Performing ultrasound-guided nerve blocks has proven to be safe, but ergonomic considerations are essential.
MethodsA non-systematic literature search was conducted in the Medline/Pubmed and Embase databases.
ObjectiveTo describe the influence of operator position, monitor location, and hand position in performing ultrasound-guided nerve blocks.
ResultsPoor ergonomics is a key factor of error when performing nerve blocks under ultrasound guidance. “In-plane” needle insertion increases success. An inappropriate position may be a cause of muscle-skeletal disorders. Based on these results, we propose specific element location and operator position for the performance of certain nerve blocks.
ConclusionPerforming ultrasound-guided nerve blocks requires an ergonomic work area allowing for greater comfort and effectiveness, thus reducing the occurrence of muscle-skeletal disorders.
Los bloqueos guiados por ultrasonografía han demostrado ser eficaces, pero requieren considerar aspectos como la ergonomía.
ObjetivoDescribir influencia de la postura del operador, ubicación del monitor y posición de las manos, al realizar bloqueos con ultrasonografía.
MétodosSe realizó una búsqueda no sistemática de literatura en Medline/Pubmed y Embase.
ResultadosUna mala ergonomía es un factor de error al realizar bloqueos con ultrasonido. La inserción de la aguja “en plano” aumenta el éxito. Una posición inapropiada puede producir trastornos musculo-esqueléticos en el operador. Basados en esto, se propone una ubicación de elementos y posición del operador para realizar algunos bloqueos.
ConclusiónRealizar bloqueos con ultrasonido requiere un área de trabajo ergonómica para lograr mayor eficacia, y disminuir aparición de trastornos músculo-esqueléticos.
The use of ultrasound (US) in perioperative regional anaesthesia and analgesia has evolved rapidly,1,2 and its use has grown significantly in anaesthetic practice.3,4 Its main advantage is the ability to identify anatomical structures in real time, allowing the precise administration and distribution of the local anaesthetic (LA) around the nerve structure.5,6
Increasingly more data are being published at the present time suggesting higher efficacy and safety with the use of US-guided nerve blocks,7,8 specifically for interscalene,9,10 supraclavicular,11 infraclavicular,12,13 axillary,14–16 femoral,17 and sciatic popliteal17–20 blocks. A meta-analysis found that when US is compared with peripheral nerve (PN) stimulation, the risk of failure is lower (RR 0.41, 95% CI 0.26–0.66, p=0.001), the procedure is faster (1min less in average with ultrasound), latency is shorter (onset time is reduced by a mean of 29%), duration is longer (by an average of 25%), and there is a lower risk of vascular puncture (RR 0.16, 95% CI 0.05–0.47, p=0.001).21
After analysing a database of 20,021 patients undergoing 25,336 PN blocks, Barrington and Kluger22 reported that the use of US, compared to PN stimulations, reduced the frequency of LA-related toxicity by up to 65% (0.59 events/1000 blocks in those cases where US was used vs. 2.1 events/1000 blocks using PN stimulation).22 However, as was mentioned by Hadzic et al.,23 the use of US in expert hands may reduce, although not eliminate, the most common complications of regional anaesthesia (RA) such as blood vessel punctures and inadvertent intraneural or intravascular injections.23
The growing use of US in RA3,4 has created the need to consider aspects that are relevant to this practice, including ergonomics and the adequate location of all the necessary elements in space.24 Multiple authors suggest that these variables influence the performance of US-guided blocks25,26 in terms of outcomes for the patient and of operator wellbeing.27–30 This prompted us to conduct a non-systematic review of the literature in the Medline/Pubmed and Embase databases to look for current evidence regarding ergonomics in RA.
Is there a relationship between ergonomics and nerve blocks?Ergonomics is the science of the physical interaction between individuals and their working environment, including equipment design and operator training in terms of motor, visual, spatial, and hearing skills, and abilities.31 When ergonomic strategies are applied, task performance and efficacy can be optimized and human wellbeing may be maximized.27
Given the advances in biomedical knowledge and technology, healthcare professionals currently find themselves working in increasingly complex and demanding environments. An example of this is the work of the anaesthetist in the modern operating theatre where he/she is exposed to multiple visual, tactile and auditory stimuli, creating a greater clinical and ergonomic challenge, especially when it comes to performing procedures.27 There is growing recognition of the importance of ergonomics in the practice of anaesthesia.32,33 To this date, ergonomics is not taught in most academic training programmes despite the recognition of its potential benefits.26,34,35
The use of US in RA requires education and training in order for the anaesthetist to acquire concepts and develop psychomotor skills, including the following26,36:
- 1.
