Chronic pain is a highly prevalent condition and its treatment includes multiple measures, including ultrasound-guided analgesic blocks. There are no reports available including different types of blocks in chronic pain patients.
ObjectiveTo determine the clinical efficacy and safety of ultrasound-guided interventional management in chronic pain patients that consulted at Instituto Colombiano del Dolor in 2011.
Materials and methodsDescriptive follow-up trial of a cohort of 149 chronic pain patients undergoing ultrasound-guided interventional therapy at Instituto Colombiano del Dolor in Medellín city, from May through December 2011. Data were collected prior to the procedure, at day two and then one month later. Pain intensity was measured with the visual analog scale.
Results149 patients were analyzed. The most common block was the supra-scapular nerve. The efficacy of the blocks was 79.2% and 38.9% after two days and one month, respectively, with a statistically significant difference between the intensity of the initial pain and pain at follow-up. The incidence of complications was low. There were no differences in the outcomes between the patients with a diagnosis of fibromyalgia and those who had not been receiving any prior pharmacological therapy.
ConclusionsUltrasound-guided interventional pain management is an effective and safe technique.
El dolor crónico es una enfermedad de alta prevalencia, su tratamiento incluye múltiples medidas, entre ellas los bloqueos analgésicos guiados por ultrasonido, no existen reportes que incluyan diferentes tipos de bloqueos en pacientes con dolor crónico.
ObjetivoDeterminar la eficacia clínica y seguridad del manejo intervencionista guiado por ultrasonografía en pacientes con dolor crónico atendidos en el Instituto Colombiano del Dolor durante el año 2011.
Materiales y métodosEstudio de tipo descriptivo de seguimiento a una cohorte de 149 pacientes con dolor crónico sometidos a tratamiento intervencionista guiado por ultrasonografía en el Instituto Colombiano del Dolor en la ciudad de Medellín entre los meses de mayo y diciembre del año 2011. Se obtuvieron datos antes del procedimiento, a los dos días y un mes después. La intensidad del dolor se midió con la escala visual análoga.
ResultadosSe analizaron 149 pacientes, el bloqueo más frecuente fue del nervio supraescapular. La eficacia de los bloqueos fue del 79,2% y 38,9% a los dos días y al mes respectivamente, con una diferencia estadísticamente significativa entre la intensidad del dolor inicial y el de los seguimientos. La incidencia de complicaciones fue baja. No hubo diferencias en los resultados finales entre los pacientes con diagnóstico de fibromialgia y en quienes no venían recibiendo tratamiento farmacológico previo.
ConclusionesEl manejo intervencionista del dolor guiado por ultrasonografía es una técnica eficaz y segura.
Pain is a frequent cause of visits to the doctor and there is an increasing need to provide optimal and safe treatment. The use of ultrasonography in interventional analgesia has become increasingly relevant for pain management in the last 10 years.1
Ultrasound guidance improves the safety of regional anesthesia because it reduces the volume of the local anesthetic agent required and hence lowers the incidence of systemic toxicity, shortens the time to perform the block, reduces the number of needle insertions and provides faster onset of action. Moreover, it reduces the risk of accidental puncture of other neighboring structures because it enables the visualization of the peripheral nerves, of the surrounding structures and the needle. The disadvantages are few but important, such as availability and the need for additional raining.2–6
There is increasing certainty about the importance of using ultrasonography in interventional analgesia to complement other more extensively used techniques – i.e. fluoroscopy – and about the need to promote ultrasound training in the anesthesia graduate programs and pain management subspecialties at various universities around the world and as a topic of general interest at international congresses.
Consequently, a trial was designed to answer the question: Is ultrasound-guided interventional management effective and safe for chronic pain patients?
Overall objectiveTo determine the clinical efficacy and safety of ultrasound-guided interventional management in chronic pain patients.
Specific objectives- •
To describe the study population in terms of the socio-demographic characteristics.
- •
To determine the major blocks performed in chronic pain patients.
- •
To identify any changes in the pain intensity as described by the patients before and after treatment.
- •
To assess the efficacy of interventional therapy in terms of pain relief.
- •
To assess the association between pain relief and sex, diagnosis of fibromyalgia and prior oral pharmacological treatments.
- •
To determine the safety of the blocks in terms of the occurrence of complications.
