The first case of idiopathic pregabalin-induced toxicity in Latin America is reported in a patient with radicular pain secondary to lumbar spinal stenosis, who presented with jaundice and elevation of liver enzymes, associated with the use of pregabalin. A diagnosis of drug-induced liver injury was made. Liver function was normalized once the drug was discontinued without any sequelae. It is important to be aware of the potential hepatic toxic effects of pregabalin, despite the fact that the drug shows no evidence of liver metabolism and liver toxicity is very unusual. The liver injury mostly resolves upon pregabalin removal.
Se reporta el primer caso de toxicidad idiosincrática inducida por pregabalina en Latinoamérica, en un paciente con dolor radicular secundario a canal lumbar estrecho, el cual se presentó con ictericia y elevación de enzimas hepáticas, asociada al uso de pregabalina. Se hace diagnóstico de lesión hepática inducida por drogas. La función hepática se normalizo una vez se suspendió el medicamento sin dejar ninguna secuela. Es importante tener en cuenta que la pregabalina puede tener efectos tóxicos severos a nivel hepático, a pesar de no tener metabolismo evidente a este nivel y ser muy poco frecuente, en la mayoría de casos la lesión hepática resuelve al suspender la pregabalina.
At least 6 cases of acute liver disease secondary to the use of pregabalin have been reported worldwide.1–6 No cases of liver toxicity associated to the drug had been so far reported in Latin America so this is the first report. In this case, the evolution was similar to the cases previously reported. After 8 days of continued use of pregabalin 75mg every 12h, the patient presented jaundice associated with a significant elevation of liver transaminases that were normalized a few days after interrupting the use of the medication, with no evidence of sequelae.
Patient informationA 53-year old male patient, farmer living in a rural area, who presented at the emergency department due to severe lumbar pain for 3 days (VAS 10/10). The pain irradiated to the lower right limb, and was associated with a loss of strength of the extremity after manipulation of a heavy object. The patient self-medicated with diclofenac and acetaminophen with no pain relief, resulting in his visit to the ER. The patient's history included hypertension treated and controlled with losartan 50mg every 12h, type II diabetes mellitus treated and controlled with vildagliptin 50 mg-metformin hydrochloride 850mg. The patient is an occasional user of alcoholic drinks, with no relevant infections, surgical or family history.
Clinical findingsThe physical examination showed nerve root signs, positive right Lasegue's sign, positive right Bragard's, and loss of strength in the same extremity. The diagnosis was mixed severe acute lumbar pain requiring further study, controlled high-blood pressure and controlled type II diabetes mellitus. On day 12 of hospitalization the patient presented clinical signs of jaundice and paraclinical tests were done (see Table 1). Pregabalin-induced liver injury was suggested, in the absence of any other associated causes. 3 days after stopping the use of the medication, the jaundice resolved with no apparent sequelae at the time of hospital discharge, or during the following visits over the next 6 months.
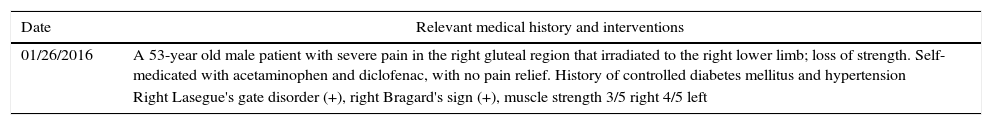
Timeline: calendar.
