Target-controlled infusion (TCI) systems allow the administration of drug to achieve a target blood or site-effect concentration. We determine induction and recovery times and the amount of drug used with TCI systems vs. manual induction.
ObjectiveTo determine whether the induction of propofol TCI and manual infusion are two comparable techniques.
MethodsA retrospective observational study was conducted in which sixty-two ASA I–II patients scheduled for elective surgery received induction using TCI or manually. Anaesthetic induction was achieved with remifentanil (0.25μg/kg/min) and propofol (manual bolus injection: 2mg/kg, or target blood concentration: 5μg/ml with the TCI system [Marsh model]) with maintenance doses of remifentanil (0.15μg/kg/min) and propofol (manually 0.10mg/kg/min or 2.5–4μg/ml using the TCI system). In both groups, rocuronium bromide was used (induction and maintenance doses: 0.6 and 0.3mg/kg, respectively) as was morphine (0.1mg/kg) 45min before the end of the surgery.
We measured: induction, operative and recovery mean times; bispectral index, heart rate, blood pressure, costs, haemodynamic instability, and intraoperative awareness. A telephone questionnaire was administered 1 month later.
ResultsThe mean induction time was longer in the TCI than the manual group (1.76±0.94 vs. 0.9±0.4min; p<0.001), but the total dose of propofol (TCI: 112.4±60.9 vs. manual: 133.8±80.3ml, p=0.241) tended to be smaller and the recovery time was significantly shorter (TCI: 7.48±3.1 vs. manual: 10.3±4.9min) (p=0.008).
ConclusionsInduction with propofol using TCI is similar to manually delivered propofol.
los sistemas de infusión controlada por objetivo (TCI) permiten la administración de fármacos para lograr una concentración en sangre de destino o sitio-efecto. Determinamos los tiempos de inducción y recuperación y la cantidad de fármacos que se usa con los sistemas TCI vs inducción manual.
Objetivocomprobar si la inducción de propofol en TCI y la infusión manual son dos técnicas comparables.
MétodosEstudio observacional retrospectivo en el que sesenta y dos pacientes ASA I-II programados para cirugía electiva recibieron inducción manualmente o usando TCI. La inducción de anestesia se logró con remifentanilo (0,25μg/kg/min) y propofol (inyección de bolo Manual: 2mg/kg, o concentración en sangre: 5μg/ml con el sistema TCI [modelo de Marsh]) con dosis de mantenimiento de remifentanilo (0,15μg/kg/min) y propofol (0,10 manualmente mg/kg/min o 2.5–4μg/ml utilizando el sistema de TCI). En ambos grupos, se utilizó bromuro de rocuronio (dosis de inducción y mantenimiento: 0,6 y 0,3mg/kg, respectivamente) así como la morfina (0,1mg/kg) 45 minutos antes del final de la cirugía. Medimos: tiempos medios de inducción, mantenimiento y de recuperación; índice biespectral, la frecuencia cardíaca, la presión arterial, los costes, la inestabilidad hemodinámica y el despertar intraoperatorio. Un cuestionario telefónico se administró 1 mes después.
ResultadosLa media de tiempo de inducción fue mayor en el grupo TCI que en el grupo manual (1,76±0,94 vs. 0,9±0,4min; p<0,001), pero la dosis total de propofol (TCI: 112,4±60,9 vs Manual: 133,8±80,3ml, p=0,241) tendía a ser más pequeña y el tiempo de recuperación fue significativamente más corto (TCI: 7,48±3,1 vs. manual de: 10,3±4,9min) (p=0,008) en el grupo TCI.
Conclusionesinducción de propofol en TCI es comparable a la infusión manual.