With the approval of the Ethics Committee, a descriptive follow-up trial of a cohort of chronic pain patients that received ultrasound-guided interventional therapy, using 0.5% bupivacaine without epinephrine plus 4mg of dexamethasone for a peripheral nerve block or an intra-articular block with 0.5% bupivacaine without epinephrine plus 40mg of methylprednisolone acetate, was undertaken. A portable General Electric LOGIQe® scanner was used, with linear transducers (7–12MHz) and convex transducers (2–5MHz). All patients were evaluated prior to the procedure and one month later. The procedures were done five to ten days following the initial evaluation. At every control the pain intensity was measured using the visual analog scale (VAS) and during the one-month follow-up visit the patients were asked about the VAS pain intensity two days after the procedure. Pain relief was defined as a drop of at least 50% in VAS. The sample was chosen from the patients that came to Instituto Colombiano del Dolor in Medellín city for pain consultation from May through December 2011 and met the inclusion and exclusion criteria. The data were collected form primary sources.
The inclusion criteria were the following:1 diagnosis of chronic pain (>6 months of evolution);2 undergoing a single peripheral nerve or intra-articular block, and3 use of ultrasonography to guide the block.
The exclusion criteria were1 indication for interventional management with multiple simultaneous blocks;2 pain management with prolotherapy, radiofrequency or ultrasound-guided trigger points;3 continued perineural infusion catheter insertion, and4 able to quantify the pain intensity.
The variables analyzed were gender – defined as phenotype, age in years at the time of the procedure; the type of procedure performed – the indication of the intervention to be made; the diagnosis of fibromyalgia present at the time of the procedure; the use of concomitant oral medicines – i.e., receiving acetaminophen in the last month –; a weak opioid; a tricyclic antidepressant and/or anti-neuropathic (pregabaline, gabapentin or carbamazepine); the pain score in terms of the subjective pain evaluation by the patient according to VAS and complications such as the occurrence of adverse events resulting from the intervention.
The database was stored in Microsoft Excel® and the software used for the analysis of the information was SPSS 18 (licensed by CES University). A descriptive analysis was completed for all the variables studied, supported by the calculation of proportions and descriptive measurements. The association between the quantitative variables and Pearson's Chi-square test was also established, in addition to a paired analysis to establish the difference between pain intensity before and after the procedure, using Wilcoxon's test. The association between pain relief with a diagnosis of fibromyalgia and the concomitant use of oral medicines was evaluated using Pearson's Chi-square test and the relative risks were calculated. A <5% statistical significance was used, with 95% confidence intervals.
ResultsA total of 426 ultrasound-guided interventional analgesic procedures were completed at Instituto Colombiano del Dolor, Medellín city, from May through December 2011. 152 patients were dismissed because they had undergone multiple procedures, 15 for radiofrequencies, 15 for prolotherapies, 46 for trigger points, 10 for perineural continuous infusion catheters and 39 because they had difficulty in quantifying pain. A total of 149 patients undergoing ultrasound-guided peripheral nerve block were analyzed.
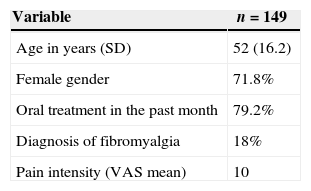
Table 1 summarizes the general characteristics of the patients evaluated. Prior oral treatment corresponds to the treatment received in the last month, with at least acetaminophen, a mild opioid, a tricyclic antidepressant and/or an anti-neuropathic drug (pregabaline, gabapentin or carbamazepine).
