Chronic back pain is one of the principal causes of long term disability in middle age. Its consequences include decreased worker productivity and increased costs for affected individuals, their employers and society in general.
ObjectiveDetermine coping strategies, characteristics of pain including psychological aspects, and quality of life in patients with chronic back pain.
Materials and methods50 patients from three institutions providing physiotherapy services in the city of Sincelejo, were surveyed. A non-experimental descriptive cross type design was used; each participant underwent treatment with a pain characteristic assessment interview, along with the visual analog scale (VAS), the Coping Strategies Questionnaire (QSC) and the Quality of Life Questionnaire Euroqol (EQ5D2).
ResultsMost patients had a diagnosis of cervicalgia and low back pain. The perceived intensity of pain was generally moderate. The most frequently used coping strategies was praying and hoping and the least used was catastrophizing. Patients reported a high level of quality of life in terms of self-care and mobility scales. In addition, statistically significant relationships between current pain intensity and coping strategy to ignore it (positive) and between duration of pain and the coping strategy consistent of minimizing pain (negative) were established.
ConclusionsThe findings suggest that the use of strategies to ignore the pain increases with the intensity of the pain and reduces with longer duration. Additionally, pain perception is sensitive to age and experiences.
El dolor de espalda crónico es una de las principales causas de discapacidad a largo plazo en la edad madura. Sus consecuencias incluyen: disminución de la productividad laboral y el aumento en los costos para los individuos afectados, sus empleadores y la sociedad en general.
ObjetivoDeterminar las estrategias para afrontar el dolor, características de éste, incluyendo aspectos psicológicos y calidad de vida en pacientes con dolor de espalda crónico.
Materiales y métodosSe encuestaron 50 pacientes de tres instituciones que prestan servicios de fisioterapia en la ciudad de Sincelejo. Se utilizó un diseño no experimental, descriptivo transversal. A cada participante se le hizo una entrevista de evaluación de las características del dolor junto con la Escala Analógica Visual (VAS), el Cuestionario de Estrategias de Afrontamiento del Dolor (QSC) y el Cuestionario de Calidad de Vida Euroqol (EQ5D2).
ResultadosLa mayoría de los pacientes presentaron un diagnóstico de lumbalgia y cervicalgia. En general su percepción de dolor era moderado. Las estrategias de afrontamiento más utilizadas eran rezar y tener esperanza, mientras que la menos usada era la catastrofización. Los pacientes reportaron un buen nivel de calidad de vida en las escalas de cuidado personal y movilidad. Además, se establecieron relaciones estadísticamente significativas entre la intensidad del dolor actual y la estrategia de afrontamiento de ignorar el dolor (positiva) y entre la duración del dolor y la capacidad para afrontarlo basada en minimizar el dolor (negativa).
ConclusionesLos hallazgos sugieren que el uso de estrategias para ignorar el dolor se incrementa con la intensidad del mismo y disminuye en a medida que se prolonga en el tiempo. Adicionalmente, la percepción del dolor es sensible a la edad y a las experiencias.
