain to push into the spinal canal. Chiari malformations are almost always present at birth, though symptoms may not develop until later in childhood. In adult years, problems can include persistent headaches, neck pain, and weakness and/or numbness and tingling in the arms and legs, which makes it a disease of interest to present as a clinical case with a nursing model care plan.
CaseThis is a 43-year-old female patient with type I Chiari malformation. She has neck and shoulder pain, stiffness in the hands, as well as hypotonus and hypotrophy in the upper limb. The patient underwent foramen magnum decompression surgery.
Care plansWe used Roy's adaptation model for the nursing care plan. The main needs we find are respiration (risk for ineffective breathing pattern), mobility (impaired physical mobility), sensation (acute pain), protection (risk for infection, and risk for bleeding), fluid and electrolyte (risk of fluid and electrolyte imbalance), and self-concept (anxiety).
ConclusionThe Roy's adaptation model approach was useful in this case as it focuses on the patient's adaptability and is suitable for use in perioperative nursing management of type I Chiari malformation in adults. A collaborative approach is essential for planning and carrying out care.
La malformación de Chiari es un defecto estructural en el cráneo que hace que parte del cerebro empuje hacia el canal espinal. Las malformaciones de Chiari casi siempre están presentes al nacer, aunque es posible que los síntomas no se desarrollen hasta más tarde en la infancia. En la edad adulta, los problemas pueden incluir dolores de cabeza persistentes, dolor de cuello y debilidad y/o entumecimiento y hormigueo en brazos y piernas, lo que la convierte en una enfermedad de interés para presentar como caso clínico con un plan de cuidados modelo de enfermería.
CasoSe trata de una paciente de 43 años con malformación de Chiari tipo I. Experimenta dolor de cuello y hombros, rigidez en las manos, así como hipotonía e hipotrofia en el miembro superior. La paciente fue sometida a una cirugía de descompresión del foramen magnum.
Plan de cuidadosUsamos el plan de cuidados de enfermería del Modelo de Adaptación de Roy. Las principales necesidades que encontramos son respiración (riesgo de patrón respiratorio ineficaz), movilidad (movilidad física alterada), sensación (dolor agudo), protección (riesgo de infección y riesgo de hemorragia), líquidos y electrolitos (riesgo de desequilibrio de líquidos y electrolitos) y autoconcepto (ansiedad).
ConclusiónEl enfoque del Modelo de Adaptación de Roy fue útil en este caso, ya que se centra en la adaptabilidad del paciente adecuada para su uso en el manejo perioperatorio de enfermería de la malformación de Chiari tipo I en adultos. Un enfoque colaborativo es esencial para planificar y llevar a cabo la atención.
Chiari malformation is defined as a group of various anatomic abnormalities in the rhombencephalon (hindbrain), due to imperfections in the structural arrangement of the posterior fossa which cause a portion of the cerebellum to descend inferiorly through the foramen magnum.1 The incidence of Chiari malformation in adults is around 1 per 1000 births with a prevalence of more frequent events in women.2 The majority of patients feel headaches or dysesthesia in the occipital region which is potentially caused by changes in cerebrospinal fluid flow (CSF), non-radicular pain in the back, shoulders, legs, motor, and sensory symptoms, and stiffness.3
The management of Chiari malformation in adults is surgery (posterior fossa decompression, craniocervical decompression, or hindbrain decompression).3 Management of surgery must be compulsive and involves multi professions to obtain optimal results and minimize postoperative complications in patients. The nursing care process is an approach undertaken by nurses to provide nursing services that can describe competencies and professional performance. The nursing process consists of assessment, formulation of diagnosis, planning, implementation, and evaluation which can be applied with models based on nursing theory.
Roy's adaptation model looks at human experiences and responses that reflect all responses of the human adaptation system that includes capacities, assets, knowledge, skills, abilities, and commitment to enable comprehensive data collection that covers all aspects of the patient.4 This case study discusses the nursing perioperative management of type I Chiari malformation in adult using The Roy adaptation model.