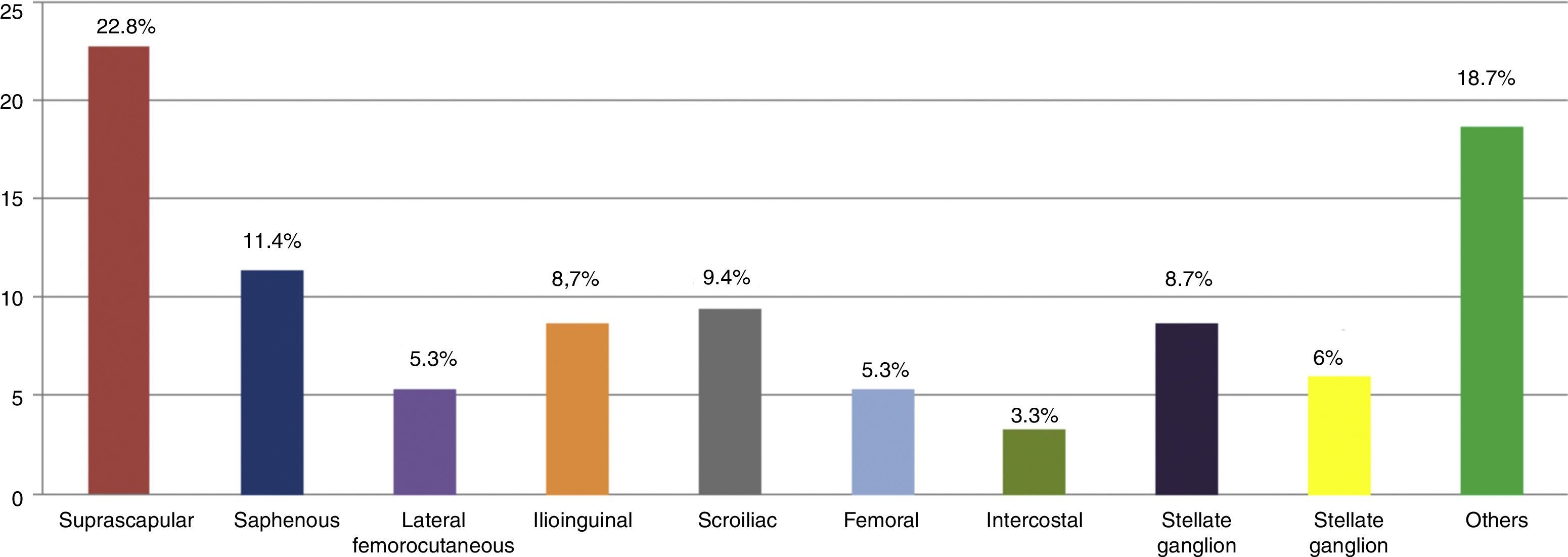
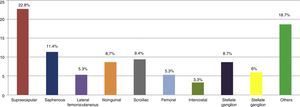
The primary block performed was the supra-scapular nerve, followed by the saphenous, the sacroiliac, the stellate ganglion, ilioinguinal, lateral femoral cutaneous and femoral. The intra-articular blocks were the knee, the shoulder, the elbow, the sacroiliac and the sternochondral joints. To a lesser extent, there were other blocks such as cervical facets, medial lumbar ramus, sciatic, obturator, posterior tibial, medial, cubital, axillary, genitofemoral, greater occipital and the rectus sheath. The most important percentages are shown on Fig. 1.
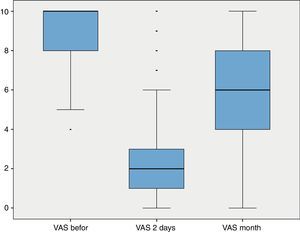
The percentage of patients that experienced pain reduction after two days and after one month of the procedure were 79.2% and 38.9%, respectively.
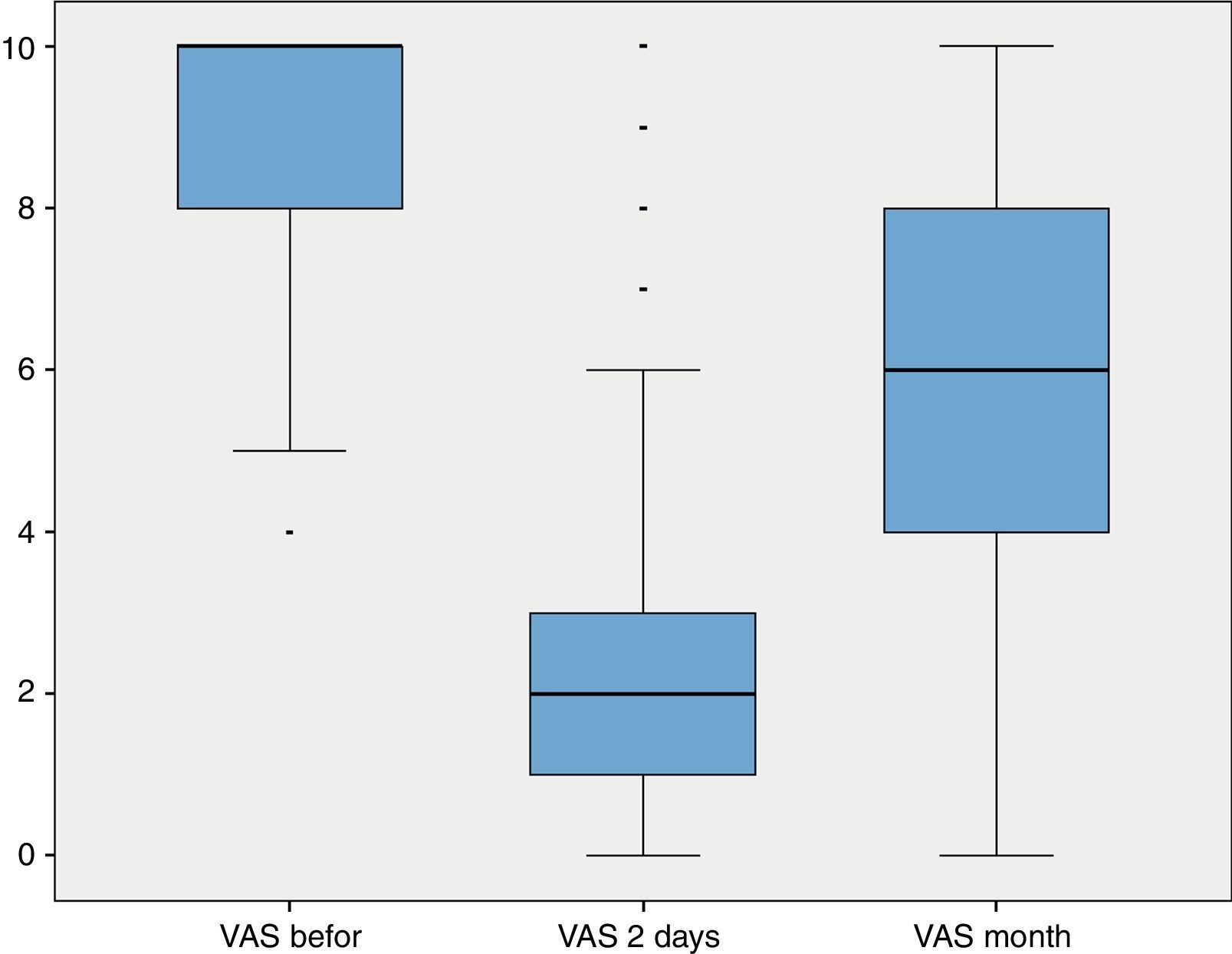
The mean VAS score on the second day and after one-month follow-up was 2 and 6, respectively. The difference between the initial VAS and the second day means was 8, a statistically significant difference (p<0.0001). Similarly, statistically significant differences were found between the initial and one-month VAS means (p<0.0001). The pain intensity after one month of the procedure was higher on the second day but it was still less than before the block (Fig. 2).