Low back pain represents the major musculoskeletal occupational hazard. It is the leading cause of disability in men of working age, involving labor problems, such as withdrawal from work, job loss and economic uncertainty. The total cost in lost productivity is enormous; it is the second health-related issue causing absenteeism from work (15%), after the common cold.1–3 Although we found no publications on recent data in Colombia, in the U.S. low back pain affects 31 million people per year and its annual cost to health services range from 20 to 50 billion dollars; 80% of this population has suffered from low back pain at some point in their life.4
The study of pain requires a comprehensive analysis of etiological factors; it is a perceptual and affective experience influenced by biological, psychological and socio-cultural factors that interact with each other.5 Chronic back pain is associated with psychological distress, emotional reactions – such as depressive symptoms, anxiety or anger – and inadequate cognitive processes including interpretations and beliefs about pain, poor perception of control over situations and inadequate styles of coping.6 Cognitive factors frequently associated with pain, act in its chronification process, such as the assigned meaning to pain, irrational beliefs, negative thoughts, the degree of perceived control, self-efficacy expectations, pain attention pattern, perceived social support, importance given to fear of pain, previously experienced episodes of pain and coping strategies.7
Coping strategies are a set of cognitive and behavioral efforts individuals use to confront excessive demands, according to a self-assessment of the available personal resources – which may be adaptive or not – depending on the context and appropriate assessment to change the situation.8,9 Lazarus and Folkman8 classified the coping strategies in two groups, problem-focused and emotion-focused. These involve strategies aimed to solve, re-conceptualize or minimize the effects of a stressful situation; they involve actions such as defining the problem, finding alternative solutions, evaluating the cost and benefit of such alternatives, their choice and implementation.3,10,11 Emotion-focused coping strategies regulate the subject's emotional response to the event and minimizes the degree of emotional disturbance. Examples of these are: positive thinking, denial, avoidance, selective attention, distancing, minimization and wresting positive value from negative events.10–12 Cognitive strategies include: diverting attention, reinterpreting pain sensations, self-affirmation, ignoring pain, praying or hoping and catastrophizing.13 In the latter, patients tend to evaluate pain as uncontrollable, exaggerate its threat value and cannot divert attention away from it.2,4 Behavioral strategies increase activity and pain behaviors while involving relevant aspects in chronic pain, such as control over it and the ability to minimize it.14,15
The purpose of the study was to investigate aspects of pain including psychological and behavioral aspects, and assess the subjective pain intensity. Additionally, this study aims to identify effects of chronic back pain on patients’ daily living, personal, work and social activities, as well as the impact on their health and administration of a specific treatment. these elements are associated with the health-related quality of life concept (HRQOL).11 Health-related quality of life (HRQOL) refers to the value given by individuals to their lives in terms of some physical, psychological and social aspects; these components are influenced by their experiences, beliefs, expectations and perceptions. HRQOL involves aspects such as economic resources, autonomy and environmental characteristics, which determine health adversely; however, they are often disregarded by doctors and researchers.16
Materials and methodsParticipantsThe total population subject of study is made up of 225 patients treated during July and August 2011 recruited in three physiotherapy centers belonging to a health-care institution in the city of Sincelejo (Colombia). A sample of 50 patients, mostly women (72%), was taken from the total population; the age of participants ranges from 18–75 years old (nearly 60% of participants are aged 35–64 years), selected through an intentional or non-probability sampling of cases diagnosed with chronic back pain with a minimum duration of six months, who voluntarily signed the informed consent to participate in the research. A total of 66% of the sample are employed, 20% unemployed, 12% self-employed and 2% are retired. Patients with cognitive deficit and poor reading comprehension level were excluded from the study. This research was approved by the ethics committee and the research Corporacion Universitaria Antonio Jose de Sucre (RAD No. 4472). The most important recommendation suggested was fulfilled and refer patients at risk of suicide, to be anxious or depressed mental health care box immediately, and inform the treating physician. Written informed consent was obtained from each participant after a full explanation of the study.
InstrumentsTo measure chronic back pain, coping strategies and quality of life variables needed to meet the purpose of the investigation, four instruments were applied: a semi-structured chronic pain assessment interview, the visual analog scale (VAS), the Coping Strategies Questionnaire (CSQ) and the Quality of Life Scale EuroQol (EQ5D2).
The Chronic Pain Assessment Interview was designed by Benítez and Pájaro (2006) and is intended to ascertain aspects of pain, such as causes, location, radiation, intensity, frequency, duration, further information on treatments used to manage pain (results obtained from each of them), its emotional impact on the individual, level of interference in the patient's daily life, ideas associated with pain and the patient's physiological reactions to pain.17
The visual analog scale (VAS) consists of a 10cm line (3.9 inches) where the patient must mark the maximum, minimum and current intensity of experienced pain; it is useful to assess the subjective pain intensity.18
The Coping Strategies Questionnaire (CSQ) was developed by Rosenstiel and Keefe.13 With Cronbach's alpha ranging between 0.71 and 0.85, it assesses coping strategies through 48 items grouped into 8 scales: diverting attention from pain, self-affirmations, praying and hoping, increasing behavioral activity, reinterpreting pain sensations, ignoring pain, catastrophizing and pain behaviors. Two items related to control exercised over pain and ability to minimize it are also included.