Intravenous anaesthetic induction may be performed using several methods: intermittent intravenous infusion, constant-rate intravenous infusion, or using target-controlled infusion (TCI) systems. TCI systems allow drugs to be administered to achieve a target blood or site-effect concentration, the dosage being automatically adjusted by a computer. TCI systems run pharmacokinetic simulations and follow algorithms meaning that the anaesthetist only has to enter patient parameters (age, body weight, height and sex) and the target concentration of the given drug: either an effect-site TCI (concentration in the brain) or blood TCI (target blood concentration).1
There are various pharmacokinetic models for the use of propofol in TCI (Marsh, Schnider and Schuttler,2 among others) while manual infusion can be carried out with or without an initial bolus, though with no bolus it takes a long time to achieve the desired hypnotic effect (approximately 4 or 5 half-lives).1 For use during routine anaesthesia, there are monitors for controlling the level of anaesthesia (hypnosis) based on calculating the bispectral index (BIS), and these allow the titration of drug doses to be adjusted to appropriate levels. The BIS monitor is the only type of device that has been approved by the US Food and Drug Administration (FDA) for assessing the depth of anaesthetic, in order to prevent intraoperative awareness.3
This study was designed to determine induction and recovery times as well as the amount of drug used during propofol induction with TCI systems vs. manual delivery.
Material and methodsThis a retrospective observational study in which a total of 62 ASA I and II patients, aged between 18 and 72 years old scheduled for elective (general) surgery were included. Data collection ran from 1st November 2010 to 15th January 2011. Patients were excluded if they had kidney or liver failure, abused alcohol or other drugs, were under chronic treatment with opioids, or were obese (BMI>30). The Hospital Universitario de Araba ethics committee issued a favorable opinion for the study at the Hospital Universitario de Araba.
Patients were monitored using electrocardiograms, and measuring heart rate, blood pressure (non-invasively), oxygen saturation status, and end-tidal carbon dioxide (EtCO2), as well as BIS values. They received one of the two groups manual or TCI according to anaesthetists criteria. Each group was under the care of two anaesthetists, these always being the same pair of professionals for all the patients in the group. The anaesthetic pump used in both the TCI and the manual induction groups was a Braun Perfusor® Space Infusion System (Melsungen, Germany).
Thirty minutes prior to surgery, all patients were given 7.5mg of oral midazolam as a pre-medication. Total intravenous anaesthesia was induced in all the patients using propofol and remifentanil. In the TCI group, propofol was given according to the Marsh pharmacokinetic model. Anaesthesia was induced with a target blood concentration of 5μg/ml in the TCI group, while a 2mg/kg bolus was given to patients in the manual induction group. The maintenance doses were remifentanil at 0.15μg/kg/min and propofol at 0.1mg/kg/min in the manual induction group and at 2.5–4μg/ml in the TCI group. The infusion was stopped at the end of the surgery.
We used rocuronium bromide for muscle relaxation (induction and maintenance doses of 0.6 and 0.3mg/kg respectively), while for analgesia 0.1mg/kg of morphine was given 45min prior to the end of the surgical procedure. We did not use reversal agents.
After removing the endotracheal tube, patients were transferred to the post-anaesthesia care unit (PACU) for monitoring.
VariablesThe following data were measured: mean times for induction, surgery, and recovery from anaesthesia as well as BIS, heart rate (HR), blood pressure (BP) and whether there was intraoperative awareness. We defined induction time as the period of time between the first dose of the drug and when the BIS decreased to less than 60. Similarly, we defined the mean anaesthesia recovery time as the period of time for the BIS to reach 60 after the last dose of propofol. Finally, we defined hypotension as a reduction of 20% or more from baseline levels and bradycardia as a heart rate of less than 60 beats per minute (bpm).
One month after surgery, a structured questionnaire was administered, always by the same anaesthetist from the research group, to assess the quality of anaesthesia care. The questionnaire consisted of two dichotomous items (yes/no). The questions asked were whether anaesthesia had been satisfactory and whether the patient had had an episode of intraoperative awareness.
Statistical analysisContinuous variables were described using means, standard deviations, and ranges, while qualitative variables were described using frequencies and percentages. Data were analysed using Student's t-tests and Chi square tests for continuous and categorical variables, respectively. Statistical analysis was performed using IBM SPSS V. 20 with the level of statistical significance set at p<0.05.
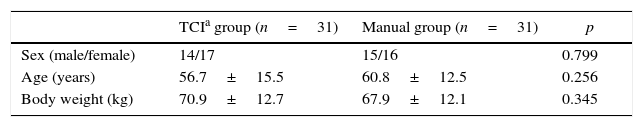
ResultsA total of 62 patients were included in the analysis (31 in each group). The two groups had similar general characteristics (sex, age and body weight), as shown in Table 1.