Description of the caseThe 43-year-old male patient experienced the type I Chiari malformation patient with syringomyelia. She was admitted to the referral national hospital in Indonesia on January 10, 2021. The patient complained that both hands felt stiff from the shoulder to the fingers 8 years ago. At that time, the patient underwent cervical MRI with the result that there was a collection of fluid in the spine so surgery was recommended, but the patient was pregnant and refused surgery. The patient came back to the hospital about two months ago. The patient was treated in the neurosurgical ward during preoperative and on the second-day after foramen magnum decompression. After 5 days she was discharged, having recovered her former functional state and mobilization.
Nursing assessmentAccording to the Callista Roy model, the patient has the following behavior and stimulus assessment:
- 1.
Physiological adaptation modes
- a.
Oxygenation and circulation: The results of the physical examination obtained data, the blood pressure 124/70mmHg, heart rate 80bpm, temperature 36.3°C, respiratory rate 15bpm, with capillary refilling time 2s. The patient underwent foramen magnum decompression surgery, postoperatively the patient was treated in the ICU Room and the second day returned to the neurosurgery ward. The patient is fitted with a soft collar neck with nasal oxygen cannulas 3l/min. Blood pressure 118/75mmHg, heart rate 98bpm, temperature 36.5°C, respiratory rate 16bpm, oxygen saturation 98%.
- b.
Nutrition: Adaptive. The physical assessment was not stomatitis, lip mucosa was moist, swallowing reflex was not good, the conjunctiva was not anemic, teeth were clean, sclera was not jaundiced, bowel sounds were heard in 4 quadrants with a frequency of 8 times/min, no ascites, body mass index was 23.1.
- c.
Elimination: Adaptive. Spontaneous urination and bowel movements, diuresis 0.6cc/kgBW/h.
- d.
Activity and rest: The patient has decreased muscle strength in both upper limbs.
- e.
Protection: There is a surgical wound on the back of the cervical closed collar neck which is connected to the drain with minimal blood production.
- f.
Sensation: During a preoperative nursing assessment, the patient complained that both hands were stiff, the right hand could not grasp the object, felt pain, and aches in the neck to the shoulder. In the postoperative phase, the patient complained of pain in the surgical wound with Visual Analog Scale 4.
- g.
Fluid and electrolyte: The patient has an acid-base balance (hypokalemia) with a potassium value of 3.1mequiv., fluid balance +150cc.
- h.
Neurological function: In neurological assessment, the patient was compos mentis, have a good memory, good language skills, good orientation to people, place, and time, good cranial nerve examination results, 3mm/3mm isochoric pupils. Localist status is obtained by the wrist and fingers are stiff (spastic), limited right-hand supination. MRI results of whole spine contrast obtained by shifting the cerebellum tonsils and medulla oblongata inferiorly through the foramen magnum in accordance with Chiari 1 malformation with syringomyelia C2-T11.
- i.
Endocrine function: Adaptive. There is no previous history of diabetes mellitus, blood sugar at 107g/dl.
- a.
- 2.
Self-concept adaptation mode
In assessing the self-concept mode, the patient says that she is worried about the surgery.
From the assessments, we identified the following nursing diagnoses by NANDA5:
- •
Respiration: 00032 – Risk for ineffective breathing pattern related to impairment of innervation of diaphragm (lesions at or above C2-T11).
- •
Mobility: 00085 – Impaired physical mobility related to neuromuscular impairment.
- •
Sensation: 00133 – Acute pain related to physical injury.
- •
Protection: 00004 – Risk for infection related to the use of invasive devices. 00126 – Risk for bleeding to the use of invasive devices.
- •
Fluid and electrolyte: 00195 – Risk of electrolyte imbalance related to active fluid loss (diuresis, abnormal drainage or bleeding).
- •
Self-concept: 00146 – Anxiety related to situational and maturational crises.
