The modified Wilson infraclavicular approach (MWIA) was described in our institution for brachial plexus blocks in paediatric patients. However, concordance studies between this approach and ultrasound for the identification of ideal puncture site have not been reported.
ObjectiveTo determine the concordance between MWIA and ultrasound for localization of the ideal puncture site.
Materials and methodsDescriptive observational study; we included 100 healthy patients between 1 and 16 years of age, with parental consent, over a 5-month period. Continuous variables were described and kappa statistics were used for concordance evaluation. We also conducted a multivariate analysis to confirm the relationship between the measured distances and weight and height.
ResultsThe distance from the skin to the brachial plexus, as well as the distance between the coracoid process and the brachial plexus, and the distance from the coracoid process to the pleura were all smaller in abduction, with no statistically significant difference. Height and weight are independent factors that determine the distance between the coracoid process and the posterior cord, both in adduction and abduction. The concordance of MWIA vs. ultrasound for determining the ideal puncture site was 47% in both positions.
ConclusionsConcordance between MWIA and ultrasound for the determination of the ideal puncture site is low when it comes to anatomic localization; however, this technique must be evaluated in randomized clinical studies in order to determine its efficacy and usefulness. Height and weight are independent factors that determine the distance between the coracoid process and the posterior cord in adduction and abduction.
En pacientes pediátricos, el sitio óptimo de inyección para el abordaje infraclavicular sigue siendo sujeto de debate; no hay estudios de concordancia entre el abordaje infraclavicular de Wilson modificado para bloqueo del plexo braquial (AIWM) y el ultrasonido para la localización del sitio ideal de punción.
ObjetivoDeterminar la concordancia entre AIWM y ultrasonido para localizar el sitio ideal de punción.
Materiales y métodosestudio observacional descriptivo; se incluyeron 100 niños sanos entre 1-16 años, en un periodo de 5 meses. Se describieron variables continuas y se evaluó la concordancia mediante la estadística kappa. Se realizó análisis multivariado para confirmar la correlación entre las distancias, el peso y la talla.
ResultadosSe encontró una menor profundidad del plexo braquial y menor distancia entre el plexo braquial y la apófisis coracoides y entre la coracoides y la pleura en abducción, sin significancia estadística. El peso y la talla son factores independientes que determinan la distancia entre la apófisis coracoides y el cordón posterior en abducción y en aducción. La concordancia del sitio ideal de punción entre AIWM y ultrasonido fue 0,47 en ambas posiciones.
ConclusionesLa concordancia entre el AIWM y el ultrasonido para determinar el sitio ideal de punción es sorprendentemente baja. Sin embargo, desde el punto de vista de utilidad y eficacia clínica, estas técnicas deben ser comparadas y evaluadas con estudios clínicos aleatorizados. El peso y la talla determinan de forma independiente la distancia entre el cordón posterior y la apófisis coracoides en aducción y abducción del brazo.
According to studies conducted in the Netherlands, distal radius and wrist fractures account for approximately 25% of all paediatric fractures1 and traumatic injuries involving the hand range between 1800 and 2600 per 100,000 inhabitants per year in the Netherlands and Denmark, respectively.2 There are also congenital disorders involving the upper limb in 0.16–0.18% of live births in the United Kingdom.3
Significant technological and scientific advances in the field of regional anaesthesia over the past decade have led to improvements in our knowledge of the anatomy, and to better surgical approaches, with improved safety profiles. Together with greater availability of resources, this has promoted the use of regional anaesthesia in paediatric patients.4–9 However, the use of regional anaesthesia techniques in children is limited by the size of the structures, the proximity of the neural structures to critical structures (pleura, blood vessels), poorly defined superficial landmarks, a tight safety margin, a higher potential for toxicity related to local anaesthetics, and the need for sedation or general anaesthesia, which might mask any signs of alarm (paraesthesias).10,11
The infraclavicular approach for brachial plexus blocks is indicated for hand, forearm, elbow and arm surgery (the shoulder excluded). Its advantages include a higher probability of achieving axillary and musculocutaneous nerve blocks when compared with the axillary approach; ease of fixation of the continuous analgesia catheters; lower impact on pulmonary function when compared to the supraclavicular and the interscalene approaches; and no arm abduction requirement.12,13 Disadvantages include the possibility of not achieving adequate posterior cord block when single injections are used; also, in the event of vascular puncture due to the depth of the structures, it is difficult to apply compressive manoeuvres.12
There are variations to the infraclavicular block: the coracoid approach,14,15 the lateral sagittal approach,16 the vertical approach,17 and the modified Raj approach.18,19 The coracoid approach is the most popular in the United States.20
The coracoid approach was first described by Whiffler21 and later modified by Wilson who, with the help of nuclear magnetic resonance imaging (NMR), determined that the ideal puncture site in adults was 2cm medial and 2cm caudal to the lateral tip of the coracoid process.15
In paediatric patients, the optimal injection site for the infraclavicular approach is still controversial.11 The modified Raj and the vertical approaches are considered “dangerous” because of the proximity of the puncture site to the cervical pleura.22,23 There are no publications at the present time in relation to Whiffler's approach or Wilson's modification in children. However, a modified Wilson technique for paediatric patients was developed at the National Rehabilitation Institute, consisting of using the coracoid process as the anatomical landmark and finding the puncture site medial and caudal to it according to the patient's weight. This modification has not been published before.
In 1999, Kapral described another modification of Whiffler's technique called the “lateral vertical” approach.24 Kapral reported a high rate of success using this technique (100%) with a broad range of nerve blocks with a broad range of nerve block spectrum (including the musculocutaneous, thoracodorsal, axillary and medial cutaneous brachial nerves) and absence of complications in adult patients.24 Later, Fleischmann and Ponde reported the use of this technique in paediatric patients, modifying the location of the puncture site, this time 0.5cm caudal to the coracoid process, with similar results as those found by Kapral.25,26 In 2004, Klaastad described the “lateral sagittal” technique in adults;27 however, there are few reports on the use of this technique in paediatric patients.28,29
The first report of an ultrasound-guided brachial plexus block through the infraclavicular approach in paediatric patients was described by Marhofer, who compared this technique with a neurostimulation-guided lateral vertical approach in a randomized clinical trial. He found shorter latency periods and longer block durations in the ultrasound group, with no difference in block quality after 30min.30
Despite the many advantages of ultrasound-guided techniques, the main limitations are still the cost of the equipment and the need for specialized training. Moreover, it does not totally eliminate the risk of inadvertent intraneural injection.31 On the other hand, safety recommendations in regional anaesthesia include triple monitoring (i.e., neurostimulation, ultrasound and injection pressure measurements).32
The objective of our study was to determine concordance between the modified Wilson infraclavicular approach and the use of ultrasound for the anatomic localization of nerve structures and of the ideal puncture site.
