The intensive care unit (ICU) physician should have the skill to successfully manage patients requiring airway insulation on account of their poor ventilatory condition. The purpose of this article is to review the current knowledge regarding rapid sequence intubation in the ICU patients and to summarize the procedure to maximally reduce the risks of intubating a critical patient.
MethodsTheme Review. An e-search of databases was performed, including PubMed, ScienceDirect, EBSCOhost, OvidSP and Scielo, without limiting the search by date, in English and Spanish. These include clinical trials, meta-analysis, practicing guidelines, randomized controlled trials, reviews, case reports, classical articles, comparative studies, consensus conferences and keynote speeches. Published articles on intubation, rapid sequence intubation and ICU intubation were included, all focusing on orotracheal intubation of the critical patient and strategies for optimization of the maneuver.
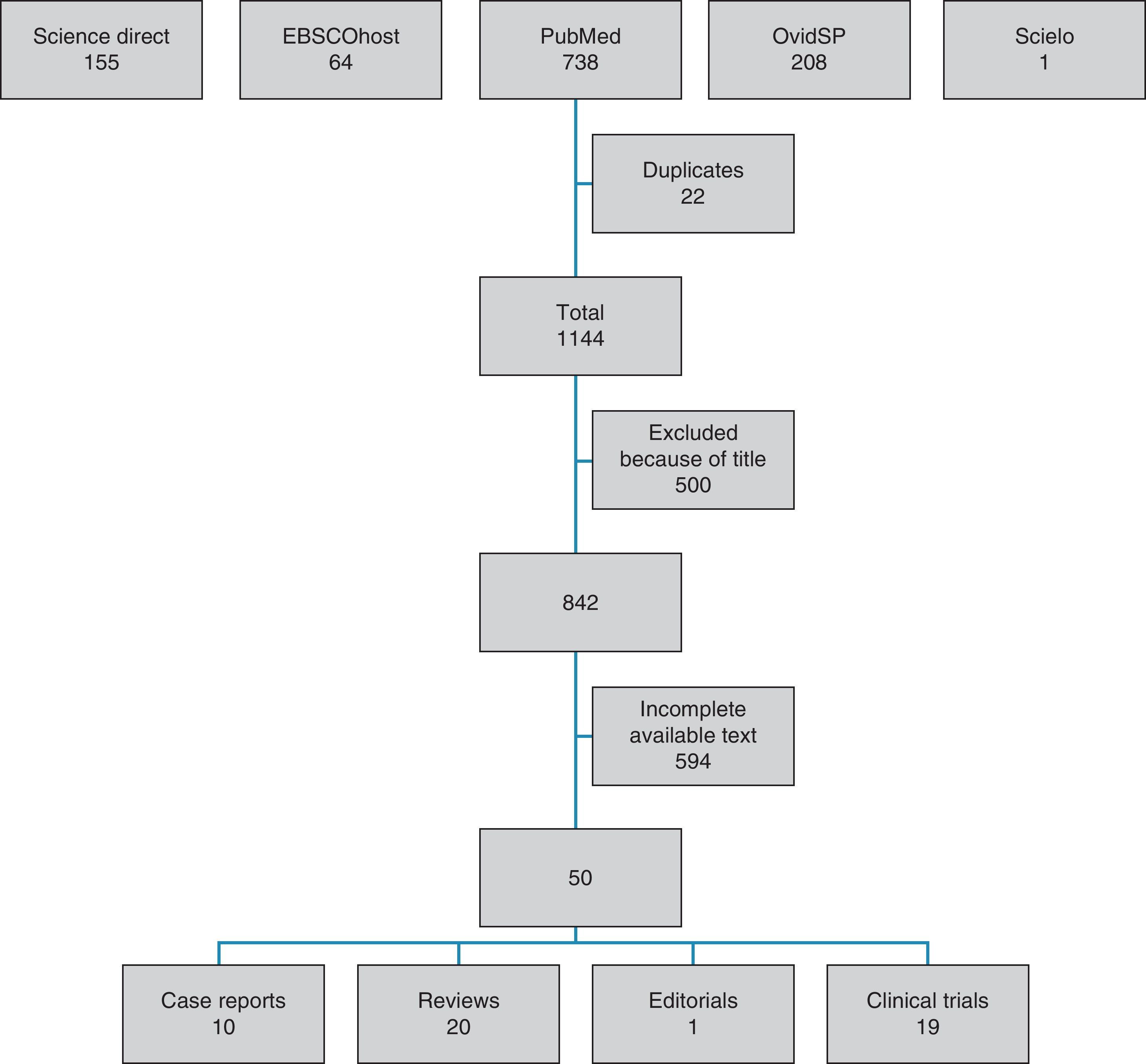
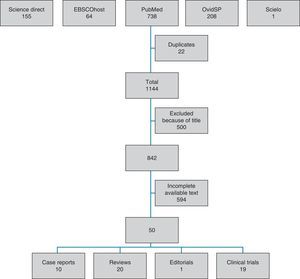
ResultsThe search yielded 1144 studies. The abstracts were reviewed and those referring to the key review criteria were chosen: intubation protocols for ICU patients. Fifty monographs met the selection criteria. A summarized presentation of the results is made and an approach to a modified rapid sequence intubation is suggested, based on the review accomplished.
El médico que trabaja en cuidados intensivos debe tener la habilidad para enfrentarse con éxito a los pacientes que necesitan aislamiento de la vía aérea debido a su pobre condición ventilatoria. El objetivo del presente artículo es revisar el estado actual del conocimiento en torno a la intubación de secuencia rápida en pacientes de la unidad de cuidados intensivos (UCI) y resumir lo que se debe hacer para reducir al máximo los riesgos durante la intubación de un paciente crítico.
MétodosRevisión temática. Se realizó una búsqueda electrónica en las bases de datos PubMed, ScienceDirect, EBSCOhost, OvidSP y Scielo, sin limitar la búsqueda por fecha en inglés y español. Se incluyeron ensayos clínicos, metaanálisis, guías para la práctica, ensayos controlados aleatorizados, revisiones, reportes de casos, artículos clásicos, estudios comparativos, conferencias de consenso y clases magistrales. Se incluyeron artículos publicados sobre intubación, intubación de secuencia rápida e intubación en UCI cuyo tema central fuese el abordaje de la vía aérea con tubo orotraqueal del paciente crítico, y las estrategias para optimizar la maniobra.