EuroQol (EQ5D2) is an instrument designed by Brooks et al.19 to characterize a group or population's quality of life. Its test–retest reliability ranges between 0.86 and 0.90 and has a checked validity.19 Moreover, the EuroQol has a good correlation with the SF-36, excluding the “psychological functional status” area. It consists of a five-scale self-administered section (mobility, self-care, daily living activities, pain/discomfort and anxiety/depression) and a visual analog scale on health.20
ProcedureThis study was carried out through three phases. In the first one, a thorough literature review on the topic was necessary in order to select the instruments. In the second one, these instruments were applied to the sample and a subsequent data collection took place. All data collection was completed by the first author, who is experience in clinical psychology and familiar with local culture. Finally, in the third phase, a statistical processing of the results and analysis of the information obtained from the theoretical basis was performed. Our analyses included tabulation of response frequencies and correlations between selected questions and demographic and clinical variables. Specifically, Spearman correlation analysis was conducted in SPSS Statistics 23 (IBM Corp., Chicago, IL, USA).
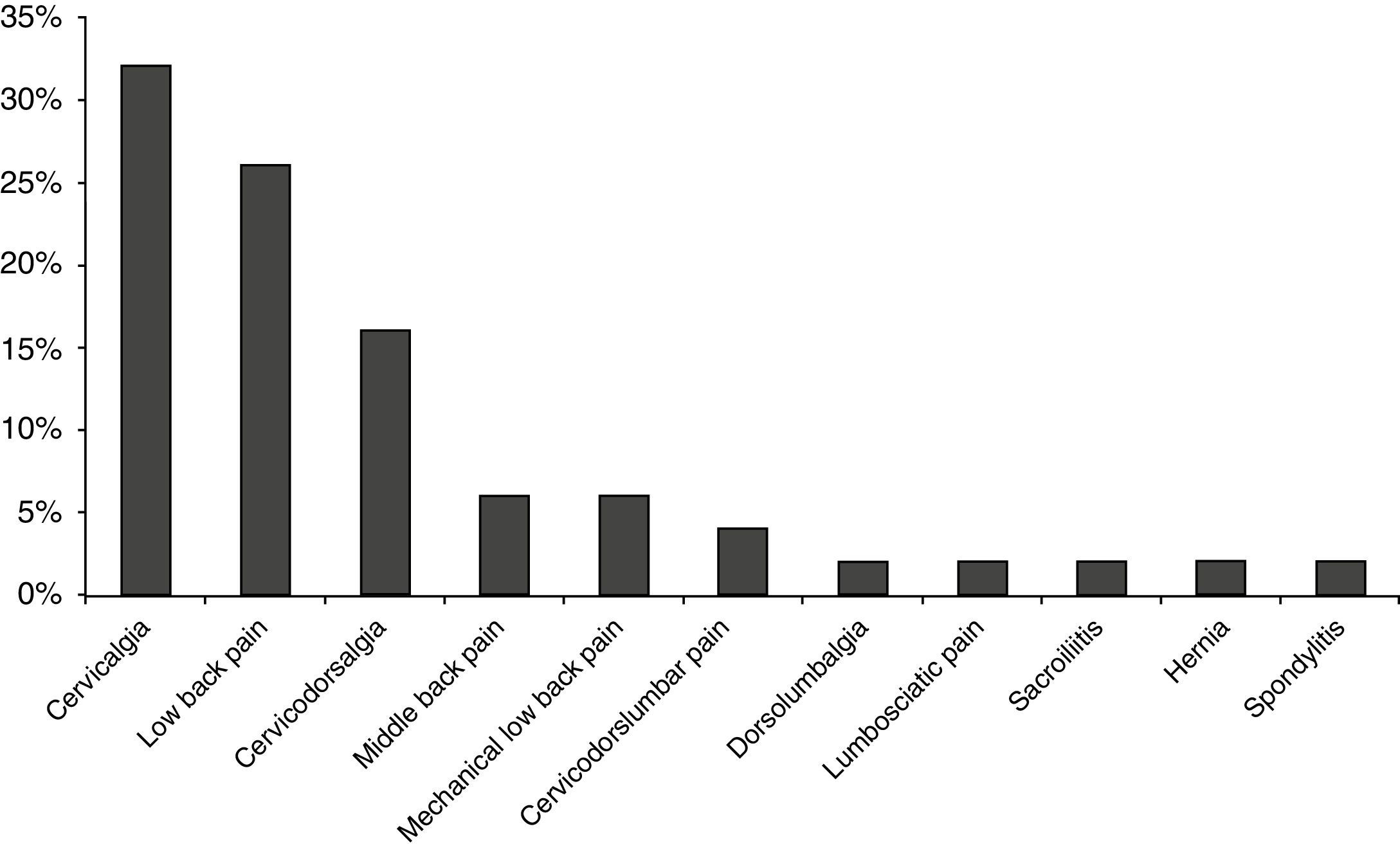
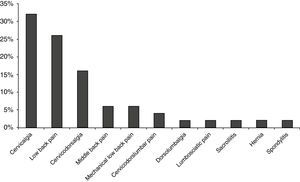
ResultsDescriptive analysisLeading chronic back pain types in patients was cervicalgia – neck pain (32%) followed by low back pain (26%) (see Fig. 1).
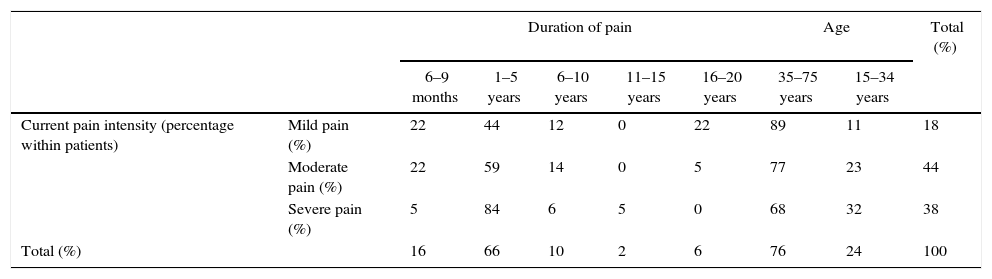