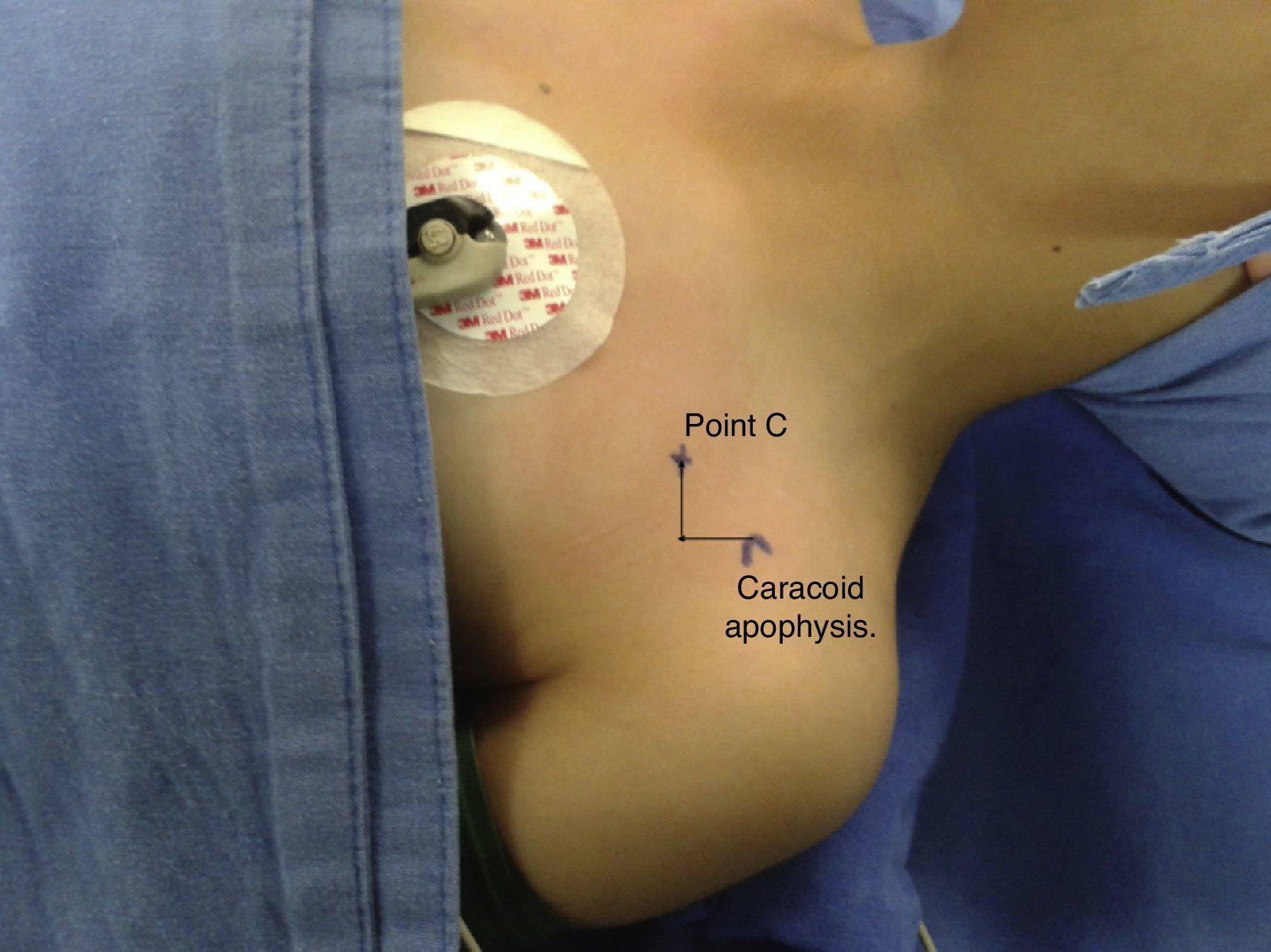
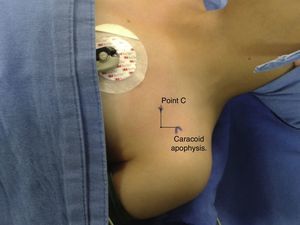
Materials and methodsA descriptive observational study was conducted. Patient recruitment was initiated once the approval of the Scientific Research Commission and the Ethics and Research Committee of the National Rehabilitation Institute was obtained. Patients included healthy children 1–16 years of age scheduled for open or closed reduction surgery for fractures of any extremity; patients with anatomical variants obscuring the visualization of the cords in the infraclavicular region were excluded. The parents of the children signed an informed consent and patients 12 or older signed an informed assent. Puncture site (C point) marking was done in accordance with the modified Wilson infraclavicular (MWIA) coracoid approach, as follows: for patients weighing less than 10kg, 1cm caudal and 1cm medial to the coracoid process; for patients weighing 10–20kg, 1.5cm caudal and 1.5cm medial to the coracoid process; for patients weighing more than 20kg, 2cm caudal and 2cm medial to the coracoid process (Fig. 1).