Comparison of groups by sex, age and body weight.
| TCIa group (n=31) | Manual group (n=31) | p | |
|---|---|---|---|
| Sex (male/female) | 14/17 | 15/16 | 0.799 |
| Age (years) | 56.7±15.5 | 60.8±12.5 | 0.256 |
| Body weight (kg) | 70.9±12.7 | 67.9±12.1 | 0.345 |
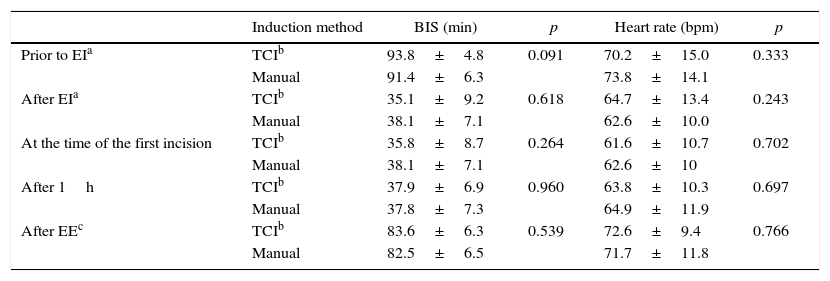
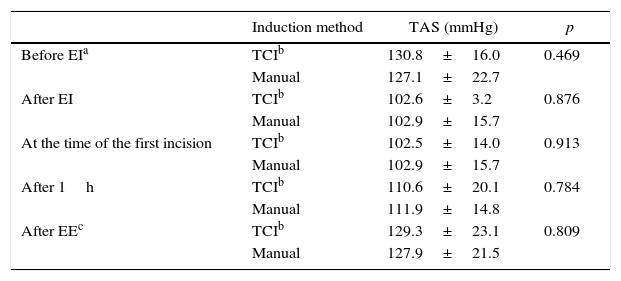
The mean surgery time was similar in the two groups: 130.7±69.7min and 144.9±98.7min for the TCI and manual induction groups respectively (p=0.514). On the other hand, we found statistically (p<0.001) significant differences in the induction time, which was 1.76±0.94 with TCI compared to 0.90±0.4min in the manual induction group, and in the anaesthesia recovery time, which was 7.48±3.1 and 10.3±4.9 in the TCI and manual groups, respectively (p=0.008). Table 2 lists the results concerning BIS and heart rate in the two groups. We did not observe statistically significant differences in either of these variables with the two techniques. Tables 3 and 4 include data corresponding to systolic and diastolic blood pressure.
Comparison of bispectral index (BIS) and heart rate in the TCI and manual induction with the corresponding p-values.
| Induction method | BIS (min) | p | Heart rate (bpm) | p | |
|---|---|---|---|---|---|
| Prior to EIa | TCIb | 93.8±4.8 | 0.091 | 70.2±15.0 | 0.333 |
| Manual | 91.4±6.3 | 73.8±14.1 | |||
| After EIa | TCIb | 35.1±9.2 | 0.618 | 64.7±13.4 | 0.243 |
| Manual | 38.1±7.1 | 62.6±10.0 | |||
| At the time of the first incision | TCIb | 35.8±8.7 | 0.264 | 61.6±10.7 | 0.702 |
| Manual | 38.1±7.1 | 62.6±10 | |||
| After 1h | TCIb | 37.9±6.9 | 0.960 | 63.8±10.3 | 0.697 |
| Manual | 37.8±7.3 | 64.9±11.9 | |||
| After EEc | TCIb | 83.6±6.3 | 0.539 | 72.6±9.4 | 0.766 |
| Manual | 82.5±6.5 | 71.7±11.8 |
Systolic blood pressure of participating patients.
Diastolic blood pressure of participating patients.
The total amount of propofol used in the TCI and manual induction groups was 112.4±60.9ml and 133.8±80.3ml respectively, the difference not being statistically significant (p=0.241). Overall, we detected 41 adverse events of which 27 (65.9%) involved hypotension and 14 (34.1%) bradycardia. Regarding hypotension, there were 7 cases (22.6%) in the TCI group and the other 20 (64.5%) were in the manual induction group (p=0.437), while there were 5 cases of bradycardia (16.1%) in the TCI group, the other 9 (29%) being in the manual induction groups (p=0.224).
