Management of chronic pain by conventional means is usually insufficient, but the enhanced knowledge of the neurobiology of pain has led to the development of new treatments like spinal neurostimulation, with optimal short- and long-term results.
ObjectivesTo integrate and update clinical practice guidelines on the effectiveness and safety of spinal neurostimulation in the management of chronic pain.
Materials and methodsSearch of practice guidelines, systematic reviews and clinical trials in the main databases (Cochrane, EMBASE, LILACS and MEDLINE), and assessment of their quality and level of evidence in order to propose recommendations for the management of chronic painful syndromes and cardiac and lower-limb ischemia.
ResultsSufficient evidence was found to support the use of spinal neurostimulation for pain relief in cases of persistent pain after back surgery and also for complex regional pain syndrome. Growing evidence was found for the use of spinal neurostimulation in refractory angina pectoris and in painful ischemic lower limbs.
ConclusionsNeurostimulation is a minimally invasive technique useful for the management of persistent pain after back surgery and for complex regional pain syndrome.
El manejo del dolor crónico por medios convencionales a menudo es insuficiente, es por eso que con el mayor conocimiento de la neurobiología del dolor se han desarrollado nuevos tratamientos como la neuroestimulación espinal, con resultados óptimos a corto y largo plazo por parte de los médicos tratantes.
ObjetivosIntegrar y actualizar guías de práctica clínica sobre la efectividad y seguridad de la neuroestimulación espinal en el manejo del dolor crónico.
Materiales y métodosSe realizó una búsqueda de guías de práctica, revisiones sistemáticas y ensayos clínicos en las principales bases de datos (Cochrane, EMBASE, LILACS y MEDLINE) evaluando su calidad y grado de evidencia para proponer recomendaciones en el manejo de síndromes dolorosos crónicos, y en isquemia cardiaca y de miembros inferiores.
ResultadosSe encontró evidencia suficiente para soportar el uso de la neuroestimulación espinal para el alivio del dolor que persiste después de cirugía de espalda y también para síndrome doloroso regional complejo. Se encontró evidencia en ascenso para el uso en angina de pecho refractaria y en extremidad inferior isquémica dolorosa.
ConclusionesLa neuroestimulación es una técnica mínimamente invasiva útil para el manejo de dolor persistente posterior a cirugía de columna y para síndrome regional complejo.
Chronic pain is a world pandemic. As such, it is a public health problem with emotional repercussions for the patient, and repercussions for the family, the workplace, society, and the economy. Multidisciplinary teams have been set up to develop research programs and education in pharmacology and minimally invasive techniques to meet the needs of the affected patients.1–4
According to the 2014 survey by the Colombian Association for the Study of Pain (ACED), the prevalence of chronic pain in the Colombian population is 47%,5 an alarming figure when compared with the 15–50% range reported in the world, with a mean of 25% according to the International Association for the Study of Pain (IASP), and of 19% for Europe.3,6–8
Among Europeans, 38% perceive that traditional medical therapy is insufficient for controlling pain.6 Moreover, the Pain in Europe survey reports that patients have experienced pain for an average of seven years and almost 20% have had pain for 20 years.7 Disability and loss of work is around 20%.8
Chronic pain accounts for 53% of all causes of total absence from work, 18% of absolute disability, and 15% of temporary absences from work.9 The Colombian 2014 pain survey shows that 32% of the respondents have been absent from work because of pain, and the prevalence of pain in the emergency services is 27.5%, and 72.5% in outpatient clinics.5
The goal of treatment in chronic pain is to increase tolerability and improve quality of life.9–12 The mainstay of physical pain management has been pharmacological therapy. However, invasive techniques such as neurostimulation – introduced more than 40 years ago – have become more relevant in recent years. Neurostimulation is based on principles of electrical stimulation, magnetic stimulation and radiofrequency, and it is used mainly when there is no response to conventional therapies.11–13
This paper is the result of a search in the literature of the best evidence supporting the use of neurostimulation, together with the experience of Colombian experts who have indicated and implanted neurostimulators, and who have long-term follow-up of their patients.