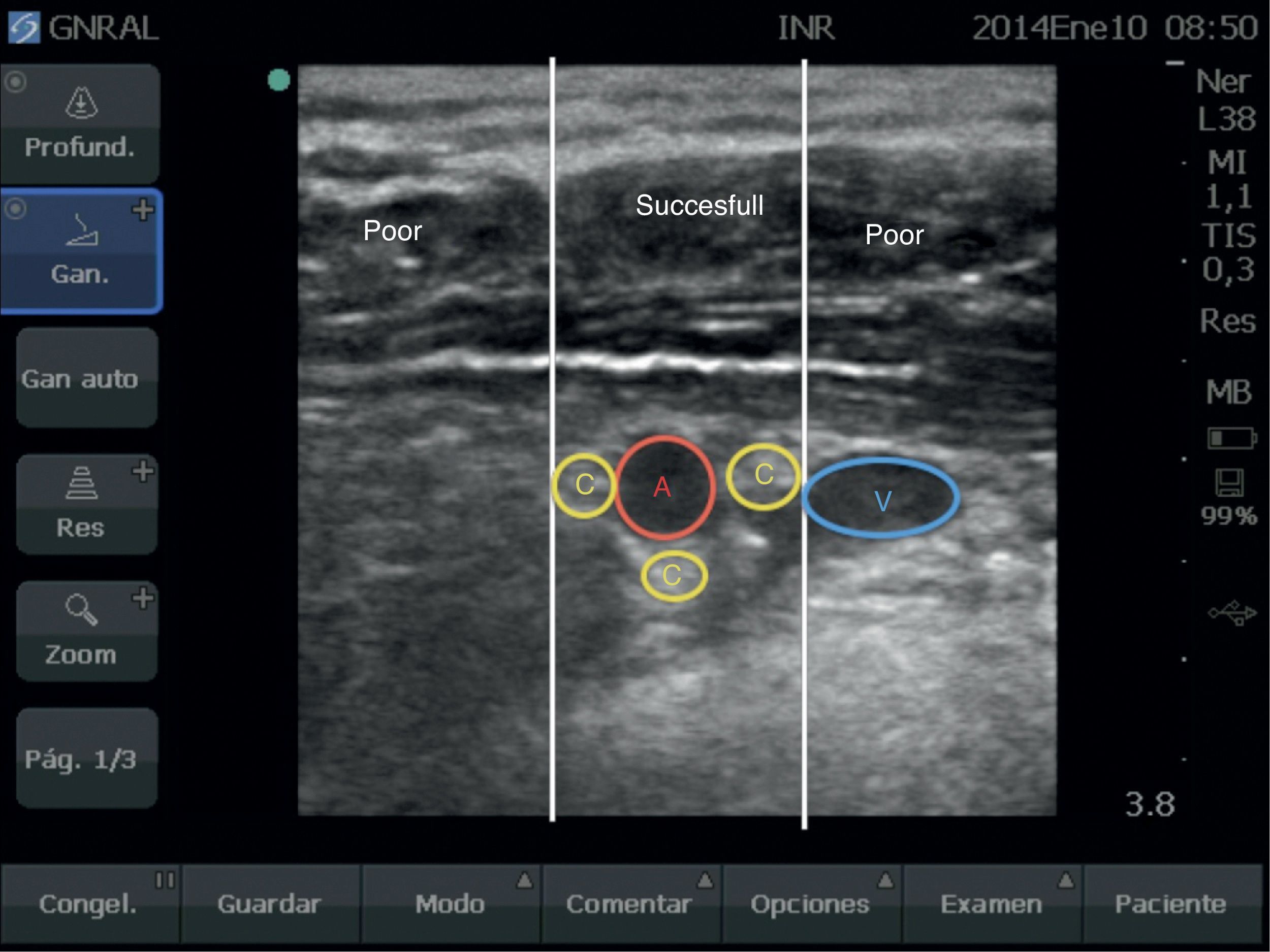
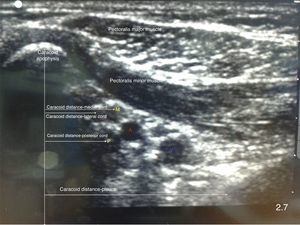
A Sonosite Micromaxx (Bothell, WA, USA) ultrasound machine with a high-frequency linear transducer (13–6MHz) was used for making measurements of any of the two extremities. The centre point of the transducer was placed on the C point marked as MWIA in a parasagittal orientation (Fig. 2), and the necessary depth and focus adjustments were made in order to ensure visualization of the target structures.
Localization was rated as “successful” when the axillary artery and the brachial plexus cords were visualized in the central third of the screen; “poor” if the axillary artery and the brachial plexus cords were seen on the lateral or medial third of the image; and “failed” when these structures were not visualized (Fig. 3).
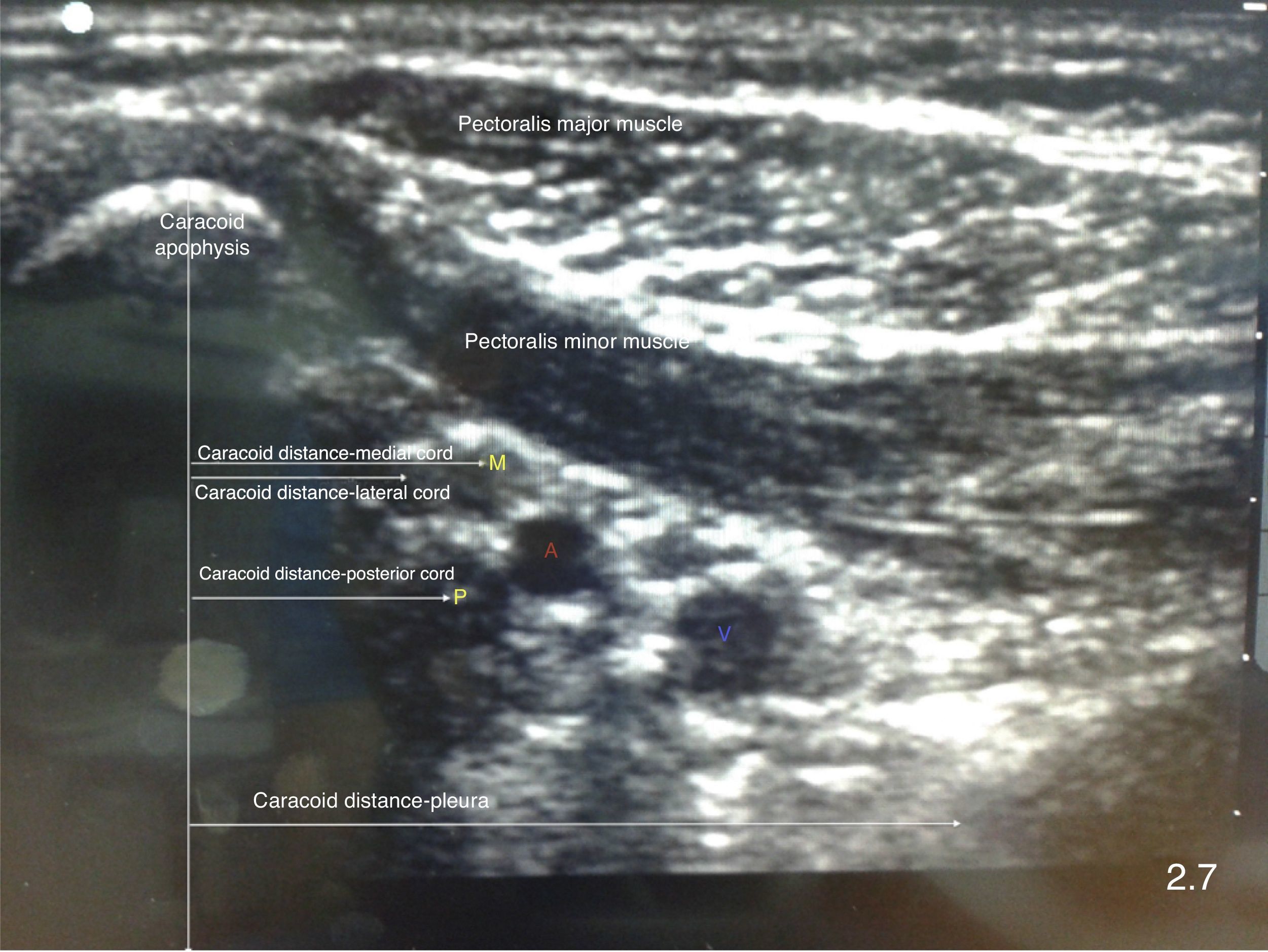
The Vienna classification described by Marhofer et al. was used to evaluate quality of imaging visualization.33 Additionally, distance measurements were made from the most prominent point in the coracoid process to the brachial plexus cords, from the skin to the cords, from the pleura to the coracoid process, and the position of the cords in relation to axillary artery was described (Fig. 4). For image acquisition, the transducer was positioned on an oblique sagittal plane.