ResultadosLa búsqueda arrojó 1.144 estudios. Se revisaron los resúmenes y se seleccionaron los que trataban sobre los criterios centrales de la revisión: protocolos de intubación para los pacientes de la UCI. Cincuenta monografías cumplieron los criterios de selección. Se hace una presentación resumida de los resultados y se propone una versión de intubación de secuencia rápida modificada a partir de la revisión hecha.
The first records about airway approach were found in Egyptian tablets dating back to 3600 b.c. illustrating sketches of what seemed to be a tracheostomy. Over three thousand years later, Alexander the Great saved one of his soldiers from asphyxia by making a small tracheal incision with the tip of his spade. In 1858, Eugene Bouchut, a French pediatrician, developed a non-surgical blind orotracheal intubation technique: he developed a metal tube to enable breathing and prevent the obstruction of the pseudomembranes caused by diphtheria in the larynx. His technique was introduced at the Conference of the French Academy of Sciences in September 18, 1858 and was strongly opposed by the French surgeon Armand Trousseau, who promoted tracheostomy for airway obstruction. Trousseau was the first surgeon to perform tracheostomies in Paris and who wrote a treaty encouraging its use.1
The goal of this paper is to review the current status of knowledge related to rapid sequence intubation in patients in the Intensive Care Unit, and to summarize what needs to be done in order to reduce risks during intubation of a critically ill patient to the greatest extent possible. A thematic review was done in the PubMed, ScienceDirect, EBSCOhost, OvidSP and Scielo databases, without limiting the search by date, either in English or Spanish. The search included clinical trials, meta-analyses, practice guidelines, randomized clinical trials, reviews, case reports, classic articles, comparative studies, consensus conferences and lectures. Published articles on intubation, rapid sequence intubation and ICU intubation that focused on the approach to the airway with orotracheal tube in critically ill patients and the strategies for optimizing the maneuver, were included. The search resulted in 1,144 studies (Fig. 1). The abstracts were reviewed and the core criteria of the review were used for the final selection, namely, intubation protocols for ICU patients. Fifty essays fulfilled the selection criteria (Table 1). The results are summarized, and a modified rapid sequence intubation sequence is proposed on the basis of the review.