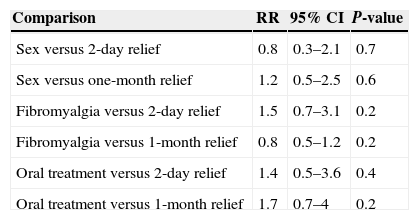
In the sub-group analysis, equal results were found in the comparison of the pain intensity among patients with fibromyalgia and those who had not been receiving pharmacological treatment. In terms of the final result after two days and after one month of the block, there was no association between gender, a diagnosis of fibromyalgia and pain relief in both evaluation periods, or with having received treatment (Table 2).
Association of sex, fibromyalgia, oral pharmacological therapy and pain relief.
| Comparison | RR | 95% CI | P-value |
|---|---|---|---|
| Sex versus 2-day relief | 0.8 | 0.3–2.1 | 0.7 |
| Sex versus one-month relief | 1.2 | 0.5–2.5 | 0.6 |
| Fibromyalgia versus 2-day relief | 1.5 | 0.7–3.1 | 0.2 |
| Fibromyalgia versus 1-month relief | 0.8 | 0.5–1.2 | 0.2 |
| Oral treatment versus 2-day relief | 1.4 | 0.5–3.6 | 0.4 |
| Oral treatment versus 1-month relief | 1.7 | 0.7–4 | 0.2 |
Source: Authors.
The incidence of complications was 2.6%, one case of intramuscular hematoma (0.6%) and three (2%) patients that fell at home on the same day of the procedure because of a lower limb motor block.