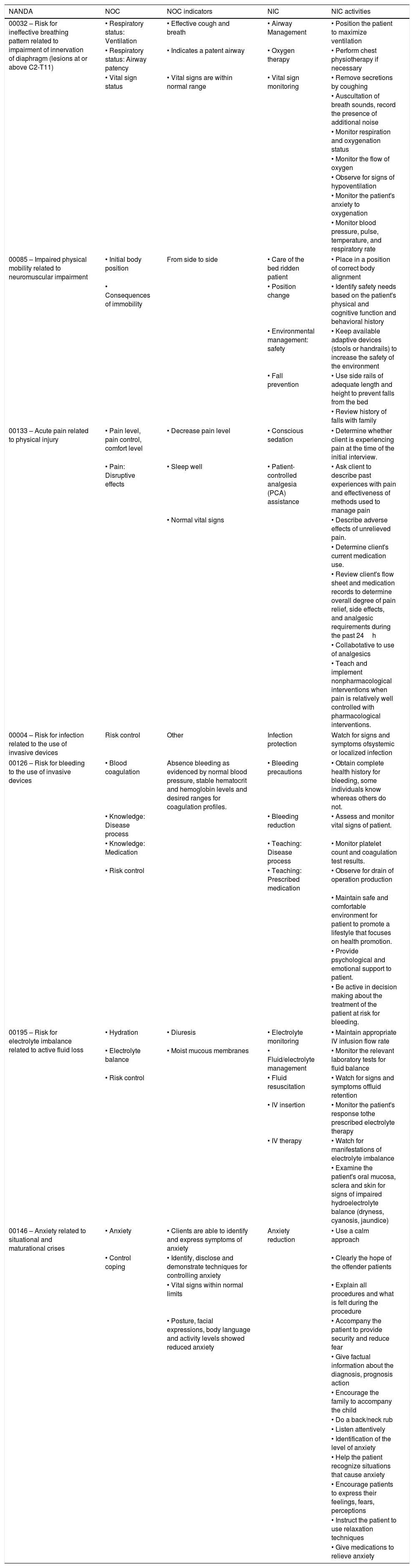
Based on the nursing diagnoses identified, the NOC and NIC, patterns that were most appropriate for the patient's situation were chosen, and they were used to create a care plan (Table 1). Preoperative nursing diagnoses include chronic pain, electrolyte balance disorders, and anxiety. Nursing interventions provided are pain management, hypokalemia management, and anxiety management based on the Nursing Intervention Classification. Collaborative intervention by giving medication 3× 500mg paracetamol and 3× 500mg KSR orally. Shortly before surgery, the patient is adaptive with the pain he feels, no longer feels anxious, and the potassium value shows 3.5mequiv.
Nurse assessment of the Chiari malformation patient according to the NANDA, NOC and NIC taxonomies.
| NANDA | NOC | NOC indicators | NIC | NIC activities |
|---|---|---|---|---|
| 00032 – Risk for ineffective breathing pattern related to impairment of innervation of diaphragm (lesions at or above C2-T11) | • Respiratory status: Ventilation | • Effective cough and breath | • Airway Management | • Position the patient to maximize ventilation |
| • Respiratory status: Airway patency | • Indicates a patent airway | • Oxygen therapy | • Perform chest physiotherapy if necessary | |
| • Vital sign status | • Vital signs are within normal range | • Vital sign monitoring | • Remove secretions by coughing | |
| • Auscultation of breath sounds, record the presence of additional noise | ||||
| • Monitor respiration and oxygenation status | ||||
| • Monitor the flow of oxygen | ||||
| • Observe for signs of hypoventilation | ||||
| • Monitor the patient's anxiety to oxygenation | ||||
| • Monitor blood pressure, pulse, temperature, and respiratory rate | ||||
| 00085 – Impaired physical mobility related to neuromuscular impairment | • Initial body position | From side to side | • Care of the bed ridden patient | • Place in a position of correct body alignment |
| • Consequences of immobility | • Position change | • Identify safety needs based on the patient's physical and cognitive function and behavioral history | ||
| • Environmental management: safety | • Keep available adaptive devices (stools or handrails) to increase the safety of the environment | |||
| • Fall prevention | • Use side rails of adequate length and height to prevent falls from the bed | |||
| • Review history of falls with family | ||||
| 00133 – Acute pain related to physical injury | • Pain level, pain control, comfort level | • Decrease pain level | • Conscious sedation | • Determine whether client is experiencing pain at the time of the initial interview. |
| • Pain: Disruptive effects | • Sleep well | • Patient-controlled analgesia (PCA) assistance | • Ask client to describe past experiences with pain and effectiveness of methods used to manage pain | |
| • Normal vital signs | • Describe adverse effects of unrelieved pain. | |||
| • Determine client's current medication use. | ||||
| • Review client's flow sheet and medication records to determine overall degree of pain relief, side effects, and analgesic requirements during the past 24h | ||||
| • Collabotative to use of analgesics | ||||
| • Teach and implement nonpharmacological interventions when pain is relatively well controlled with pharmacological interventions. | ||||
| 00004 – Risk for infection related to the use of invasive devices | Risk control | Other | Infection protection | Watch for signs and symptoms ofsystemic or localized infection |