Measurements were made with the arm in adduction and 90° of abduction with the patient under sedation or general anaesthesia for the scheduled surgical procedure. It is important to mention that the ultrasound scans were performed by two investigators wit experience in ultrasound-guided infraclavicular blocks.
The sample size was determined on the basis of convenience, requiring 100 patients over a 5-month period. The data were entered in an Excel database, and the STATA 10 software was used for data analysis. A measurement of central tendency was made for continuous variables. Kappa statistics were used to evaluate concordance between nominal variables. A linear regression was also performed in order to confirm the correlation between the distance from the coracoid process to the posterior cord and weight and height.
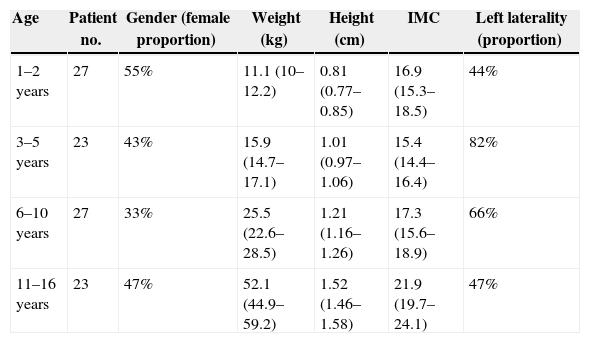
ResultsThe study enrolled 100 patients. Demographic characteristics are shown by age group (Table 1). The patients were distributed homogenously among age groups. Gender distribution was also homogenous except in the 6–10 group (33% female patients). Children under 5 tended to have a low BMI (body mass index) (<18).
Demographic characteristics. Weight, height and body mass index expressed as means and confidence intervals.
| Age | Patient no. | Gender (female proportion) | Weight (kg) | Height (cm) | IMC | Left laterality (proportion) |
|---|---|---|---|---|---|---|
| 1–2 years | 27 | 55% | 11.1 (10–12.2) | 0.81 (0.77–0.85) | 16.9 (15.3–18.5) | 44% |
| 3–5 years | 23 | 43% | 15.9 (14.7– 17.1) | 1.01 (0.97–1.06) | 15.4 (14.4–16.4) | 82% |
| 6–10 years | 27 | 33% | 25.5 (22.6–28.5) | 1.21 (1.16–1.26) | 17.3 (15.6–18.9) | 66% |
| 11–16 years | 23 | 47% | 52.1 (44.9–59.2) | 1.52 (1.46–1.58) | 21.9 (19.7–24.1) | 47% |
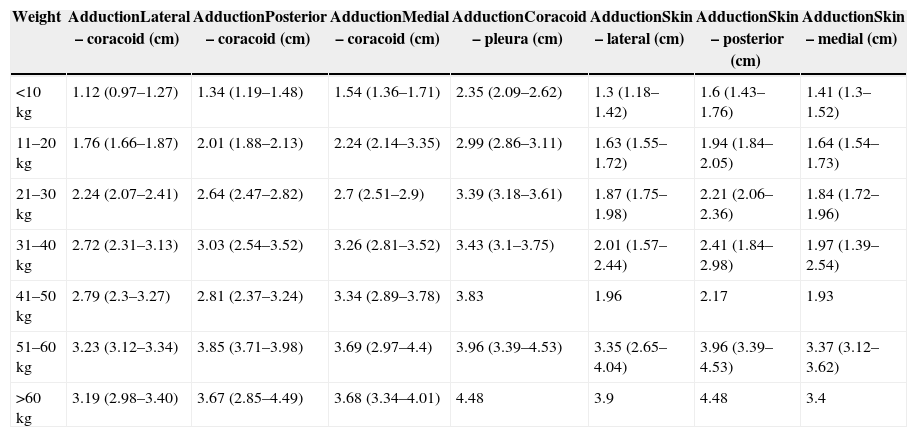
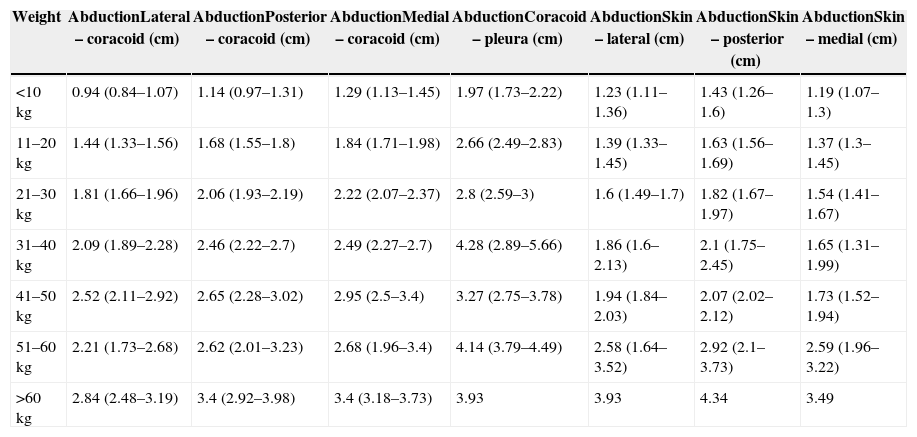
There is a significant difference in distances measured from the coracoid process to the brachial plexus in adduction and abduction between patients <10kg and those 11–20kg. However, in patients of more than 20kg there is no significant difference. Distances from the skin to the cords, the coracoid process to the cords, and from the coracoid process to the pleura were shorter in abduction in all age groups. However, the difference was not statistically significant (Tables 2 and 3).