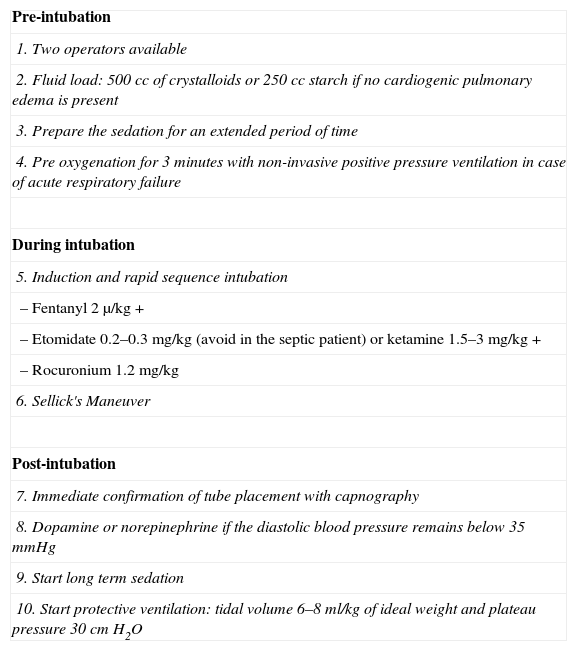
Summary of articles selected for review.
| Trial | Design | Year | Results |
| 1. Trousseau A: Du tubage de la glotte et de la tracheotomie, par M Bouchut. | Case Report | 1858 | NA |
| 2. Garcia M: Observations on the human voice. Proc R Soc Lond 1854; 7:399–410. | Case Report | 1854 | NA |
| 3. von Esmarch F: Handbuch der Kriegschirurgischen Technik. Hannover, Germany, Carl Rumpler, 1877. | Case Report | 1877 | NA |
| 4. Kirstein A: Autoskopie des Larynx und der Trachea. Berl Klin Wochenschr 1895; 32:476–478. | Case Report | 1895 | NA |
| 5. Killian G: Ueber directe Brochoskopie. Munch Med Wochenschr 1898; 45:844–847. | Case Report | 1898 | NA |
| 6. Jaber. An intervention to decrease complications related to endotracheal intubation in the intensive care unit. | Prospective, multicenter | 2009 | The implementation of management protocols may limit the complications associated with intubation in the ICU |
| 7. Schmidt. Effects of supervision by attending anesthesiologists on complications of emergency tracheal intubation. | Prospective, cohort trial | 2008 | Trainer surveillance significantly reduced the complications during intubation |
| 8. Vincent JL. Yearbook of Intensive Care and Emergency Medicine. | Textbook | 2009 | Volume expansion prevents the collapse of the critical patient during intubation |
| 9. Miller R. Miller's Anesthesia. 7th ed. United States of America: Elsevier; 2010 | Textbook | 2010 | Pre-oxygenation is required prior to the laryngoscopy maneuver |
| 10. Weiler N. Assessment of pulmonary mechanics and gastric inflation pressure during mask ventilation. | Series of cases | 1995 | Inspiratory pressure should be limited to 20cm H2O |
| 11. Clements P. Should patients be manually ventilated during rapid sequence induction of anaesthesia? | Review | 2009 | Experienced practitioners may ventilate the patient with positive pressure during rapid sequence intubation |
| 12. Henderson JJ. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. | Review | 2004 | Positive pressure ventilation should be considered in difficult airway patients |
| 13. El-Orbany M. Rapid sequence induction and intubation: current controversy. | Review | 2010 | There is some controversy regarding the ideal strategy for rapid sequence intubation – induction |
| 14. Baillard. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. | Randomized, prospective | 2006 | Facial mask pre-oxygenation was superior to conventional pre-oxygenation |
| 15. Stept WJ. Rapid induction–intubation for prevention of gastric-content aspiration. | Series of Cases | 1970 | The rapid sequence induction – intubation protocol prevents gastric aspiration |
| 16. Dobson AP. Effective time to satisfactory intubation conditions after administration of rocuronium in adults. Comparison of propofol and thiopentone for rapid sequence induction of anaesthesia. | Randomized, prospective | 1999 | Rocuronium used in propofol induction is an alternative to succinylcholine in rapid sequence induction – intubation |
| 17. White PF. Comparative evaluation of intravenous agents for rapid sequence induction – thiopental, ketamine, and midazolam. | Randomized, prospective | 1982 | Midazolam or midazolam-ketamine are safe and effective for induction |
| 18. Yeung. A review of etomidate for rapid sequence intubation in the emergency department. | Review | 2002 | Of all the available induction agents, etomidate provides the most favorable safety profile |