Table 1 shows the relation between current pain intensity and the time elapsed since the patients’ first episode. 82% of the patients experienced moderate–severe pain intensity, and 66% reported a pain duration between 1 and 5 years regardless of the pain severity.
Relationship between current pain intensity, time elapsed since patients’ first episode, and age.
| Duration of pain | Age | Total (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 6–9 months | 1–5 years | 6–10 years | 11–15 years | 16–20 years | 35–75 years | 15–34 years | |||
| Current pain intensity (percentage within patients) | Mild pain (%) | 22 | 44 | 12 | 0 | 22 | 89 | 11 | 18 |
| Moderate pain (%) | 22 | 59 | 14 | 0 | 5 | 77 | 23 | 44 | |
| Severe pain (%) | 5 | 84 | 6 | 5 | 0 | 68 | 32 | 38 | |
| Total (%) | 16 | 66 | 10 | 2 | 6 | 76 | 24 | 100 | |
Source: Authors.
According to the previous types of treatments received by patients to relieve their pain, physical therapy is the coping strategy with the highest frequency of use (48.2%), followed by drugs (38.8%), no treatment (7.1%) and others as psychological treatment, X-rays, acupuncture, infiltrations and chiropractic (11.3%).
Concerning behavioral characteristics toward pain, the leading behavior is complaining (37.5%), followed by sighing (25%) as well as physiological changes experienced because of pain. On the other hand, blood pressure increase or decrease (27.3%) and sweating (22.7%) were reported to a greater extent. Ultimately, the most affected activities by pain, are sleep (27%) and work (22.1%).
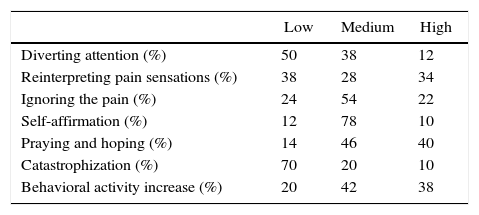
Table 2 outlines praying and hoping of pain as the most frequently used coping strategy by patients (40%) and catastrophization as the least used one (70%).