Distances measured with the limb in adduction. Values are means and confidence intervals.
| Weight | AdductionLateral – coracoid (cm) | AdductionPosterior – coracoid (cm) | AdductionMedial – coracoid (cm) | AdductionCoracoid – pleura (cm) | AdductionSkin – lateral (cm) | AdductionSkin – posterior (cm) | AdductionSkin – medial (cm) |
|---|---|---|---|---|---|---|---|
| <10kg | 1.12 (0.97–1.27) | 1.34 (1.19–1.48) | 1.54 (1.36–1.71) | 2.35 (2.09–2.62) | 1.3 (1.18–1.42) | 1.6 (1.43–1.76) | 1.41 (1.3–1.52) |
| 11–20kg | 1.76 (1.66–1.87) | 2.01 (1.88–2.13) | 2.24 (2.14–3.35) | 2.99 (2.86–3.11) | 1.63 (1.55–1.72) | 1.94 (1.84–2.05) | 1.64 (1.54–1.73) |
| 21–30kg | 2.24 (2.07–2.41) | 2.64 (2.47–2.82) | 2.7 (2.51–2.9) | 3.39 (3.18–3.61) | 1.87 (1.75–1.98) | 2.21 (2.06–2.36) | 1.84 (1.72–1.96) |
| 31–40kg | 2.72 (2.31–3.13) | 3.03 (2.54–3.52) | 3.26 (2.81–3.52) | 3.43 (3.1–3.75) | 2.01 (1.57–2.44) | 2.41 (1.84–2.98) | 1.97 (1.39–2.54) |
| 41–50kg | 2.79 (2.3–3.27) | 2.81 (2.37–3.24) | 3.34 (2.89–3.78) | 3.83 | 1.96 | 2.17 | 1.93 |
| 51–60kg | 3.23 (3.12–3.34) | 3.85 (3.71–3.98) | 3.69 (2.97–4.4) | 3.96 (3.39–4.53) | 3.35 (2.65–4.04) | 3.96 (3.39–4.53) | 3.37 (3.12–3.62) |
| >60kg | 3.19 (2.98–3.40) | 3.67 (2.85–4.49) | 3.68 (3.34–4.01) | 4.48 | 3.9 | 4.48 | 3.4 |
Distances measured with the limb in abduction. Values are means and confidence intervals.
| Weight | AbductionLateral – coracoid (cm) | AbductionPosterior – coracoid (cm) | AbductionMedial – coracoid (cm) | AbductionCoracoid – pleura (cm) | AbductionSkin – lateral (cm) | AbductionSkin – posterior (cm) | AbductionSkin – medial (cm) |
|---|---|---|---|---|---|---|---|
| <10kg | 0.94 (0.84–1.07) | 1.14 (0.97–1.31) | 1.29 (1.13–1.45) | 1.97 (1.73–2.22) | 1.23 (1.11–1.36) | 1.43 (1.26–1.6) | 1.19 (1.07–1.3) |
| 11–20kg | 1.44 (1.33–1.56) | 1.68 (1.55–1.8) | 1.84 (1.71–1.98) | 2.66 (2.49–2.83) | 1.39 (1.33–1.45) | 1.63 (1.56–1.69) | 1.37 (1.3–1.45) |
| 21–30kg | 1.81 (1.66–1.96) | 2.06 (1.93–2.19) | 2.22 (2.07–2.37) | 2.8 (2.59–3) | 1.6 (1.49–1.7) | 1.82 (1.67–1.97) | 1.54 (1.41–1.67) |
| 31–40kg | 2.09 (1.89–2.28) | 2.46 (2.22–2.7) | 2.49 (2.27–2.7) | 4.28 (2.89–5.66) | 1.86 (1.6–2.13) | 2.1 (1.75–2.45) | 1.65 (1.31–1.99) |
| 41–50kg | 2.52 (2.11–2.92) | 2.65 (2.28–3.02) | 2.95 (2.5–3.4) | 3.27 (2.75–3.78) | 1.94 (1.84–2.03) | 2.07 (2.02–2.12) | 1.73 (1.52–1.94) |
| 51–60kg | 2.21 (1.73–2.68) | 2.62 (2.01–3.23) | 2.68 (1.96–3.4) | 4.14 (3.79–4.49) | 2.58 (1.64–3.52) | 2.92 (2.1–3.73) | 2.59 (1.96–3.22) |
| >60kg | 2.84 (2.48–3.19) | 3.4 (2.92–3.98) | 3.4 (3.18–3.73) | 3.93 | 3.93 | 4.34 | 3.49 |
Localization of the target anatomical structures using ultrasound on “C point” in patients under 10kg failed in 8.4% of patients, both in adduction as well as abduction; it was poor in 41% of patients in adduction and in 33.3% in abduction; and it was successful only in 66% of patients in adduction and 58.3% of patients in abduction.
In patients 10–20kg, localization of the target anatomical structures using ultrasound on “point C” failed in 13% of patients in adduction and 0% in abduction; it was poor in 41% of patients in adduction and in 43% in abduction; and was successful in 46% of patients in adduction and 56% in abduction.
In patients over 20kg, localization of the target anatomical structures using ultrasound on “point C” failed in 13% of patients in adduction and in 4.1% in abduction; it was poor in 49% in adduction and in 59.1% in abduction; and it was successful in 38% in adduction and in 36% in abduction. No statistically significant differences were found in terms of successful ultrasound identification in adduction or abduction according to the weight of the patients.
In terms of the quality of the visualization, 88% of the measurements were given a score of 2, and the rest were given a score of 3 under the Vienna classification. There were no statistically significant differences between age groups regarding the quality of visualization.
A multivariate analysis was conducted in order to determine the correlation between the distance from the coracoid process to the posterior cord in accordance with weight and height, and a statistically significant correlation was found in adduction (weight: p=0.015, height: p<0.01) and in abduction (weight and height p<0.01).
Position of the cord in the brachial plexus in relation to the axillary artery was evaluated in adduction and abduction, using a clock distribution. Considering that no intervention was performed and cords were, therefore, not identified using neurostimulation, cord positions described in previous anatomical studies were used. The lateral cord was defined as the most superficial and closest to the coracoid process; the posterior cord was defined as the most posterior in relation to the artery; and the medial cord was defined as the one most frequently located between the axillary artery and vein.