| Date | Relevant medical history and interventions |
|---|---|
| 01/26/2016 | A 53-year old male patient with severe pain in the right gluteal region that irradiated to the right lower limb; loss of strength. Self-medicated with acetaminophen and diclofenac, with no pain relief. History of controlled diabetes mellitus and hypertension |
| Right Lasegue's gate disorder (+), right Bragard's sign (+), muscle strength 3/5 right 4/5 left |
| Date | Clinical evolution | Diagnostic tests | Interventions |
|---|---|---|---|
| 01/26/2016 | Lumbosacral spine X-rays: space narrowing of L4–L5, antalgic scoliosis | Diazepam, dipyrone, ranitidine, losartan, vildagliptine-metformin | |
| 01/28/2016 | Pain persists | TGO/ASAT 10.4, TGP/ALAT 23.1, total bilirubin 1.01, direct 0.36, indirect 0.05, alkaline phosphatase 58, blood glucose 178mg/dl | |
| 01/29/2016 | Clinical evaluation pain. Difficult to manage pain | Lumbar MRI: compressive L2–L3 disc hernia, right foramen stenosis, changes in facet joint osteoarthritis. Spondylolisthesis L4–L5 | Removal of diazepam and dipiyone |
| 01/30/2016 | Pregabalin 75mgc/12h, tramadol 50mgc/8h | ||
| 02/01/2016 | Glycemia 129.8, bun 20.2, calcium 1.17, sodium 136, potassium 4.18, chlorine 101.1, PCR 0.19, hemoglobin 16, hematocrit 44.7 leukocytes 7.100, PT 11.8, PTT 36.2 | ||
| 02/04/2016 | Pain persists. Neurosurgical team decides in favor of surgical management | ||
| 02/05/2016 | The patient undergoes lumbar L2–L5 spinal instrumentation and L2 right laminectomy | ||
| 02/07/2016 | Jaundice develops | TGO/ASAT 480, TGP/ALAT 1012.5, total bilirubin 0.58, direct 0.22, indirect 0.36, lactic dehydrogenase 415, hemoglobin 11, hematocrit 33.8, leukocytes 8.800 | |
| 02/08/2016 | Diagnosis of drug-induced hepatitis | Pregabalin is removed | |
| 02/10/2016 | Jaundice resolves | TGO/ASAT 49.9, TGO/ALAT 348.9 | |
| 02/13/2016 | Postoperative pain control. Hospital discharge |
Imaging studies: lumbosacral spine X-rays: L4–L5 space narrowing, antalgic scoliosis, and lumbar MRI evidencing L2–L3 compressive disc hernia with stenosis of the right foramen, changes in facet joints arthrosis, and spondylolisthesis L4–L5.
Pre-surgical testing was done: TGO/ASAT 10.4U/l (reference value 0–32U/l), TGP/ALAT 23.1U/l (reference value 0–41U/l), total bilirubin 1.01mg/dl (direct 0.36mg/dl, indirect 0.65mg/dl), alkaline phosphatase 58U/l, glycaemia 129mg/dl, BUN 20.2mg/dl, creatinine 0.77mg/dl, sodium 136.1meq/dl, potassium 4.18meq/dl, chlorine 101.1meq/dl, prothrombin time (PT) of 11.8s, INR 0.84, partial thromboplastine time (PTT) of 36.2s and blood count within the normal limits. All tests were within the normal range, with no evidence of liver dysfunction. On day 12 of hospitalization the patient presents jaundice and new liver tests were ordered: TGO/ASAT 480U/l TGP/ALAT 1012.5U/l, total bilirubin 0.58mg/dl (direct 0.22mg/dl, indirect 0.36mg/dl), lactic dehydrogenase 415U/l (reference value 280–480U/l), blood test within the normal limits. There were no economic, language, or cultural barriers for the diagnosis. Based on these results, a diagnosis of drug-associated hepatitis was made, ruling out infectious hepatitis since no evidence of fever, hepatomegaly, or relevant blood test changes was found. Possibly the hepatitis was secondary to the use of pregabalin and the drug was immediately removed. There is progressive jaundice improvement and 3 days later the patient undergoes hepatic enzymes control with the following results: TGO/ASAT 49U/l TGP/ALAT 348U/l, thus confirming drug related hepatitis, secondary to the use of pregabalin. Afterwards the patient evolves with no evidence of liver or other sequelae until the time of discharge, with a significant reduction in liver enzymes and resolution of jaundice.