DiscussionThere are few reports on the management of benign chronic pain, whilst there are many about malignant pain and perioperative regional anesthesia. Ultrasound-guided nerve blocks have been an effective and safe tool. This trial shows that pain relief was accomplished in 79.2% of the patients two days after the procedure and in 38.9% after one month of treatment with a low incidence of complications.
The most frequent block was the supra-scapular nerve block – the most sensitive nerve of the shoulder. This approach has been effective, particularly in rheumatoid arthritis, osteoarthritis, and rotator cuff disorders, with complications such as pneumothorax, intravascular injection, residual block and local trauma.7 This trial included 34 supra-scapular blocks with a 79.4% efficacy after two days of the procedure and 35.3% after one month. There were no complications. A recent publication reported a 47.8% pain improvement in patients during the first month following the procedure.8 Harmon and Hearty9 reported a case of ultrasound-guided supra-scapular nerve block with a reduction in pain intensity and improved shoulder movement and function for 12 weeks. It is also possible to use continuous supra-scapular nerve block with a catheter,10 but this approach is beyond the scope of this trial.
The saphenous nerve is a sensitive branch of the femoral nerve; it is easy to identify and its block provides analgesia in patients with chronic knee pain. The saphenous nerve innervates an extensive skin area on the medial aspect of the knee, the leg, the ankle and the foot,11–15 in addition to improving acute postoperative pain.16,17 Tsai et al.18 reported a series of 39 cases of ultrasound-guided saphenous nerve blocks with a 77% success rate after four months; these results are similar to the results herein.
The ilioinguinal nerve block has been used to control postoperative pain mainly in inguinal herniorrhaphy in children,19 but the procedure has been extended to adult patients in whom the incidence of postoperative inguinal pain is 12%. More recently it has also been used for managing chronic central sensitization pain.20 This trial included 13 patients treated with ilioinguinal nerve block, of which after the second day only one patient continued to experience pain and after one month follow-up 61.5% were still improving.
Neck and chest blocks may have a high risk of esophageal, tracheal, and thyroid injury, intravascular or epidural injection and pneumothorax if not performed under real time visualization. Kapral et al.21 described the ultrasound-guided stellate ganglion block in 1995, while the intercostal nerve block technique was described in 2004 by Eichenberger et al.22 A high frequency transducer was used in this trial that enabled the identification of these structures and adequate positioning of the needle;23 13 stellate ganglion blocks were performed and there were no complications. Likewise, five intercostal blocks were administered with no pneumothorax reports, but there was one episode of hematoma in the dorsal paravertebral musculature reported 24h after the block, in a patient that was anti-coagulated up to five days before the procedure. The patient received medical treatment and there were no sequels later.
Intra-articular blocks are traditionally performed “blindly”, but ultrasonography is increasingly being used to be able to approach any joint.6 6% of our intra-articular blocks were in the shoulder and the knee with good results.
Due to the few chronic pain management reports, the recommendations are low evidence, except for the celiac plexus block,1 for which the ultrasound-guided technique was described in 1983.24 Cochrane published recently a systematic review4 with 18 clinical trials and 1344 acute pain patients and reported an incidence of minor complications below 10% – a higher value than the number reported in this trial with one hematoma and three falls due to residual motor block of a lower limb, following a femoral block. The risk of falling after a lower limb block is high.25 Muraskin et al.,26 reported two cases of falls following peripheral nerve blocks.
The limitations described were a short follow-up period and the possible bias of the patients’ memory when retrospectively rating pain 48h after the block.
The data contribute valuable information for the specialists in the area because of the broad range of ultrasound-guided blocks performed at a pain management referral center, with favorable and safe results. The blocks excluded from the trial are also relevant and should be the object of future research.
ConclusionsUltrasonography-guided interventional pain management is a treatment option indicated for acute or chronic pain patients. This approach does not replace fluoroscopy-guided procedures, but offers some benefits such as lower cost, no radiation exposure and a lower rate of complications. All of the above considerations make this an effective and safe choice.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNone.
Ethical disclosuresThe authors declare that they have followed the protocols of their work center on the publication of patient data Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study. Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Arcila-Lotero MA, Mejía-Aguilar MA. Eficacia y seguridad del manejo intervencionista guiado por ultrasonografía en pacientes con dolor crónico: seguimiento a una cohorte. Rev Colomb Anestesiol. 2015;43:263–268.