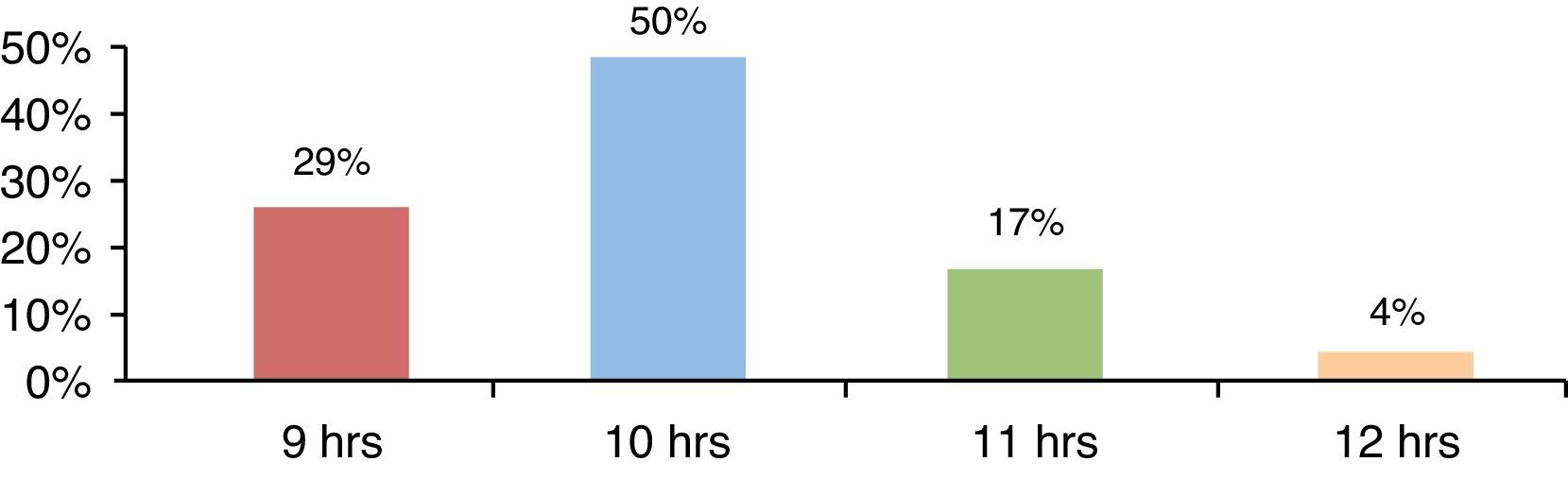
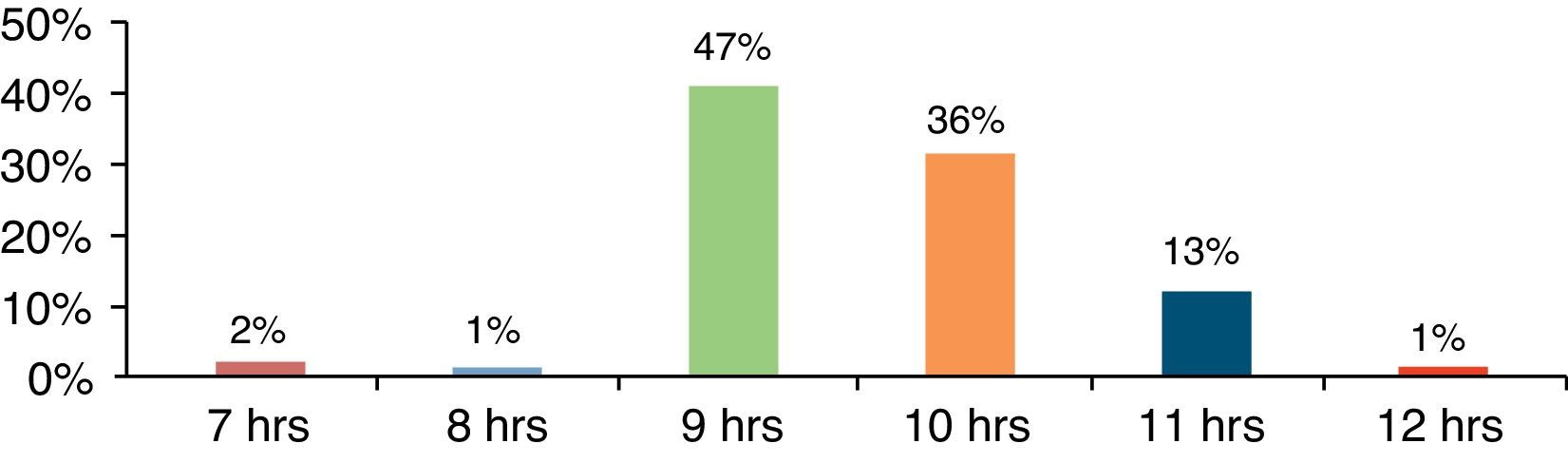
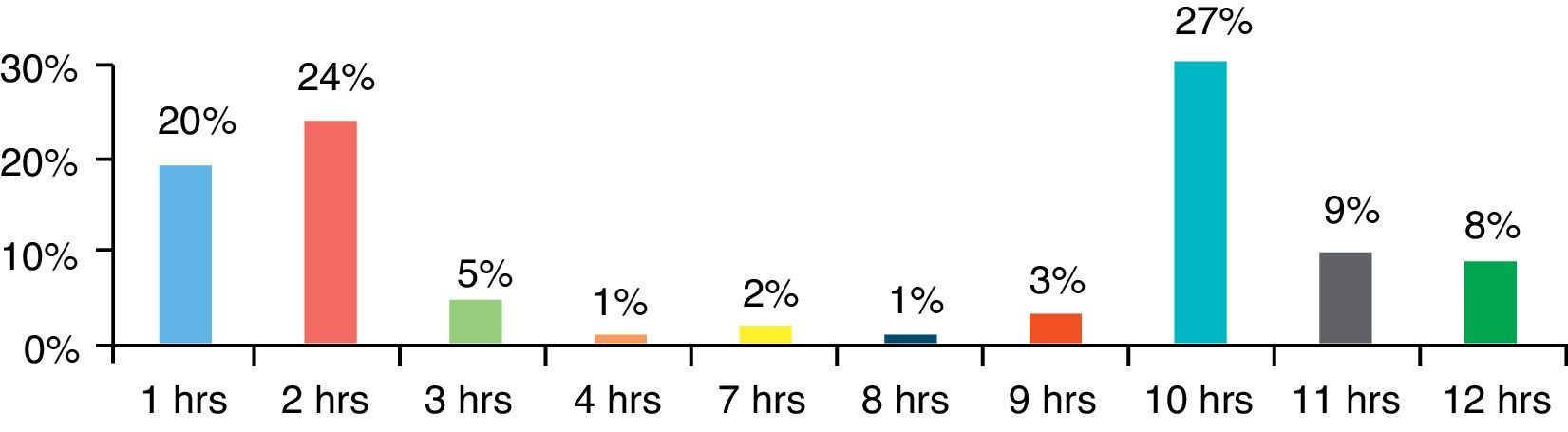
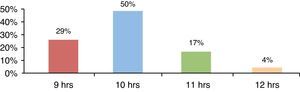
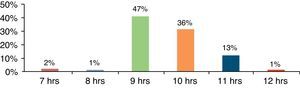
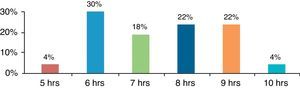
The lateral cord was found between 7 and 12 o’clock, and the most frequent location was at 10 o’clock in adduction (50%) and 9 o’clock in abduction (47%) (Figs. 5 and 6).