Achieving adequate imaging and visualization of the nerve structure.37
- 2.
Alignment of the needle with the US beam.38
- 3.
Identifying the advancement of the needle in real time.37
- 4.
Placing the tip of the needle on the target point.38
- 5.
Identifying the appropriate distribution of the LA around the nerve.37
If any of these steps is performed suboptimally, there is a lower probability of achieving a successful nerve block. Sites et al.26,39 found that poor ergonomics (defined as turning the trunk, holding the needle with the non-dominant hand and turning the head 45 degrees or more) is a source of error among anaesthesia residents and novice operators when performing US-guided blocks, and is associated with fatigue and lower performance.26,39
In view of the above, it is suggested that adopting the inadequate ergonomics may have a dual relevant impact: first, block failure due to lower accuracy of hand motions, either of the hand holding the needle or the hand holding the probe26 and difficulty aligning with the US bema,40 leading to impaired viewing of needle advancement and LA distribution; and, second, the potential development of muscle-skeletal disorders in the operator.41,42
Does ergonomics have an impact on the success of a nerve block?As has been previously determined, US-guided RA is a safe and effective technique for performing nerve blocks,8,21,22 provided perfect visualization of the nerve structure is achieved.43 The needle may be advanced towards the target perpendicular or parallel to the US beam, in what is known “out-of-plane” insertion (OPI) or “in-plane insertion (IPI), respectively. With the in-plane technique it is possible to watch the needle as it moves towards the target, but it requires skill and may create a false sense of security.25,44 OPI is a more complex technique aimed at visualizing the tip of the needle or watching for indirect signs such as the movement of the adjacent tissue as the needle advances, or hydrolocalization,45 but it has the advantage of providing a length of insertion which is three times shorter and more comfortable for the patient.46
