The painful shoulder syndrome is one of the most common chronic pain conditions of muscle-skeletal origin. It is frequent to find patients who do not improve with conservative treatment based on medications and physical therapy, or even with surgical management. Ultrasound-guided suprascapular blockade is another option when basic therapy does not work.
ObjectiveTo determine the clinical efficacy and safety of interventional management with ultrasound-guided suprascapular nerve block in patients with chronic shoulder pain.
Materials and methodsA descriptive, prospective, follow-up study was conducted in a cohort of 46 patients with chronic shoulder pain disorder who received interventional treatment under ultrasound guidance at the Colombian Pain Institute between October 2011 and May 2012, with the objective of determining efficacy and safety of the procedure. Data were gathered before the procedure, and then two days later and one month after the procedure. Pain intensity was measured using the visual analogue scale (VAS).
ResultsForty-six blocks were performed. Overall, 78.3% of the patients experienced at least 50% reduction of pain two days later, and 47.8% had pain relief after one month, with a statistically significant difference (p<0.0001) between the starting VAS median score and the median scores on the second postoperative day and at one month. There were no complications.
ConclusionsUltrasound-guided suprascapular blockade is an effective and safe treatment option in patients with chronic shoulder pain.
El síndrome de hombro doloroso es una de las patologías más comunes de dolor crónico de origen osteomuscular. Y es frecuente encontrar pacientes sin mejoría con el tratamiento conservador con terapia física y fármacos, e incluso fallo en el manejo quirúrgico. El bloqueo supraescapular guiado por ultrasonido es una alternativa cuando la terapia de base no funciona.
ObjetivoDeterminar la eficacia clínica y la seguridad del manejo intervencionista con bloqueo del nervio supraescapular guiado por ultrasonografía en pacientes con dolor crónico de hombro.
Materiales y métodosSe realizó un estudio de tipo descriptivo, prospectivo, de seguimiento a una cohorte de 46 pacientes con enfermedad dolorosa crónica de hombro que recibieron tratamiento intervencionista guiado por ultrasonografía en el Instituto Colombiano del Dolor entre los meses de octubre de 2011 y mayo de 2012, para determinar su eficacia y seguridad. Se obtuvieron datos antes del procedimiento, a los 2 días y un mes después. La intensidad de dolor se midió con la escala visual analógica (EVA).
ResultadosSe realizaron 46 bloqueos. El 78,3% de los pacientes presentaron una disminución del dolor de al menos el 50% a los 2 días y el 47,8% al mes, con una diferencia estadísticamente significativa (p < 0,0001) entre las medianas de la EVA inicial, al segundo día y al mes. No se presentaron complicaciones.
ConclusionesEl bloqueo supraescapular guiado por ultrasonografía es una opción de tratamiento eficaz y segura en pacientes con dolor crónico de hombro.
Pain is a frequent complaint and the need to provide optimal and safe treatment options is increasing. The use of ultrasound in analgesic interventional procedures has been gaining importance in the field of pain treatment over the past 10 years.1
The painful shoulder syndrome is a frequent condition among the elderly and an important cause of functional disability; its prevalence in the general population is approximately 20%.2
Suprascapular nerve block was first described in 1941 by Wertheim and Rovenstine,3 and it has been widely used since then by anesthesiologists for the management of chronic shoulder pain with good results. Conditions in which this technique has been used include adhesive capsulitis, rheumatologic disorders, arthritis, arthrosis, postoperative pain, trauma, cancer, and even in painful syndromes secondary to stroke as a complication of the hemiplegia.4,5 It is also used in other situations such as acute pain and the diagnosis of suprascapular neuropathy.6 In 2007, Harmon and Hearty had described the technique of ultrasound-guided suprascapular nerve block,7 which has improved the rate of success as well as the safety with which these procedures are performed.
With the introduction of ultrasound into the field of regional anesthesia, the efficacy and safety of analgesic blocks have been optimized. In patients with painful shoulder syndrome, the use of ultrasound has improved accuracy and allowed direct visualization of the needle and of the anatomic site where the analgesic is delivered. Likewise, it has reduced the possibility of complications such as pneumothorax, and avoided the exposure of the staff to radiation, when compared with other technologies used for performing suprascapular nerve block.6 At present there are few studies available in the literature about the use of ultrasound for suprascapular nerve blocks.