Materials and methodsWith the aim of updating and adapting the international guidelines, experts on the subject (clinical and methodological) were identified in the country. As a group, they held five teleconferences and two on-site meetings to discuss the findings in the literature and make a correlation with their practice in order to arrive at a consensus. Initially, they identified the Clinical Practice Guidelines (CPG) on the topic of neurostimulation using the Tripdatabase meta-search engine. Then, in order to identify articles not included in the existing guidelines, a non-systematic search was conducted in the Cochrane, EMBASE, LILACS and MEDLINE databases using as search descriptors the terms “failed back surgery syndrome” AND “spinal cord stimulation”; “complex regional pain syndrome” AND “spinal cord stimulation”; “pain in refractory angina” AND “spinal cord stimulation” AND chronic ischemic lower extremity pain AND “spinal cord stimulation”. When the strategy yielded too many retrieved articles, the Systematic Review OR Meta-analysis OR Randomized Clinical Trials filters were used. In some painful syndromes, due to the small number of articles retrieved, no limits or filters were applied to the search. The search was limited by year of publication (2000–2014), but not so by language and/or abstracts.
CPGs were assessed by three independent reviewers using the AGREE-II tool, in order to arrive at global quality score.14 This tool also provides a methodological strategy for guideline development. It consists of a form divided into six domains with 23 questions, followed by two global score forms. Each question is assessed on a Linkert scale from 1 to 7. It has not established minimum scores or score patterns between domains to differentiate between high- and low-quality guidelines. After completing the 23 items, the AGREE-II users must perform two global assessments of the guidelines that require the user to judge the quality of the guideline taking into consideration the criteria applied during the evaluation process. The user is also asked whether he/she would recommend the use of the guideline.14 The GRADE tool was used for systematic reviews (SR) of the literature and individual studies;15 this tool is a system for classifying the quality of the evidence and rating the strength of the recommendations. First, it categorizes the outcomes of interest and their relative importance; then it evaluates the quality of the evidence according to four categories for each of the outcomes in order to obtain a global quality of the evidence; and finally it rates the strength of the recommendations under two categories only: strong or weak recommendations.15
Results and discussionIndications for spinal neurostimulationIn clinical trials on pain, a relief of more than 50% is considered a satisfactory response. The most recent guidelines of the European Federation of Neurological Societies (EFNS),13 found that only 30–40% of the patients with neuropathic pain show good response to medications.13,16. Hence, spinal neurostimulation emerges as an option in the following cases:10–13
Persitent pain following spine surgery.
Complex regional pain syndrome.
Refractory angina pectoris pain.
Vascular ischemic pain.
A rational selection of patients increases the possibility of success. We suggest the following criteria:
Absence of response to conventional treatments.
A cause of pain that is not amenable to surgical correction.
Pain of less than 6 months of duration.
Preferably non-malignant neuropathic pain.
A history of minimal spine interventions.
Psychological/psychiatric assessment to rule out a primary emotional disorder as a cause of pain.
Absence of lawsuit circumstances or potential secondary gain.
A transient implantation period is suggested in order to assess response, before final implantation, except in angina pectoris patients in whom the definitive technique may be used right away. Coverage of the painful area with paresthesia is mandatory.9–13
Patients diagnosed with chronic painful syndromes with the following characteristics must not be included:11–13
Spinal malformation preventing electrode implantation in the epidural space.
Clotting disorders.
No response to prior neurostimulation.
Pending surgery.
Inadequate family environment.
Inability to grasp how the system works.
Local infection close to the implantation site.