Chapman et al.25 state that “The operator must focus on the image on the monitor and on the patient, hence the importance of having the anatomical area and the US machine in the same line of view. This requires placing the screen at eye level on the opposite side of the operator”.25 Using this hypothesis, Langford et al., in a trial with 31 anaesthetists, found that placement of the US machine in front of the operator improved accuracy with in-plane needle advancement when compared with the placement of the machine perpendicular to the operator, but found no difference in terms of the time for performing the task.28 The importance of these results relates to the fact that “accuracy in needle placement is more important than the speed in reaching the target because it improves the odds of a successful block and reduces complications associated with inadvertent damage to the non-target structures”.28
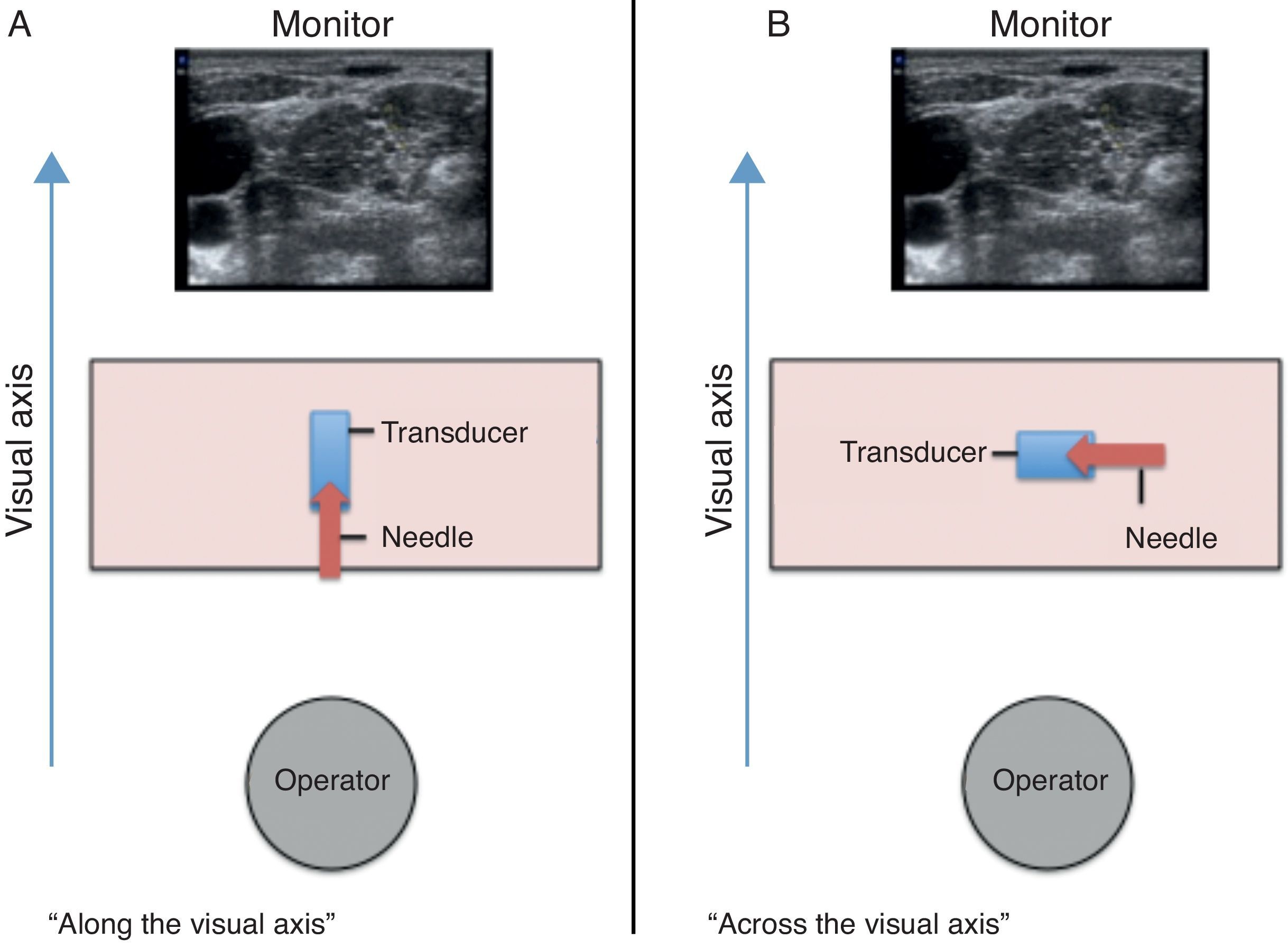
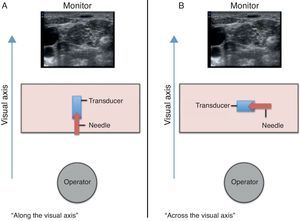
Speer et al.29 describe two ways to position the hands in relation to the visual axis of the operator while performing “in-plane” needle insertion29:
- 1.
“ALONG the visual axis” (ALVA): the long axis of the transducer with the needle parallel to the visual axis (Fig. 1A).
- 2.
“ACROSS the visual axis” (ACVA): locating the long axis of the transducer and placing the needle perpendicular to the visual axis (Fig. 1B).
A randomized clinical trial using simulation with phantom-type models analyzed the performance of 24 novice operators as they advanced the needle towards a target under ultrasound guidance. Each participant performed 5 ALVA attempts and 5 ACVA attempts, and it was found that when the 2 axes are parallel there is a significant reduction in the time to perform the task and improved image quality.29
Wilson et al.30 compared the use of the ALVA and ACVA techniques in medical students and found that the use of the IPI approach with the former technique was associated with better visualization, shorter time to complete the task, and higher success; moreover, the participants reported a higher preference for this technique.30 The authors suggest that in novice operators, needle advancement with the ALVA technique minimizes the need for needle relocations, reduces the time to perform the procedure, improves ergonomic performance and enhances needle tip viewing, thus improving safety and the rate of successful outcomes.30
May inappropriate ergonomics when performing US-guided nerve blocks give rise to muscle-skeletal disorders in the operator?The importance of an ergonomic ultrasound workstation to reduce the incidence of muscle-skeletal disorders has been widely described.42 Although this aspect has not been studied specifically for US-guided nerve blocks, similar considerations could be extrapolated and applied.