QuestionnaireOf the total of 62 patients participating in the study, we managed to contact 24 patients (74.1%) from each group. All those who completed the questionnaire (n=48) stated that the anaesthesia had been satisfactory, while none reported intraoperative awareness.
DiscussionTargeted-controlled infusion with propofol is an alternative to classical manually-delivered induction.4–6 There have been many studies published using TCI systems.7–14 To date, however, there is still no strong evidence to recommend using TCI over manual infusion for propofol induction, according to a Cochrane metanalysis,15 and while some studies have demonstrated greater haemodynamic stability16,17 others have not.18 Recommendations in favour of one or other of the approaches will only be able to be made after further analysis based on data from new studies.
In our study, we observed statistically significant differences in the time of induction and the time of recovery from anaesthesia. Specifically, although the TCI group had longer induction times compared to manual infusion, the time of recovery from anaesthesia was shorter, a pattern that has been reported by other authors.19 After intravenous administration a period of time to onset of clinical effect arises because the blood flow is the pathway through which the effector site is reached. The speed of the blood/brain balance is essential in administering a drug in clinical practice. In manual infusion, a faster effect could occur but waking longer due to inaccurate prediction of propofol effect site concentration and It is not possible to maintain a constant concentration.20
In both groups, the opioid used was remifentanil, since this induction agent does not seem to alter the requirements for propofol in TCI patients,21 the doses used being similar in the two groups to avoid potential interference in our study. We note this in relation to the use of propofol as, although the difference was not statistically significant, we found that the TCI group required less of this hypnotic agent than those receiving manual infusion. Similar findings have recently been reported by Müller et al.22 This is in contrast to the Cochrane review15 carried out before these studies, in which it was found that higher doses of propofol were required with TCI compared to manual infusion.
Anaesthetic monitoring using the BIS during propofol infusion can result in safer anaesthesia.19 In our study, BIS values before endotracheal intubation, after the first surgical incision, 1h after surgery and after endotracheal extubation were similar in the two groups, the differences not being significant.
The greatest problem with manual induction is the dose-dependent haemodynamic response.1 In our study, we detected a more episodes of bradycardia and hypotension in the manual induction group, but the difference was not statistically significant. The haemodynamic parameters of heart rate and blood pressure before and after endotracheal intubation, after the first surgical incision, 1h after the start of the surgery and after endotracheal extubation were similar in the two groups (no statistically significant differences).
The administration of higher concentrations of propofol may decrease the likelihood of anaesthetic awareness, however, lead to an increased risk of haemodynamic side effects.23
With regard to the quality of the anaesthesia, we found no differences between the groups using our questionnaire; notably, there were no episodes of intraoperative awareness with either of the techniques.
Limitations: TCI devices for propofol that use the Marsh mode that considering only weight, it is possible that the bias associated with use of this device could lead to overdosage when it is used in obese patients.24 The retrospective observational study generally requires a large sample size. The team does not control the study factor, merely to observe, measure and analyse. Selection bias is a fundamental problem of retrospective studies and for the avoidance of selection bias depends largely on the researcher knows the sources of potential bias. The design of an observational study influences the statistical power, it is optimal to have the same number of observations of the two populations being compared (provided that variations in the two populations are the same).
In our study, all patients received the same drug at the same dose preoperatively (midazolam) so premedication was not a confounding factor, it having a similar effect on the propofol concentration in both groups.25 Further, sex, age and body weight could not be responsible for bias in the analysis as the groups were well-matched in terms of these characteristics.
Relative to the pharmacokinetic model, there are two different models (Marsh and Schnider) for the administration of total intravenous anaesthesia with propofol. According to a recent study,26 both pharmacokinetic models are equivalent in terms of stability of depth of anaesthesia.
In conclusion, induction with propofol using TIC is similar to manually delivered propofol, though the anaesthesia recovery time was statistically significantly shorter in the TCI group.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo external funding was received.
Conflicts of interestThe authors have not conflicts of interest to declare.
Please cite this article as: Laso LF, Picado AL, de La Fuente EO, Murua AM, Castro CS, Ruilope LP, et al. Inducción con propofol: infusión controlada por objetivo o manual. Un estudio observacional. Rev Colomb Anestesiol. 2016;44:272–277.