The electrodes are placed percutaneously or through minor laminectomy in the posterior epidural space. In all, 4–16 electrodes are placed: four for unilateral pain and 8–16 in bilateral pain. The space selected must correspond to the entry area of the compromised roots of the painful territory.9–13
A trial period of 3–7 days with external stimulation is required in order to determine the correct placement of the electrodes and to avoid definitive implantation in patients who would not tolerate stimulation. Close to 30% of the trials are negative.9
Technical advances in new devices and techniques have helped overcome the limitation of stimulating multiple dermatomes and succeed in accessing regions like the occiput and the sacral region to provide a favorable treatment option.9–13
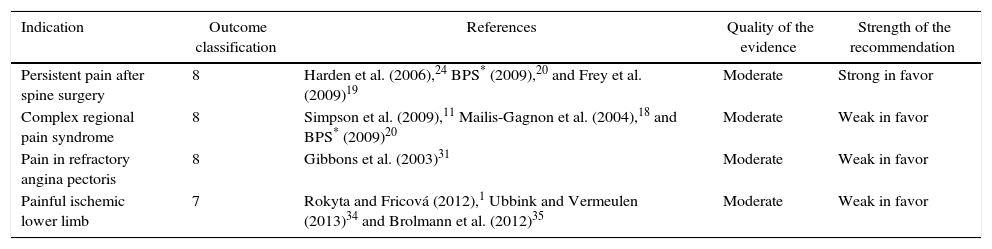
Table 1 shows the results of the review of the literature used as a basis to prepare this proposal.
Grading of the evidence for the outcomes evaluated in this adaptation of the guidelines.
| Indication | Outcome classification | References | Quality of the evidence | Strength of the recommendation |
|---|---|---|---|---|
| Persistent pain after spine surgery | 8 | Harden et al. (2006),24 BPS* (2009),20 and Frey et al. (2009)19 | Moderate | Strong in favor |
| Complex regional pain syndrome | 8 | Simpson et al. (2009),11 Mailis-Gagnon et al. (2004),18 and BPS* (2009)20 | Moderate | Weak in favor |
| Pain in refractory angina pectoris | 8 | Gibbons et al. (2003)31 | Moderate | Weak in favor |
| Painful ischemic lower limb | 7 | Rokyta and Fricová (2012),1 Ubbink and Vermeulen (2013)34 and Brolmann et al. (2012)35 | Moderate | Weak in favor |
BPS: British Pain Society.
Classification of the outcome of interest: 1–2 not important, 4–6 important, 7–9 key.
Quality of the evidence: high, moderate, low, very low (CPG, CT, observational).
Strength of the recommendation: strong, weak (very favorable risk-benefit balance, no conclusive proof of the effects of the intervention).
Source: Authors.
Persistent pain after spine surgery (PPSS) is defined as lumbar or radicular pain that persists or becomes established after spine surgery.16 PPSS has increased proportionately with the number of surgeries performed. It is more frequent after fusion surgery (stabilization) and affects 10–40% of all patients.17
Results of the searchOverall, 29 articles were identified; of those, six were SRs that answer the question asked, the first in 200418 and the most recent one of 2009.19 Four out of six SRs were published before 2007 and included the same randomized clinical trial containing a preliminary report and two additional publications with a longer follow-up.20,21 The search yielded 14 references that could correspond to clinical trials.22 Unfortunately, there was only one cost-effectiveness study based on the clinical trial (CT) published previously by Kumar.23 Additionally, two on-going protocols were identified17,18 with no result reported to date. No new CTs other than these reported by systematic review were identified.
EvaluationThe AGREE-II was used for CPGs. In the assessment, the NICE guideline11 was given an average score in all domains and, specifically in the methodological rigor domain, the score was 6/7. The score for the British Pain Society (BPS) guideline20 was 5/7 in the methodological rigor domain. The SR by Frey19 was evaluated using the GRADE system to generate the evidence table and the quality of the evidence was rated as moderate.