The physical factors most commonly associated with the development of muscle-skeletal disorders include vibrations, excess force and tension, strong or uncomfortable motions, poor posture, repetitive motions and prolonged pressure time.47 Except for vibrations, all of these factors may be present when performing ultrasound scans, in particular in obese patients who require the use of higher force on the probe in order to reduce the thickness of the fat layers and improve image quality.42,48
The parts of the body most commonly affected as a result of poor posturing are the shoulders (76%), neck (74%), wrists (59%), back (58%) and hands (55%).49 Although many of the symptoms are mild, if left unaddressed they may lead to serious and debilitating chronic disorders.42 The most frequent diagnoses are tendinitis and tenosynovitis affecting shoulders, hands and wrists.50
The positions most frequently associated with inappropriate ergonomics when performing ultrasound scans are shown below42:
- 1.
Wrist flexion, extension and deviation (Figs. 2.1–2.3)
- 2.
Neck flexion, extension and torsion (Figs. 3.1–3.3)
- 3.
Trunk flexion and torsion (Figs. 4.1 and 4.2)
- 4.
Arm abduction (angle >30 degrees) (Fig. 5)
- 5.
Ergonomic overstretching to reach the target (Fig. 6)
- 6.
Pinch grasp of the probe (there is up to a five-fold reduction in the force applied when the volar grip is used42) (Fig. 7)
Operator posture and interaction with all the pieces of equipment have to be considered for an appropriate scan.51 An ergonomic work area must include the following:
- 1.