| 19. Dean P. Should etomidate be used for rapid-sequence intubation induction in critically ill septic patients? Probably not. | Review | 2008 | Etomidate may lead to adrenal failure in the septic patient |
| 20. Werther JR. Ketamine anesthesia. | Review | 1985 | Ketamine rises the intracranial pressure |
| 21. Barr. Thiopentone and suxamethonium crash induction. An assessment of the potential hazards. | Case Series | 1976 | Cricoid pressure was effective in preventing regurgitation |
| 22. El-Orbany. The neuromuscular effects and tracheal intubation conditions after small doses of succinylcholine. | Randomized, prospective | 2004 | A dose of 0.6mg/kg of succinylcholine resulted in identical intubation conditions to a 1 mg/kg |
| 23. Seupaul. Evidence-based emergency medicine. Does succinylcholine maximize intubating conditions better than rocuronium for rapid sequence intubation? | Systematic review | 2011 | Succinylcholine is superior to rocuronium in terms of providing excellent intubation conditions |
| 24. Martyn. Succinylcholine-induced hyperkalemia in acquired pathologic states: etiologic factors and molecular mechanisms. | Review | 2006 | Succinylcholine may induce fatal hyperkalemia in certain pathological conditions |
| 25. Dodson. Changes in acetylcholine receptor number in muscle from critically ill patients receiving muscle relaxants: An investigation of the molecular mechanism of prolonged paralysis. | Prospective trial | 1995 | Denervated patients may require higher doses of muscle relaxants due to a stronger presence of cholinergic receptors |
| 26. Walz. Airway management in critical illness. | Review | 2007 | The airway approach may be complicated due to multiple factors limiting the physiological reserve |
| 27. Jones. Anaesthesia and demyelinating disease. | Review | 1980 | In demyelinating disease, succinylcholine induces considerable hyperkalemia |
| 28. Cooperman. Succinylcholine-induced hyperkalemia in neuromuscular disease. | Review | 1970 | Succinylcholine causes hyperkalemia in neuromuscular disease |
| 29. Leiman. Mechanisms of succinylcholine-induced arrhythmias in hypoxic or hypoxic: hypercarbic dogs. | Review | 1987 | Succinylcholine induces arrhythmia due to sympathetic stimulation |
| 30. Sluga. Rocuronium versus succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. | Randomized, prospective | 2005 | Succinylcholine creates better intubation conditions and more expeditiously |
| 31. Andrews. A large simple randomized trial of rocuronium versus succinylcholine in rapid-sequence induction of anaesthesia along with propofol. | Randomized, prospective | 1999 | Rocuronium at 1mg/kg is equivalent to succinylcholine in the rapid induction – intubation sequence |
| 32. Patanwala. Comparison of succinylcholine and rocuronium for first-attempt intubation success in the emergency department. | Randomized, prospective | 2011 | Succinylcholine and rocuronium are equivalent in first-attempt intubation success |
| 33. Harris. Effects of thiopentone, etomidate and propofol on the hemodynamic response to tracheal intubation. | Randomized, prospective | 1988 | Propofol caused a significant blood pressure when used as a hypnotic agent, while etomidate caused an opposite response |
| 34. Miller. Effects of alfentanil on the hemodynamic and catecholamine response to tracheal intubation. | Randomized, placebo controlled, double blind | 1993 | Alfentanil controls the systolic pressure response, pulse and systemic vascular resistance to intubation |