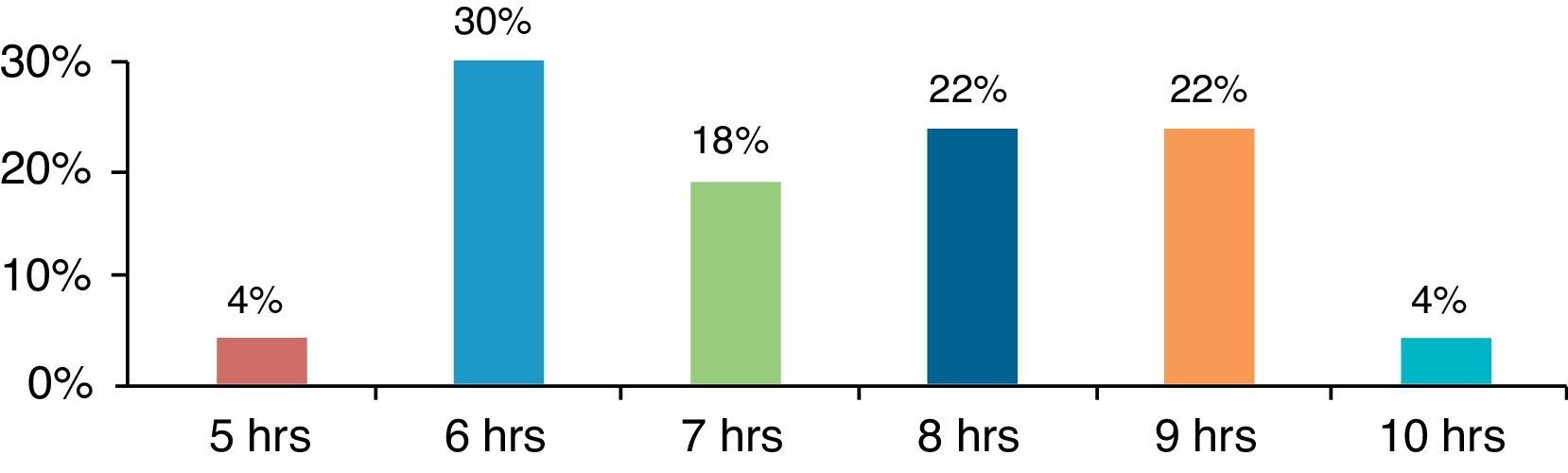
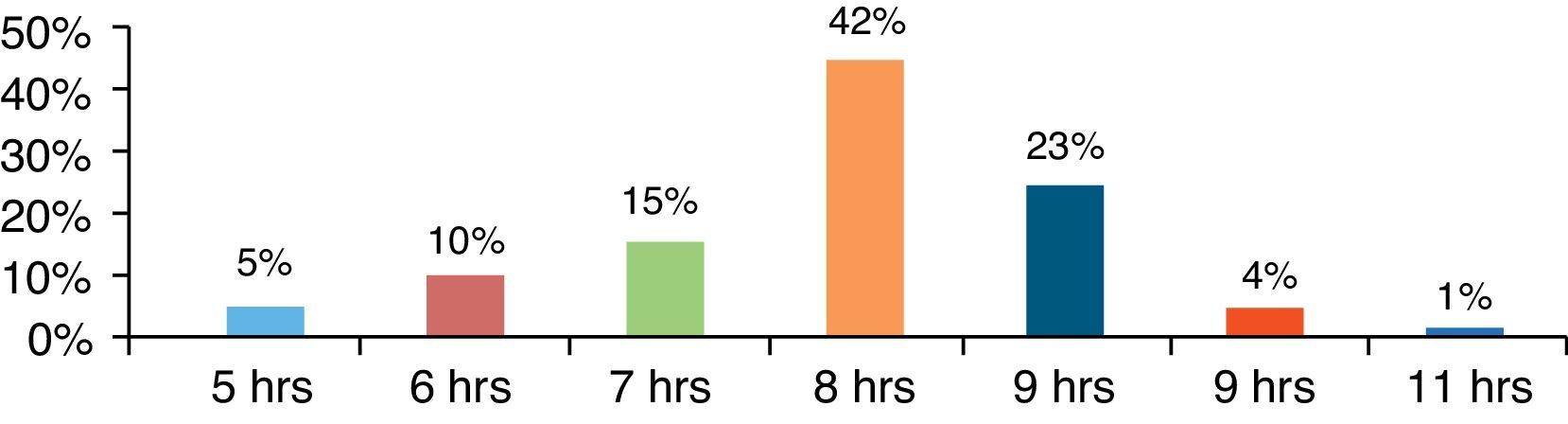
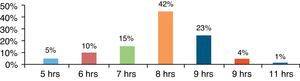
The posterior cord was found between 5 and 11 o’clock. The most frequent location was at 6 o’clock in adduction (30%) and at 8 o’clock in abduction (42%) (Figs. 7 and 8).