A table with lateral retractile supports in order to avoid creating a larger distance to the patient, with powered height adjustment because manual controls interfere with the chair and operator location.42
- 2.
A chair with wheels, adjustable from the seating position.42,51
- 3.
A spacious examination room with indirect lighting that does not interfere with the display.42,51
Based on the information above, approaches to ensure appropriate ergonomics are proposed24:
- 1.
Avoiding inadequate positioning of the hands, wrists, neck, trunk and shoulders (Figs. 2–7).
- 2.
Placing the US machine on the opposite side of the side of the body where the nerve block will be performed.
- 3.
Avoid turning the head 45 degrees or more.
- 4.
Aligning the monitor with the operator's visual axis.
- 5.
ALVA alignment of the probe and needle.
- 6.
Working from a sitting position with the arm supported on the bed.
- 7.
Adjusting the height of the bed.
- 8.
No hand crossing (transducer and needle).
- 9.
Holding the needle with the dominant hand.
- 10.
Avoid the pinch grip when holding the transducer (Fig. 7).
- 11.
Holding the probe from the bottom and using the patient's skin as support for the fingers in order to gain greater stability.
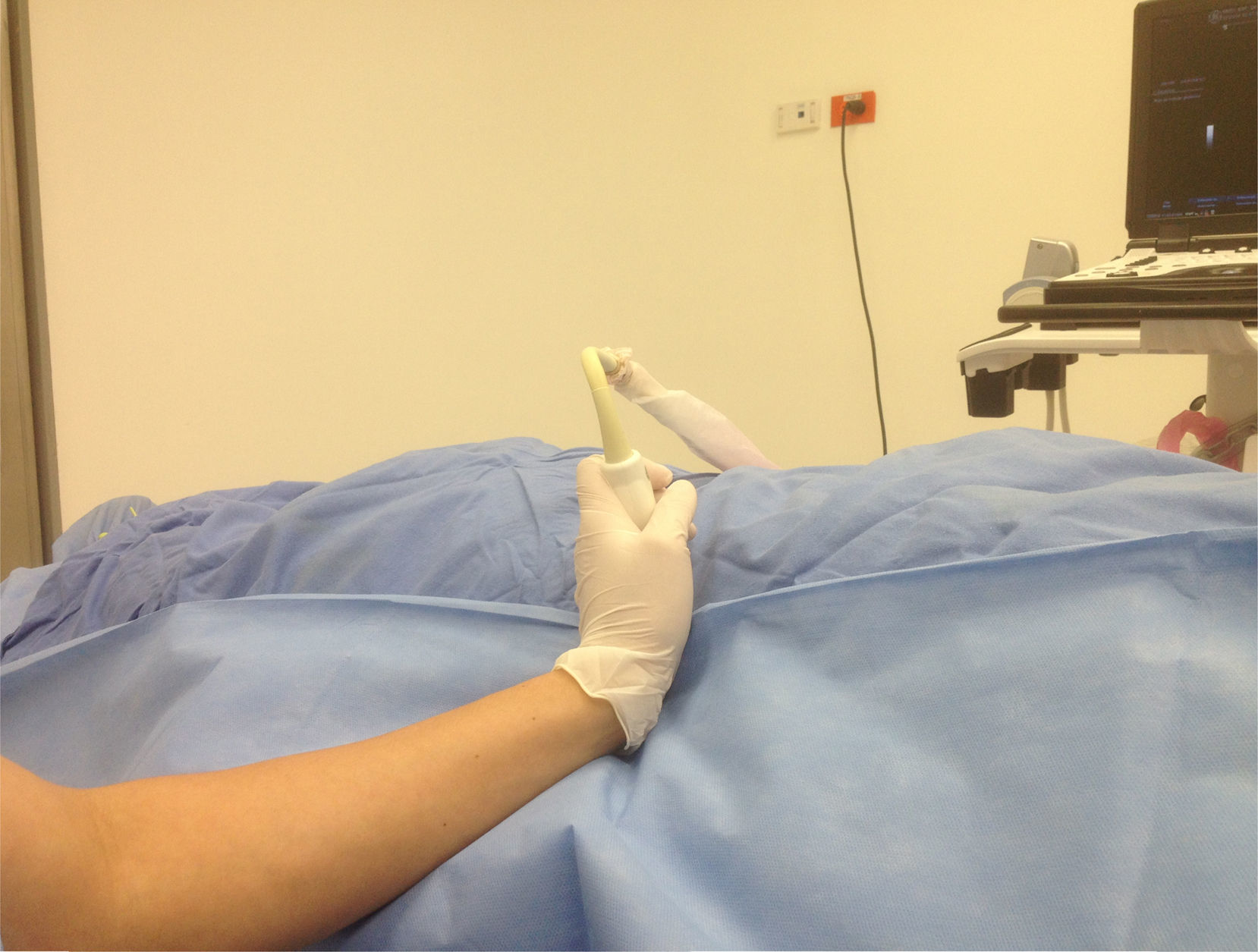
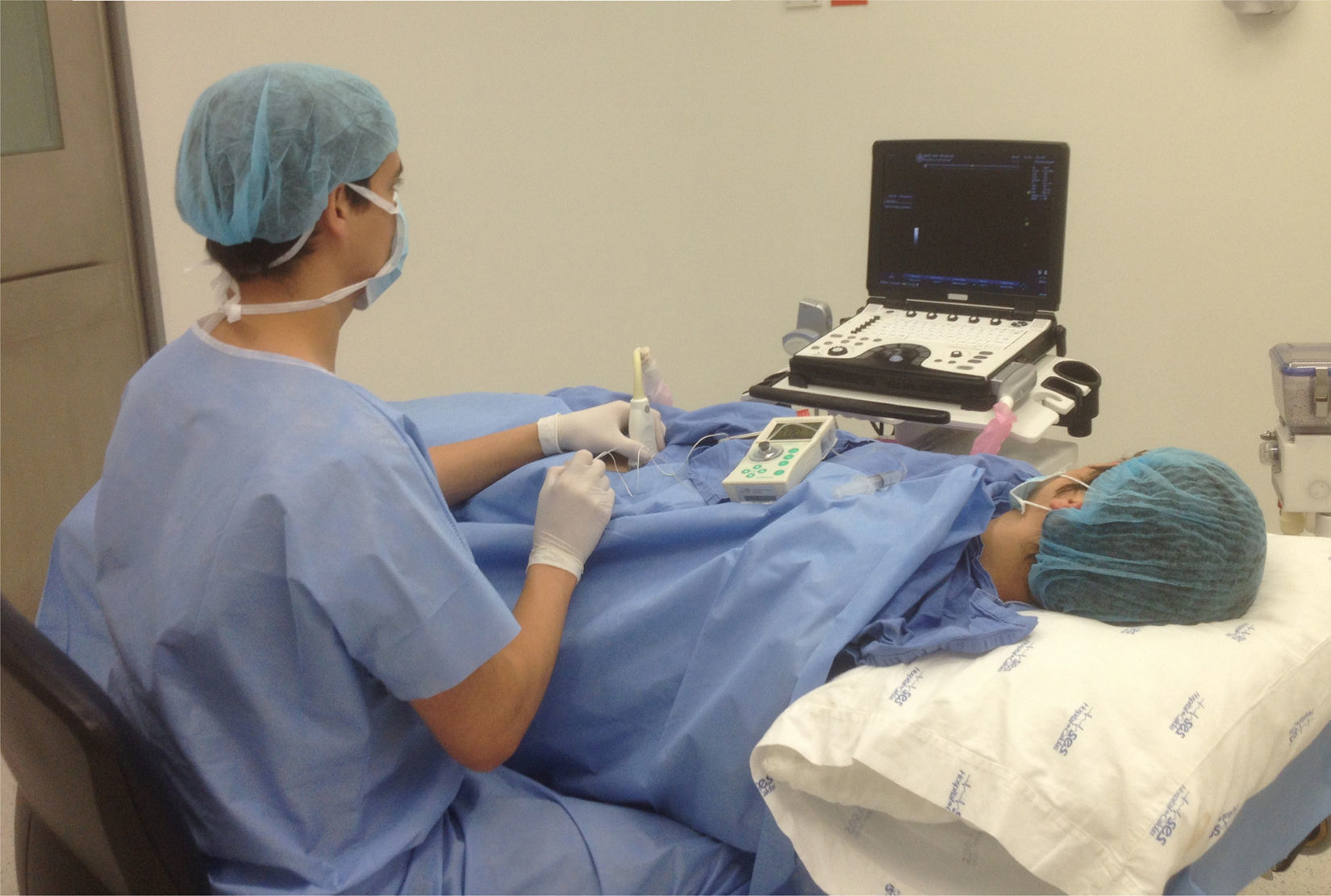
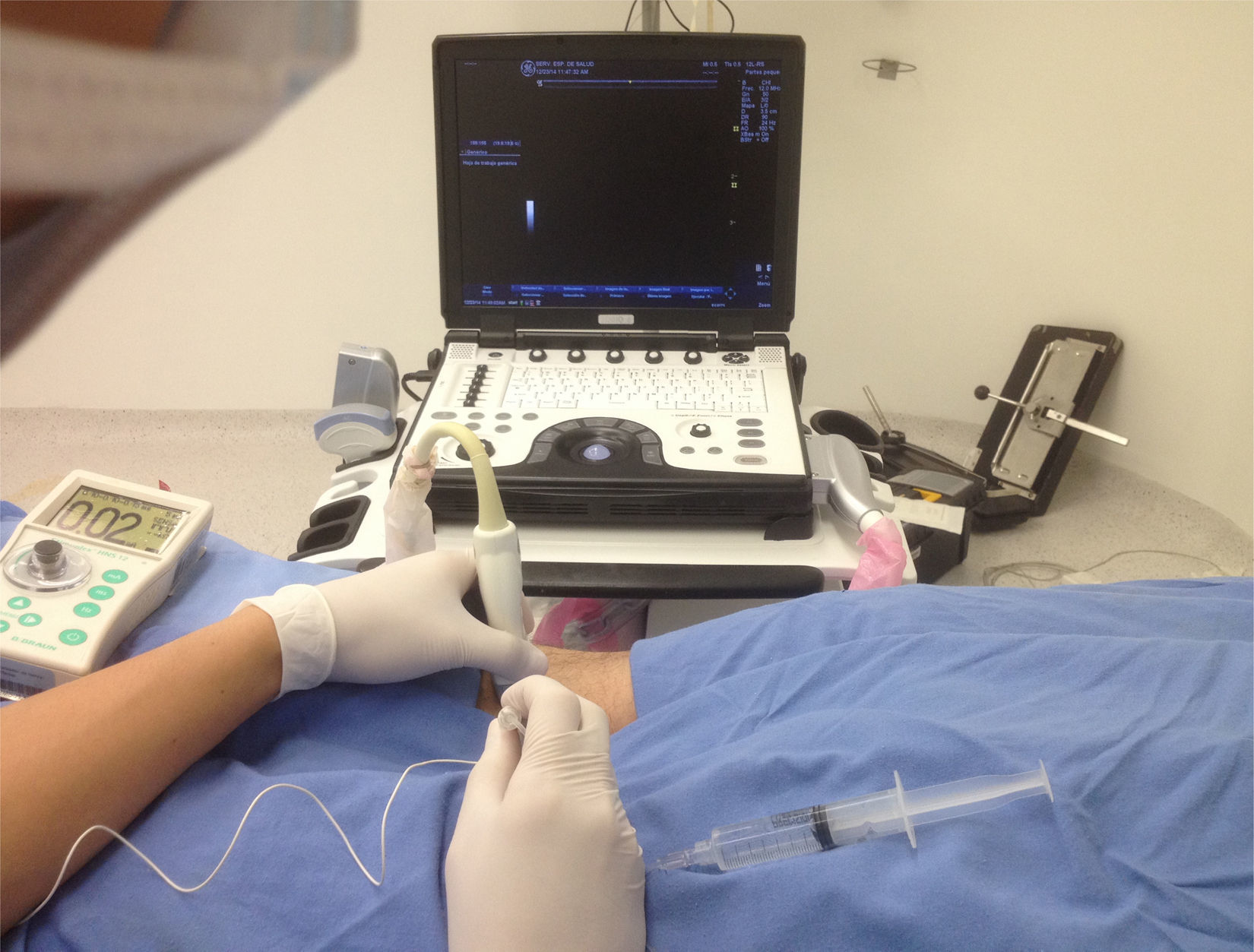
A proposal for ergonomic performance of interscalene and supraclavicular nerve blocks (Fig. 8), axillary blocks (Figs. 9.1 and 9.2), femoral blocks (Figs. 10.1 and 10.2) and sciatic popliteal blocks (Figs. 11.1 and 11.2) is presented below.