Therapeutic interventionMedical management was introduced with intravenous diclofenac every 12h and IV tramadol 50mg every 8h, with rescue doses of 25mg between doses. In view of the pain severity and poor analgesic regime response, an interconsultation with the pain management service resulted in the additional prescription of pregabalin 75mg every 12h on day 4 of hospitalization, while waiting for the decision of the surgical team to define the approach. The persistence of severe pain lead to exploration and decompression of the L2–L3 canal with posterior arthrodesis of the lumbar spine on day 9 of hospitalization with no major complications. After 8 days of continued use of pregabalin, the decision was made to remove the drug as the potential etiological agent of the drug-associated hepatitis. Clinical and paraclinical improvement was observed.
Follow-up and resultsThe pre-surgical tests indicate that the patient's liver function was normal at admission and his baseline pathologies were controlled. The lumbar MRI clearly established the etiology of the patient's pain, which based on its severity and refractory management required a surgical approach. The quite significant elevation of the hepatic transaminases, particularly TGP/ALAT (that increased over 40 times its initial value) showed the presence of a liver inflammatory injury. Such injury was associated with the use of pregabalin, since upon removal of the drug, the transaminase levels experienced a positive response.
DiscussionPregabalin is an FDA approved medication for managing pain associated with diabetic neuropathy, post-herpetic neuralgia, as adjuvant therapy in the management of partial convulsive crisis in adults, management of fibromyalgia, and neuropathic pain associated with spinal cord injuries. Pregabalin is a neuromodulator with high affinity for the alpha-2-delta subunit of voltage-gated calcium channels in the central nervous system. It limits the inflow of this ion and of any ion-dependent ionic flows; it also inhibits the release of pain-associated mediators such as noradrenalin, substance P and glutamate, which accounts for its clinical effectiveness in the treatment of pain. The liver metabolism of pregabalin is practically negligible; it does not induce or inhibit any liver enzymes. Two irrelevant residues are produced during pregabalin metabolism: a N-methylated metabolite equivalent to 0.9%, and an undefined element representing 0.4%, of the pregabalin dose administered. Whether these residues have any organic action is yet to be determined. No pregabalin activity has been defined with regards to the cytochrome complex enzymes.7
In this particular patient pregabalin was directly involved in the liver injury. The patient developed jaundice with elevation of the hepatic enzymes – TGP/ALAT 43-fold increase and TGO/ASAT over 4-fold increase, after 8 days of pregabalin use. There were no clinical or paraclinical findings suggesting a different etiology. One strong point in this case was the early diagnosis which led to the removal of the drug preventing any significant sequelae. However, an important limitation was failure to do continuous follow-up of the transaminases until these were completely normalized.
The drug-associated acute liver injury may be classified as an idiosyncratic hepatocyte injury. A causal assessment of the clinical presentation based on Roussel Uclaf model (RUCAM)8 resulted in a high probability.
Similar to the cases reported, this particular case evidences the time-dependent association between the onset of pregabalin treatment and the liver injury symptoms. Usually these symptoms present between the first week and up to 4 months of uninterrupted use. Just as in other cases reported in the literature, the liver function recovered to a normal condition upon discontinuation of the drug. The absence of a rise in the bilirubin levels was intriguing, but probably due to the early diagnosis and immediate removal of the medication. It should be stressed that although pregabalin is not metabolized through the liver, the potential for liver toxicity must not be ruled out, as has been described in acute liver injuries associated with pregabalin. This neuromodulator must be considered a drug that on rare occasions may cause acute idiosyncratic liver failure.
Patient perspectiveThe patient clearly understood his idiosyncratic reaction to pregabalin, understood that despite obtaining better pain control during his hospitalization, this medication caused changes in his liver function and hence since then, the patient has emphatically informed his doctors that he must not take pregabalin due to the risk of developing severe liver injury.
Informed consentThe patient provided his informed consent to publish this case report.
Ethical disclosuresProtection of human and animal subjectsThe author declares that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe author declares that no patient data appear in this article.
Right to privacy and informed consentThe author declares that no patient data appear in this article.
FundingThis paper was funded with the author's own resources.
Conflicts of interestThe author has no conflicts of interest to declare.
Please cite this article as: Quintero-Castellanos M. Lesión hepática inducida por el uso de pregabalina. Reporte de Caso. Rev Colomb Anestesiol. 2017;45:349–352.