Frequency of coping strategies used by patients.
| Low | Medium | High | |
|---|---|---|---|
| Diverting attention (%) | 50 | 38 | 12 |
| Reinterpreting pain sensations (%) | 38 | 28 | 34 |
| Ignoring the pain (%) | 24 | 54 | 22 |
| Self-affirmation (%) | 12 | 78 | 10 |
| Praying and hoping (%) | 14 | 46 | 40 |
| Catastrophization (%) | 70 | 20 | 10 |
| Behavioral activity increase (%) | 20 | 42 | 38 |
Source: Authors.
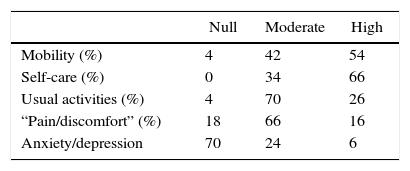
Regarding patients’ perception of pain control, 78% report having some, 16% report having full control and 6% report not having any. About their perceived ability to minimize pain, 64% may do so slightly, 20% report minimizing it to a total extent and 16% are not able to do so. The prevalence for quality of life dimensions are presented in Table 3.
According to the assessment of perceived general health status, patients claim that their current health status compared to the one they had for the previous 12 months is better (68%), equal (28%) and worse (4%). Also, current health status is perceived as fair (42%), good (34%) and bad (24%).
Correlation analysisIn the correlation analysis of the variables, a significant relationship between duration of pain and coping strategy to minimize it was found (r=−0.373, P-value=0.008). This relationship is negative suggesting that a longer duration of pain means that less coping strategies are used to minimize it. Besides, a significant association between current pain intensity and ignoring pain was displayed (r=0.360, P-value=0.010). This relationship is positive giving further evidence that the higher the current pain intensity the more coping strategies to ignore it are used.
Discussion and conclusionsThis research was aimed to determine coping strategies and quality of life characteristics in patients suffering from chronic back pain; in order to do so, a descriptive correlational nonparametric analysis was used, taking into account that these variables are relevant to the quality of life in terms of occupational health. In this sense, different studies have stressed the importance of behavioral and psychological variables as factors influencing chronic pain.13,15
Low back pain is one of the biggest complaints in outpatient, resulting in disability and decreased quality of life.21 Low back pain was the second most common pain in this study (26%); for these patients, multidisciplinary and multimodal treatments are recommended.22 However, some studies indicate that patients report obtaining greater pain relief through physical therapy, in contrast to other interventional therapies.21
Self-efficacy expectations play a crucial role in the experience of chronic pain.23–26 In relation to the perception of pain control, 6% of the sample perceived a lack of control compared to 78% who experience some. Regarding perceived ability to minimize pain, only 16% of the sample perceive not being able to do so, suggesting that the majority of participants show high self-efficacy in relation to their experience of pain, have resources and high perceived control and ability to cope with it, using these skills to guarantee a good degree of general adaptation to coping.
Following the same descriptive sense, in relation to age, we found that the largest proportion of participants’ ages range between 35 and 75 years old were overrepresented in all pain severity categories. Previous literature has confirmed that that suffering and pain are prevalent in elderly populations.18,27,28 Some authors indicate that subjects experience changes in pain perception or sensitivity as they age, such as decreased pain sensitivity over time.20 Their findings are consistent with data from this study, since a lower proportion of participants aged 35–75 reported moderate pain (77%) than severe pain (68%). By contrast, Fordyce29 argues that older patients complain more of pain than younger ones, while other studies suggest that pain complaints are based on the tendency to report pain instead of sensitivity to its perception.30–32
With respect to coping strategies, catastrophizing was the least used by patients, indicating that they do not have a catastrophic vision regarding their pain and do not perceive it as an uncontrollable or threatening event – usually associated with good prognosis on their condition.33 Conversely, self-affirmations, praying or hoping followed by an increased behavioral activity were commonly reported by participants with a medium and high frequency.