Position for performing interscalene and supraclavicular nerve blocks. Patient in supine position at 45 degrees, arm in adduction, head slightly rotated to the contralateral side. Monitor in front, aligned along the visual axis. Volar grasp of the high-frequency linear probe, using the patient as support for the hand. In-plane needle entry with along-the-visual-axis approach.
Position for performing the axillary nerve block. Patient in supine position with the arm in 90 degrees of abduction and flexed at the elbow, head rotated to the opposite side of the block. The anaesthetist is at the head of the bed, on the side where the block will be performed. The monitor is in front, aligned along the visual axis. Ergonomic position with no inappropriate posture of the wrist, neck, shoulder or trunk. Volar grasp of the transducer with support for the hand. Needle entering in-plane, with along-the-visual-axis approach.
Position for performing femoral nerve block. Patient in supine position with the leg in slight external rotation. The anaesthetist is on the side of the block, with the monitor in front, aligned along the visual axis. Ergonomic position with no inadequate wrist, neck, shoulder or trunk poture. Volar grasp of the transducer with support for the hand. In-plane needle insertion with along-the-visual-axis approach.
Position for performing the sciatic popliteal nerve block. Patient in prone position with the lower limbs in neutral position. The anaesthetist is positioned on the opposite side of the block, with the monitor in front, aligned along the visual axis. Ergonomic position with no inadequate wrist, neck, shoulder or trunk posture. Volar grasp of the transducer with support for the hand. In-plane needle insertion with along-the-visual-axis approach.
The growing use and development of US in RA are driven by the ability to achieve real-time visualization, thus improving efficacy and safety. Because it is “operator-dependent”, its use does not guarantee success or absence of complications in cases of insufficient skill or knowledge of the anatomy. The main psychomotor skills that need to be developed include the following: achieving an image of the area of interest, aligning the needle with the US beam, advancing the tip of the needle accurately to the ideal site for injecting the LA, and recognizing adequate distribution. As part of developing and maintaining these skills, an ergonomic work area helps adopt the appropriate postures to reduce the occurrence of muscle-skeletal disorders and to improve comfort and effectiveness when performing the procedure. The latter is based on data suggesting that the alignment of the transducer, needle and screen in the same parallel plane and visual axis, improves of visualization and needle advancement accuracy, which is key to a successful nerve block.
FundingThe authors did not receive sponsorship to undertake this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Aguirre-Ospina OD, González-Maldonado JF, Ríos-Medina ÁM. Ergonomía en los bloqueos nerviosos guiados por ultrasonografía. Revisión no sistemática de la literatura. Rev Colomb Anestesiol. 2015;43:331–339.