The CPGs evaluated the recommendation on the use of spinal neurostimulation in PPSS. Both guidelines are consistent: The NICE guideline assesses the use of neurostimulation in patients with neuropathic pain or pain of ischemic origin and recommends it in adults of neuropathic pain of any origin, including PPSS, except in ischemic pain. The BPS guideline20 also recommends neurostimulation in patients with chronic pain due to PPSS. The two guidelines include only two relevant CTs on the research question.19,20
The six SRs support the use of neurostimulation in patients with PPSS, although they recommend that further clinical trials should be conducted. The systematic review by Frey et al. published in 2009 only included articles published in English, including the CT by Kumar and North,22,23 and also included 10 observational studies. The outcomes assessed were pain improvement, functional assessment and others such as psychological improvement, return to work, use of analgesics and cost-effectiveness. The conclusion of this review is that there is evidence supporting the recommendation to use spinal neurostimulation (SN) in patients with short-term (less than 12 months) and long-term (more than 12 months) PPSS. Satisfaction is consistently in favor of the use of neurostimulation. The same review assesses quality according to the methodology described by Koes et al.25 with a score of 55/100 for the study by Kumar23 and of 56/100 for the study by North.22
The clinical trial by Kumar23 included adults with radicular pain over 50/100, lasting at least 6 months after surgery for disc hernia correction. The primary outcome was the proportion of patients with more than a 50% improvement of their leg pain after 6 months. Secondary outcomes included back pain and leg pain improvement, quality of life and functional performance, use of analgesia, satisfaction with treatment, and adverse effects. Overall, 100 patients were included, 52 in the neurostimulation group and 48 in the control group. Baseline characteristics were similar, except for mean back pain, which was higher in the neurostimulation group (p=0.03). The primary outcome was more frequent in the neurostimulation group (48%) than in the control group (9%), p<0.001. Differences in favor of neurostimulation were also found in levels of back pain (p=0.008), leg pain (p<0.001), in seven dimensions of quality of life, and in satisfaction (p<0.001). At 12 months, the primary outcome was 34% vs. 7%, p=0.005. Reported complications were electrode migration (10%), infection (8%), and loss of the paresthesia (7%).
A 24-month follow-up was reported by the authors in a new comparison called “illustrative”, probably because of losses to follow-up. The results favor the intervention (37% vs. 2%), p=0.003. Other positive outcomes included leg pain, quality of life and the Oswestry disability index.
The clinical trial by North22 compared NS versus reoperation, with a 2-year follow-up. This trial included 50 adults who received the treatment. After 6 months of follow-up, the study authorized a change: 54% of the patients assigned to reintervention switched to the treatment with spinal cord stimulation (SCS) and 21% switched to reoperation. Of the patients available for follow-up, 47% in the SCS group had a successful result with the treatment, compared with 12% in the reoperation group (p<0.01)18.
RecommendationThe evidence described supports the use of neurostimulation over conventional therapy. Published guidelines and systematic reviews recommend SCS in patients with PPSS.
In adult patients taken to spine surgery, with radicular neuropathic pain that is more severe in the legs than in the back, is of moderate intensity (>50/100) and has lasted for more than 6 months, SCS is effective during the first year (quality of evidence: moderate; grade of recommendation: weak in favor).
Complex regional pain syndromeComplex Regional Pain Syndrome (CRPS) is a regional pain disorder (with no neural or dermatome pattern) that is not proportional in terms of time, progression or severity to the usual course of the originating injury. Pain may be spontaneous or evoked by movement and is usually distal and associated with sensory, motor, vasomotor and/or trophic changes. The pathophysiology involves components of neurogenic inflammation, central sensitization, alterations of cortical representation, and autonomic changes.24,26
Results of the searchTwo guidelines that answered the clinical question – the NICE guideline11 and the BPS guideline20 – and five SRs published between 2003 and 2009 were identified. The qualitative evaluation of the systematic reviews found that they all included the same CT to answer the question of the effectiveness of NS in CRPS, and it was the clinical trial conducted in 2000 by Kemler et al.27,28 The Cochrane review18 included another trial, but with a different population (lumbar pain in failed spine surgery). All SRs, except the Cochrane review, included observational studies to support the conclusion. Finally, two additional articles were identified, corresponding to the 2- and 5-year follow-up of the Kemler trial.29,30
EvaluationThe guideline was assessed using the AGREE-II. The NICE guideline11 was given an average evaluation in all domains, and specifically for the methodological rigor domain, the score was 6/7. The BPS guideline20 was given a score of 27 in the methodological rigor domain. The Cochrane systematic review is a high-quality review according to SIGN (Scottish Intercollegiate Guidelines Network). The SIGN assessment of the CT by Kemler, present in all the systematic reviews, was acceptable. Finally, the Cochrane systematic review and the individual RCTs were evaluated using the GRADE system, and the quality of the evidence for the articles included was moderate.