Positive self-affirmation is a cognitive coping strategy aimed at reducing the degree of emotional reaction through positive thinking and wresting positive value from negative events.11,12,14 It is a cognitive strategy, since the subject accepts personal responsibility and experiences pain as a means of personal growth.14
In the analysis of the relationship among research variables, a significant correlation was found between current pain intensity and the coping strategy of ignoring pain (however, there was no relationship with the other coping strategies). This is consistent with similar findings where pain avoidance and cognitions are significantly associated with higher pain intensity in low back pain patients; those who experience increasing pain intensity increase the use of ignoring pain strategy.34
In emotion-focused ignoring pain strategy, the individual makes an effort to control the negative emotional response related to pain.10–12 For this reason, it is considered an evasive strategy, since it aims to avoid the problem or negative emotions it entails.
A negative correlation was also observed between duration of pain and minimizing the pain coping strategy; however, no relationship was found between its duration and the other coping strategies. Most participants had endured pain for a moderate period of time (5 years max.); at the same time, they report being able to minimize pain. In other words, the shorter the duration of pain, the higher their perceived ability to minimize it.35
This can probably be explained by the fact that if patients have endured pain for a short period of time, they will have higher self-efficacy expectations about their own skills and resources to cope, which they will try to implement in order to eliminate pain. However, as time passes and pain is still present, they perceive these skills are not as effective, changing their perception of control over pain. In this sense, Rotter35 explains that patients with higher perceived control will report lower levels of pain intensity. Perceived uncontrollability leads to thoughts of uselessness and helplessness against pain, triggering negative emotions.36,37 Soucase et al.28 also suggest that patients tend to express their emotions during the initial stage of the disease, but subsequently repress them and the threat assessment along with a pessimistic expectation of pain relief in the short term, predicts difficulties in their emotional health through a high anxiety level.
In contrast to other studies,2,28,32 the intensity and duration of pain, have no significant correlation to the quality of life, suggesting that suffering from chronic back pain is not a decisive factor that affects quality of life. In general, it is essential to recognize pain as a complex experience in which molecular, cellular, physiological, biological, psychological and social factors interact; as a consequence, it is impossible to establish definitive criteria for evaluating pain and how this can affect people's quality of life.18
Ultimately, Zarazaga et al.30 explain that despite experiencing pain, coping strategies determine the patient's state of mind and ability to perform everyday tasks. However, there seems to be some independence between these three variables so that, for example, a patient may have a high pain intensity, good performance and positive state of mind, depending on the way he/she has assessed pain and his/her use of coping strategies.
Although this study provides new information of remote communities, some important limitations should be discussed. First, self-report measures could be affected by recalling issues or socially desirable responses. There is a need for the implementation of objective measures. Second, participation in this study was voluntary which might has created selection bias. Future research would benefit from the use of a larger and more diverse sample. Third, the pain circumstances included in this study are not comprehensive. Therefore, future studies should include more psychosocial, cognitive and environmental variables associated with pain and people's functioning from a multidimensional perspective, in order to have a better understanding and explanation of chronic back pain determinants. To achieve this, a biopsychosocial approach that integrates various disciplines in the health care system, is required. Additionally, emerging techniques in the management of cronic pain should be explored (e.g. neurostimulation38 and opioids39).
Ethical disclosuresProtection of human and animal subjectsThe authors state that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and agreement with the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors state that they have followed the protocols of its work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document work in the power of the correspondence author.
FundingAuthors did not receive any funding.
Conflict of interestNeither I nor any of the authors of this manuscript have any financial conflict of interest pertaining to the work developed.
Article translated by Monica Martinez Cudriz, Master's degree in Translation and Intercultural Studies, Universidad de Sevilla, Spain.
Please cite this article as: Mercedes Bello-Villanueva A, Benítez-Lara M, Oviedo-Trespalacios O. Características del dolor, aspectos psicológicos, calidad de vida y estrategias de afrontamiento en pacientes con dolor de espalda crónico en una ciudad de Colombia. Rev Colomb Anestesiol. 2017;45:310–316.