The objective of this study is to determine the clinical efficacy and safety of interventional management of chronic shoulder pain by means of ultrasound-guided suprascapular nerve block.
Materials and methodsAfter obtaining the approval of the institutional review board, we conducted an observational descriptive, prospective follow-up study in a cohort of patients with chronic painful shoulder disease who received ultrasound-guided interventional treatment by means of a suprascapular nerve block by using 8mL of 0.5% bupivacaine without epinephrine, plus dexamethasone 4mg. A General Electric LOGIQe® portable ultrasound machine with a linear transducer (7–12MHz) was used. The block was performed by using 50mm and 100mm Teflon-coated needles connected to the peripheral nerve stimulator, in order to confirm the nerve location. With the patients seated, and after cleaning the site with chlorhexidine, the skin was infiltrated with a volume of 5–7mL of 2% lidocaine without epinephrine. All the patients were assessed before the procedure and one month later. The procedures were performed five to ten days after the initial assessment. Patients were assessed for pain intensity by using the visual analogue scale (VAS) and for the one-month follow-up questions were asked also about pain intensity VAS score on the second day after the procedure. Pain relief was defined as a reduction of at least 50% on the VAS. The sample was selected from among the patients coming to the Colombian Pain Institute in Medellín, Colombia, between October 2011 and May 2012, who met the inclusion and exclusion criteria. Data were obtained from primary sources. No informed consent was required considering the observational nature of the study.
The following were the inclusion criteria: (1) a diagnosis of chronic shoulder pain (more than 6 months); (2) performance of a suprascapular nerve block; and (3) use of ultrasound guidance for the block.
The following were the exclusion criteria: (1) indication for interventional management with multiple simultaneous blocks; (2) pain management of the suprascapular nerve with prolotherapy or radiofrequency in the two preceding years; (3) insertion of perineural continuous infusion catheter; and (4) inability to quantify pain intensity.
The variables considered were gender, age, diagnosis, concomitant use of oral analgesics, diagnosis of fibromyalgia, VAS pain score, and the presence of complications.
The database was stored in Microsoft Excel® and the software used for data analysis was the SPSS 18 (CES University license). A descriptive analysis supported on proportion calculation and descriptive measures was done for all the variables studied; association between qualitative variables was established by using the Pearson Chi square test; a paired analysis was also conducted to establish the difference in pain intensity before and after the procedure using the Wilcoxon test, and a bivariate analysis was used to asses the association between pain relief and the diagnosis of fibromyalgia, and the concomitant use of oral medications. The statistical significance level used was less than 5% with 95% confidence intervals.
ResultsOverall, 46 patients treated with ultrasound-guided suprascapular nerve block were analyzed. Mean age was 55.3 (±15.5), with a proportion of 78.3% of females. Eighty-four per cent of patients had been receiving oral pharmacological treatment in the last month with at least acetaminophen, a weak opioid, a tricyclic antidepressant and/or an antineuropathic agent (pregabalin, gabapentin or carbamazepine). The majority of patients had reported severe pain before the block was performed (Table 1).
Overall characteristics of the patients studied.
| Variable | n=46 |
| Age in years (±SD) | 55.3 (15.3) |
| Female gender | 78.3% |
| Oral treatment in the past month | 84.8% |
| Pain with neuropathic characteristics | 32.6% |
| Prior shoulder surgery | 19.6% |
| Diagnosis of fibromyalgia | 21.7% |
| Severe pain (VAS ≥7) | 93.5% |
SD, standard deviation; VAS, visual analogue scale.