| 00126 – Risk for bleeding to the use of invasive devices | • Blood coagulation | Absence bleeding as evidenced by normal blood pressure, stable hematocrit and hemoglobin levels and desired ranges for coagulation profiles. | • Bleeding precautions | • Obtain complete health history for bleeding, some individuals know whereas others do not. |
| • Knowledge: Disease process | • Bleeding reduction | • Assess and monitor vital signs of patient. | ||
| • Knowledge: Medication | • Teaching: Disease process | • Monitor platelet count and coagulation test results. | ||
| • Risk control | • Teaching: Prescribed medication | • Observe for drain of operation production | ||
| • Maintain safe and comfortable environment for patient to promote a lifestyle that focuses on health promotion. | ||||
| • Provide psychological and emotional support to patient. | ||||
| • Be active in decision making about the treatment of the patient at risk for bleeding. | ||||
| 00195 – Risk for electrolyte imbalance related to active fluid loss | • Hydration | • Diuresis | • Electrolyte monitoring | • Maintain appropriate IV infusion flow rate |
| • Electrolyte balance | • Moist mucous membranes | • Fluid/electrolyte management | • Monitor the relevant laboratory tests for fluid balance | |
| • Risk control | • Fluid resuscitation | • Watch for signs and symptoms offluid retention | ||
| • IV insertion | • Monitor the patient's response tothe prescribed electrolyte therapy | |||
| • IV therapy | • Watch for manifestations of electrolyte imbalance | |||
| • Examine the patient's oral mucosa, sclera and skin for signs of impaired hydroelectrolyte balance (dryness, cyanosis, jaundice) | ||||
| 00146 – Anxiety related to situational and maturational crises | • Anxiety | • Clients are able to identify and express symptoms of anxiety | Anxiety reduction | • Use a calm approach |
| • Control coping | • Identify, disclose and demonstrate techniques for controlling anxiety | • Clearly the hope of the offender patients | ||
| • Vital signs within normal limits | • Explain all procedures and what is felt during the procedure | |||
| • Posture, facial expressions, body language and activity levels showed reduced anxiety | • Accompany the patient to provide security and reduce fear | |||
| • Give factual information about the diagnosis, prognosis action | ||||
| • Encourage the family to accompany the child | ||||
| • Do a back/neck rub | ||||
| • Listen attentively | ||||
| • Identification of the level of anxiety | ||||
| • Help the patient recognize situations that cause anxiety | ||||
| • Encourage patients to express their feelings, fears, perceptions | ||||
| • Instruct the patient to use relaxation techniques | ||||
| • Give medications to relieve anxiety | ||||
The patient underwent foramen magnum decompression surgery, postoperatively the patient was treated in the ICU Room and the second day returned to the neurosurgery ward. On the second postoperative day, nurses emphasize respiratory management by observing the patient's respiratory status and positioning the patient in the supine position, pain management, fluid and electrolyte management by observing fluid intake, output and balance, and management of surgical wounds by observing signs of bleeding, signs – CSF leak signs, and signs of infection in the surgical wound.