RecommendationsBased on the evidence and bearing in mind the follow-up between 6 months and 5 years, the conclusion is that in adults with a diagnosis of CRPS and no adequate response to conventional treatment (physical therapy, sympathetic block, transcutaneous electrical stimulation and analgesic medication), NS plus physical therapy is effective for pain relief for a period of up to 2 years. It is not possible to arrive at a conclusion regarding the impact of the intervention in terms of quality of life and functional recovery. (Quality of the evidence, moderate; grade of recommendation, strong in favor.) Unfortunately, the benefits do not persist at 5 years of treatment with SCS.28–30 (Quality of the evidence, moderate; grade of recommendation, weak in favor.)
Pain in refractory angina pectorisPain in refractory angina pectoris is defined as ischemic cardiogenic pain, exacerbated by exercise, in patients with proven coronary heart disease and who are not candidates for coronary by-pass because of their clinical and anatomic characteristics.31
Results of the searchTwo references were identified, one of which is a clinical practice guideline and the other a narrative review.31,32
AssessmentThe clinical practice guideline was assessed using the AGREE-II tool and was given a global score of 5/7, while the narrative review was assessed using the GRADE methodology, resulting in a moderate rating for evidence and a weak recommendation in favor.
RecommendationAccording to the two references identified, the conclusion is that NS may be an option for pain management in refractory angina pectoris when more conventional options have been discarded, with a moderate quality of evidence and weak recommendation in favor.
Painful ischemic lower limbThe painful ischemic lower limb is defined as ischemic vascular pain at rest, exacerbated by exercise, with evidence of severe vascular flow abnormality.25,33
Results of the searchBoth the guidelines as well as the published reviews agree on the heterogeneity of the studies and the lack of methodological rigor when it comes to assessing the efficacy of SCS versus conventional medical management in terms of quality of life, mortality, rate of amputation, use of analgesia, and cost-effectiveness. Despite the fact the there are studies dating from before 2003, they were not included because of methodological deficiencies. After 2003, two consensus guidelines1,34 and one systematic review have been published.35
AssessmentThe AGREE-II tool was used to assess the guidelines, resulting in a global rating of 5/7, while the systematic review was assessed using the grade methodology, resulting in a moderate rating for the evidence and a weak recommendation in favor.
RecommendationAt the present time, there is a weak evidence supporting the benefit of NS therapy in cases of painful ischemic lower limb. In patients with vascular pain limb the recommendation is to make an adequate selection when applying the NE therapy or when there is the a greater or lesser risk of limb amputation. The therapy is potentially useful in the following cases:
- -
When there are no more therapeutic options for pain relief.
- -
Patients with optimal therapeutic response to SCS during a trial period (pain and functional improvement).
- -
The decision for use must be made by a multidisciplinary team.
- -
The device is NOT free of complications and both the practitioner as well as the patient must be aware of them.
A review of the evidence was conducted on the use of NS for the treatment of chronic painful syndromes for which it may be a safe and efficacious option. The evidence is adequate for persistent pain after spine surgery and for complex regional pain syndrome. However, the evidence is weak for pain in refractory angina pectoris and in painful ischemic lower limb; therefore, in appropriately selected patients, NS is a useful and reversible treatment to treat severe chronic pain associated to diseases described here, when an initial conservative treatment has shown to be ineffective.
Conflict of interestThe authors declare not having conflicts of interest that might compete with the objective of this review, and not having received honorarium for participating in the preparation of these guidelines, except for only one author, Luis Fernando Cifuentes, an employee of Boston Scientific Colombia. However, this author did not participate in recommendations in which he had any conflict of interest.
FundingThe financial support for the preparation of the guideline was an unconstrained contribution from Boston Scientific Colombia.
Please cite this article as: Griego JM, Gómez MP, Gomezese OF, Cadavid AM, Yepes CJ, Mayungo T, et al. Adaptación colombiana de las guías de neuroestimulación espinal en el manejo del dolor crónico e isquémico. Rev Colomb Anestesiol. 2016;44:334–340.