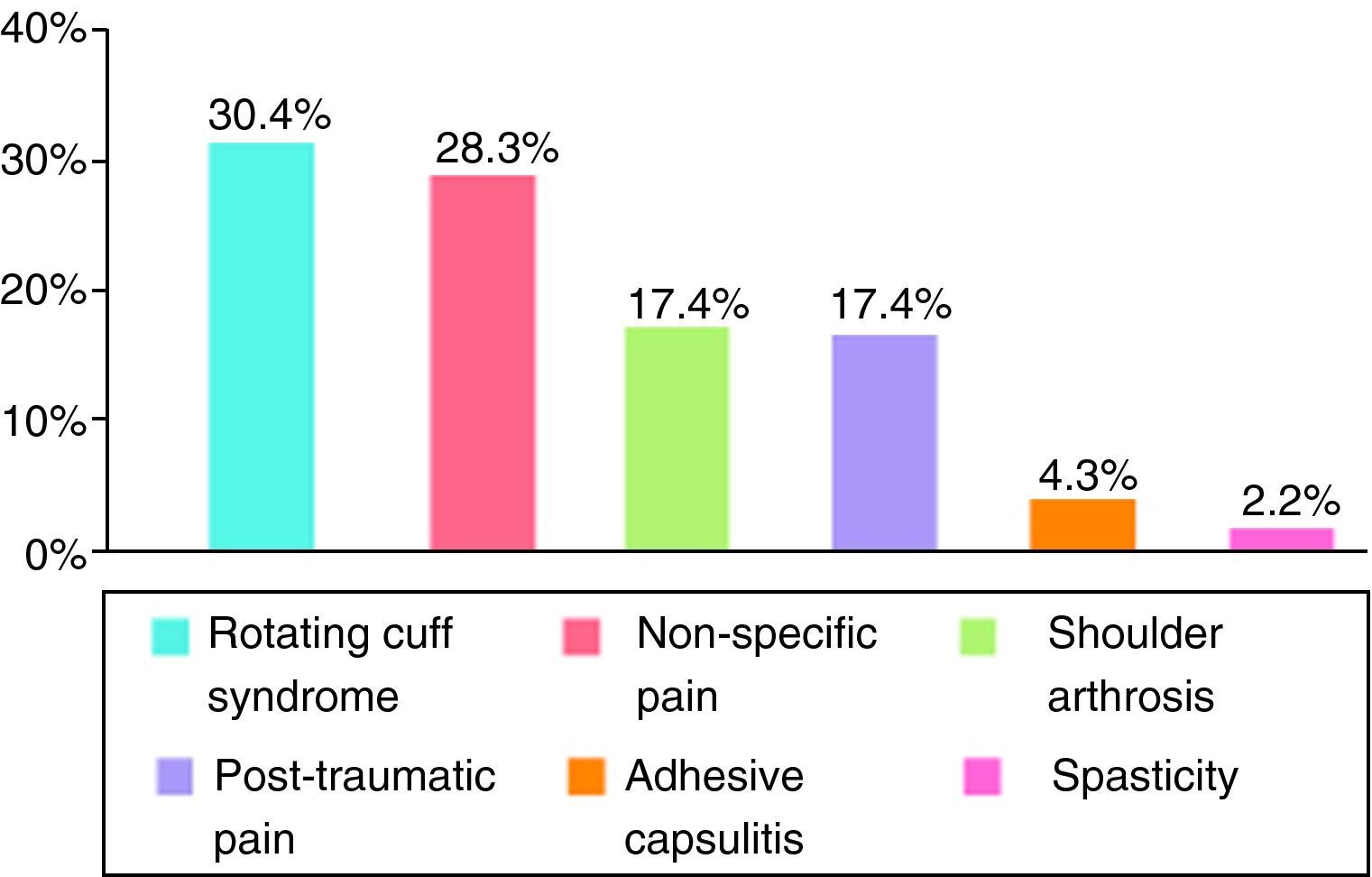
The main diagnosis was rotating cuff syndrome, followed by non-specific pain reported mainly by patients with fibromyalgia (Fig. 1).
The proportion of patients with reduced pain two days and one month after the procedure was 78.3% and 47.8%, respectively.
On the second day after the block, 70% of patients had a VAS pain score of ≤3. More than 50% of patients had mild-to-moderate pain intensity at one-month follow-up (VAS≤6). The difference between the initial VAS and the second-day VAS medians was statistically significant at 7 points (p<0.0001). Likewise, statistically significant differences were found between the initial VAS median and the one-month VAS median (p<0.0001) (Fig. 2).