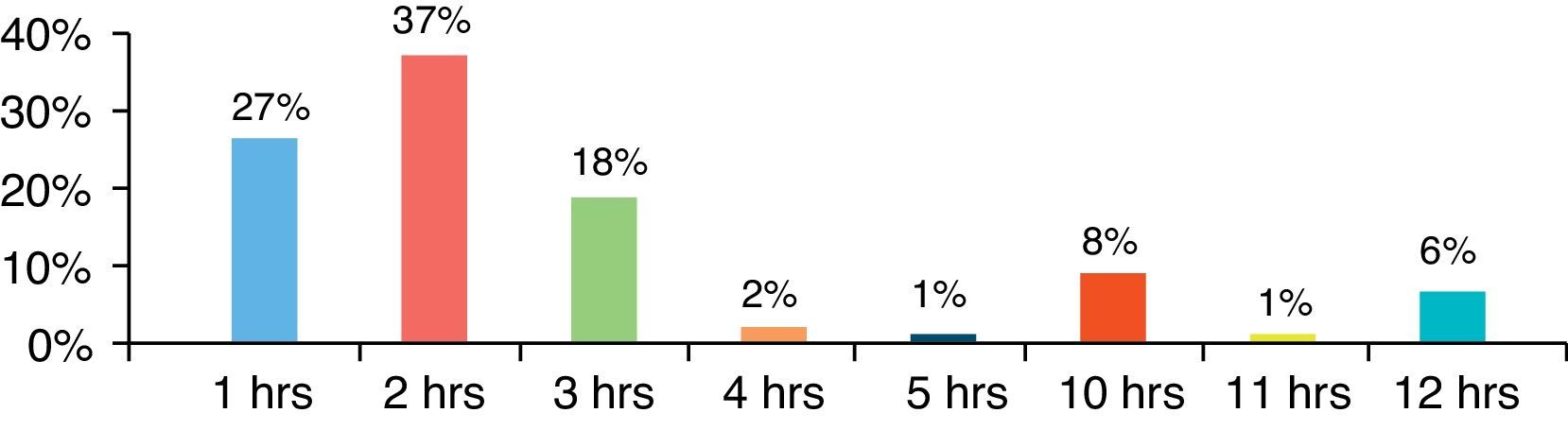
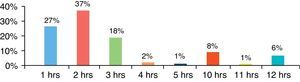
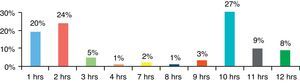
The greatest location variability was found for the medial cord, mainly in abduction. The most frequent location was at 2 o’clock in adduction (37%) and at 10 o’clock in abduction (27%) (Figs. 9 and 10).
Concordance between the modified Wilson approach and ultrasound for determining the ideal puncture site was 0.47 in adduction and abduction.
DiscussionThe objective of this study was to determine concordance between the MWIA and ultrasound for the location of the ideal anatomical puncture site, considering the lack of clinical studies regarding this topic in the literature, and the fact that there is only one similar study in adult patients. The study by Kuo et al.,34 assessed the accuracy of Wilson's coracoid approach for the location of the ideal puncture site and compared it with ultrasound in adult patients. It was found that the accuracy rate for the landmark-based approach was 74.4%.34 In our study, concordance between anatomical landmarks (MWIA) and ultrasound for identifying the ideal puncture site was only 0.47, suggesting that the landmark-based approach might not be adequate for predicting the ideal puncture site in paediatric patients. However, due to the usual individual anatomical variability, it is not very probable that a method guided by anatomical landmarks can be successful in 100% of cases without the need for needle repositioning.
It is important to mention that, given the size of paediatric patients, a 1cm distance difference, perhaps irrelevant in adults, might be quite significant in a child. There are other factors influencing success with the first attempt, including the entry angle of the needle in relation to the skin, which might lead to a failed block even when the exact entry point is determined by anatomical landmarks or by other means. In this regard, ultrasound provides the advantage of direct visualization of needle orientation.
Multiple studies have been conducted in adult populations using nuclear magnetic resonance (NMR) in order to advance the development of landmark-based approaches.15,27,35,36 However, the use of NMR or computed tomography-based studies in healthy children is limited by the need to provide sedation or general anaesthesia, mainly in smaller children who might suffer adverse events associated with anaesthetic agents or the exposure to ionizing radiation.37–40 From this perspective, studies using ultrasound are warranted.
The study by Ruiz et al. assessed the influence of arm abduction on the distance of the axillary artery from the skin, the coracoid process and the pleura, using ultrasound in adult patients. They reported a shorter depth of the axillary artery in abduction, but they did not find any differences in pleural depth in abduction, or regarding the distance between the coracoid process and the axillary artery.41 The study by Greher et al. sought to identify the accuracy of the vertical infraclavicular approach developed by Kilka by means of ultrasound measurements in healthy adults. They found that the overall accuracy of Kilka's vertical approach was not sufficient to predict the optimal puncture site.22
In our study, there was no statistically significant difference in the depth of the brachial plexus, the distance between the cords and the coracoid process, or the distance between the coracoid process and the pleura in abduction. This is consistent with the results from studies performed in adults. Ultrasound may possibly underestimate the depth of the brachial plexus structures due to the compressive effect from the transducer. The measurements obtained suggest that the distance between the coracoid process and the brachial plexus is modified to a greater degree in children under 20kg. Additionally, it was found that weight and height are independent variables that modify the distance between the coracoid process and the posterior cord. This suggests that a formula based on weight and height should be developed for children under 20kg in order to calculate the distance between the coracoid process and the brachial plexus when it comes to performing infraclavicular blocks.
As for the location of the brachial plexus cords in relation to the axillary artery, it was found to be highly variable in particular for the medial cord. In an earlier study by Sauter et al. using NMR in adult patients, the authors found the brachial plexus cords between 3 and 11 o’clock.35 A limitation of our study was that the cords were not identified using neurostimulation, hence our inability to assert that they were correctly identified.
Patients were not studied bilaterally, and this may also be a limitation of this study, considering reports of individual right/left asymmetry in 61% of cases.12
In one of its publications, the Paediatric Regional Anaesthesia Network (PRAN) reported a higher tendency towards performing ultrasound-guided peripheral blocks in the upper extremity (82%), leading to the assumption that ultrasound availability may explain the increasing number of peripheral nerve blocks.4 In the most recent study by ADARPEF (L’Association Des Anesthésistes-Réanimateurs Pédiatriques d’Expression Française), there was also a higher trend towards the performance of peripheral nerve blocks in paediatric patients.42 Despite the advantages of ultrasound,31 availability of these machines is low in many developing countries, hence the continuing use of landmark and neurostimulation-guided approaches.
ConclusionsThere is low concordance between the modified Wilson infraclavicular coracoid approach and the use of ultrasound for determining the ideal puncture site; however, no clinical studies have been conducted to assess the success, the need for needle repositioning or the complications of this approach.
Weight and height are independent factors that determine the distance between the coracoid process and the posterior cord in adduction as well as in abduction. The infraclavicular brachial plexus is slightly more superficial and lies closer to the coracoid process in upper limb abduction; there is also variability in the distribution of the cords around the axillary artery in adduction as well as in abduction.
FundingThe authors did not receive sponsorship to undertake this article.
Conflict of interestThe authors have no conflicts of interest to declare.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Pérez-Pradilla AC, Peña-Riverón AA, Chaparro-Gómez LC, Castro-Ortiz LC, Velázquez-Delgado E, Acevedo-de la Peña R. Abordaje infraclavicular en pediatría: concordancia del abordaje de Wilson modificado y el ultrasonido para la localización del sitio de punción ideal. Rev Colomb Anestesiol. 2015;43:269–277.