Assessment of resultsWith planned nursing care, we were able to keep the patient free of postoperative complications. Patients were treated for 5 days postoperatively with gradual mobilization. When returning home, patients have not used oxygen and a collar neck. The patient has begun to sit, no shortness of breath, no signs of bleeding, no CSF leak, and infection in the wound. Patients are also adaptive to pain in the surgical wound by applying deep breathing relaxation techniques.
DiscussionPatients have 8 years of experienced type I Chiari malformation with clinical manifestations of neck and shoulder pain and stiffness in the upper limb. As a result, the patient experiences hypotonus-hypotrophy in the upper limb with decreased muscle strength. This condition is related to syrinx-related/spinal cord syndromes that occur in patients with Chiari malformation, causing loss of motor and sensory abilities especially in the hands.6
Patients experience syringomyelia on cervical 2 to thoracal 11. In the case of syringomyelia with spinal cord compression from syrinx, the symptoms can include numbness, muscle weakness, pain, stiffness, unusual sensations (burning, tingling), sensation changes (loss of pain or temperature sensitivity) and bladder and bowel problems. Patients in this case study experienced neck and shoulder pain. Kahn et al. (2015) state that patients with type 1 Chiari malformation with headaches often have an abnormal narrow space behind the tonsils where the flow of CSF is getting stressed over time.7 Pain that radiates to the neck and shoulders is considered part of an intense occipital headache.
Perioperative nursing management consists of preoperative, intraoperative, and postoperative management. However, in this article, nursing care focuses only on the preoperative and postoperative phases in the neurosurgical ward. The approach to patient nursing care uses Roy's adaptation model approach. Nurses play a role in providing nursing care by focusing on the patient's adaptability. Nurses try to improve and maintain the patient's coping mechanism to adapt to the stimulus that occurs. Nursing interventions carried out in the preoperative phase focus on pain management and anxiety and collaboration in balancing electrolyte levels (potassium). In anxiety conditions there will be inflammatory mechanisms, endothelial dysfunction, platelet dysfunction, and autonomic dysfunction which can make intraoperative complications.8
In the postoperative phase, nurses emphasize respiratory management by observing the patient's respiratory status and placing the patient in the supine position, pain management, fluid, and electrolyte management by monitoring intake, output, and balance fluid. Observation of the patient's breathing status is mainly done while the patient is sleeping because patients with type I Chiari malformation disorders have a higher prevalence of sleep-related respiratory disorders than those observed in the general population.9 The disorder that occurs is central sleep apnoea syndrome where the patient stops breathing temporarily or his breathing attempts go down for more than 10s. In this patient, sleep-related respiratory disorders do not occur. Postoperative nursing management in Chiari malformation patients aims to minimize the incidence of complications caused by surgery and anesthesia.10 Based on international data, 6.8% of Chiari malformation patients require repeat surgery, and 9.3% experience readmission within 30 days postoperatively with the most common cause being CSF leak.11 So it is very important to do surgical wound management by observing the signs of bleeding, signs of CSF leakage, and signs of infection in the surgical wound.
ConclusionRoy's adaptation model approach was useful in this case as it focuses on the patient's adaptability suitable for use in the nursing perioperative management of type I Chiari malformation in adults. Nursing interventions carried out in the preoperative phase focus on pain management and anxiety and collaboration in balancing electrolyte levels (potassium). In the postoperative phase, nursing interventions aim to minimize the complications and incidence of readmissions so that nurses place more emphasis on respiratory management by inspecting the patient's respiratory status and positioning the patient in the supine position, pain management, fluid, and electrolyte management by observing fluid intake, output and balance. Besides, surgical wound management is performed by observing the signs of bleeding, signs of CSF leakage, and signs of infection in the surgical wound.
Conflict of interestsThe authors declare that they have no conflict of interests.