Although not comparable because of the insufficient sample size between groups, patients diagnosed with fibromyalgia, those with neuropathic characteristics and those with prior surgeries had a lower analgesic response with the block. There were no gender differences, or differences among those that had been receiving prior treatment.
Finally, there were no complications.
DiscussionChronic shoulder pain originating intrinsically in the joint structures is a frequent medical complaint and a cause of functional disability. In many cases, it is difficult to treat and responds poorly to pharmacological and physical therapies, creating a progressive condition that may result in total limitation such as adhesive capsulitis. For this reason, it is important to consider interventional options, including suprascapular nerve block, when conservative therapy fails.8
Currently there are few reports in the literature regarding management of chronic benign pain, subject matter of this study, but there is a significant number of reports on malignant pain and perioperative regional anesthesia. Chronic pain has been managed by means of blockade of the involved nerves, and ultrasound has proved to be an effective and safe tool.
In the past, blockade of muscle-skeletal and perineural structures of the shoulder was done based on anatomical landmarks under no imaging guidance (“blindly”), with less than 50% effectiveness.9,10 With the advances in imaging techniques, including fluoroscopy, magnetic resonance and ultrasound, effectiveness now ranges between 27% and 100%; this wide range is explained by the variety of methods, the type of guidance used and the training of the operator. For example, there are reports of 95–100% certainty in the adequate location of shoulder structures with the help of ultrasound.11,12 Among the various imaging guidance techniques, ultrasound has benefits over fluoroscopy such as no exposure to X-rays, and the visualization of muscle and nerve structures. The advantages over magnetic resonance include lower cost of the equipment, fast real-time imaging, and even portability.13,14
The suprascapular nerve is the largest sensory nerve in the shoulder, and the technique for blocking it has been described ever since 1941, with several refinements and variations throughout the years.3 It has been used with good efficacy for the management of acute and chronic pain, particularly in rheumatoid arthritis, osteoarthritis of the glenohumeral joint and rotating cuff disorders, including frozen shoulder. Some authors have reported a few complications such as pneumothorax, intravascular injection, residual motor blockade and local trauma.15
In a systematic review, it was found that a series of three intra-articular blocks results in the improvement of pain and mobility for 16 weeks, with no additional benefit with 4 or more sessions.16
In this study, 46 ultrasound-guided suprascapular blocks were performed with an efficacy of 78.3% after two days, and 47.8% after one month, and absence of complications. Harmon and Hearty7 reported one case of ultrasound-guided suprascapular nerve block in which they found a reduction in pain intensity and improved mobility and function over a 12-week period. It is also possible to use continuous suprascapular nerve block through an in-dwelling catheter,17 but the placement of perineural catheters was not considered in this study. Suprascapular nerve block is easy to perform, results in long-term analgesia, and is a safe technique that improves shoulder pain from multiple causes.
Our data show a wide variety of indications for ultrasound-guided suprascapular blockade with favorable and safe results over a seven-month period in a reference center for pain management. Excluded blockades are also relevant and subject matter of future research, including the three-compartment blockade of the shoulder.
There were some limitations such as the short follow-up period, and potential memory bias in the retrospective classification of pain at 48h after the procedure. However, given that patients finally experienced relief after months of enduring the pain, it was easy for them to remember the improvement during those initial days. Moreover, a high proportion of patients continued to experience relief of their pain during the first month.
This study showed evidence of the value of ultrasound, hence the need to provide better training to practitioners performing analgesic interventional procedures, starting with graduate training, considering that ultrasound is an adequate option for interventional management of many painful syndromes.
ConclusionsInterventional management of shoulder pain using ultrasound-guided suprascapular nerve block is a treatment option indicated for patients who fail conservative therapy. In addition, it is associated with a low rate of complications, making it a safe option.
There are few publications on this subject and it would be important to have good quality, preferably comparative studies in order to arrive at more robust conclusions for medical practice.
FundingThe funding of this review came from our own resources, with the advice from CES University.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Arcila Lotero MA, et al. Eficacia y seguridad del bloqueo de nervio supraescapular guiado por ultrasonido en pacientes con dolor crónico de hombro. Rev Colomb Anestesiol. 2013;41:104–8.