| 35. O’Hare. Bolus dose remifentanil for control of haemodynamic response to tracheal intubation during rapid sequence induction of anaesthesia. | Randomized, placebo controlled, double blind | 1999 | A dose of 1 and 1.25μg/kg of remifentanyl prior to intubation effectively controlled the blood pressure and pulse elevation |
| 36. Palencia-Herrejón; Grupo de Trabajo de Analgesia y Sedación de la SEMICYUC. [Intubation of the critical patient]. | Review | 2008 | Fentanyl provides hemodynamic stability during induction – intubation |
| 37. Vanner. Safe use of cricoid pressure. | Review | 1999 | The correct use of cricoid pressure reduces the incidence of pulmonary aspiration without hindering the tracheal intubation |
| 38. Robinson. Fatal aspiration (Mendelson's) syndrome despite antacids and cricoid pressure. | Case series | 1979 | Pulmonary aspiration may occur despite the correct implementation of Sellick's maneuver |
| 39. Williamson. Cricoid pressure. | Editorial | 1989 | The idea that Sellick's maneuver is simple should not be encouraged |
| 40. Haslam. Effect of cricoid pressure on the view at laryngoscopy. | Case series | 2005 | Applying a 30N force on the throat may obscure the vision of the laryngoscopist |
| 41. Grmec. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. | Prospective | 2002 | Capnography is the most reliable method in the pre hospital environment to confirm the adequate placement of the endotracheal tube |
| 42. Silvestri. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. | Prospective, observational | 2005 | Continuous capnography monitoring was not associated with unrecognized misplaced intubation |
| 43. Neumar. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. | Systematic review | 2010 | Capnography should be used to confirm a successful intubation |
| 44. Nolan. Part 1: executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. | Systematic review | 2010 | Capnography should be used to confirm a successful intubation |
| 45. Havel. Vasopressors for hypotensive shock. | Systematic review | 2011 | There are no long term differences among vasopressors for correcting the hypertensive shock |
| 46. De Backer. Comparison of dopamine and norepinephrine in the treatment of shock. | Randomized, prospective | 2010 | Dopamine was associated to more adverse events |
| 47. Petrucci. Lung protective ventilation strategy for the acute respiratory distress syndrome. | Systematic review | 2007 | Mortality was lower at 28 d with the protective pulmonary ventilation techniques |
| 48. Amato. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. | Randomized, prospective | 1998 | The protective strategy was associated to lower 28 d mortality, higher extubation success and lower barotrauma in adult respiratory distress patients |
| 49. Ranieri. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. | Randomized, prospective controlled | 1999 | Cytokines response to mechanical ventilation is minimized with pulmonary over-distention |
| 50. Brower. Prospective, randomized controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. | Randomized, prospective controlled | 1999 | There were no significant differences among patients using low tidal volumes as compared to those using the traditional volumes |
Prior to the advent of the modern laryngoscope, the only way to visualize the larynx was through indirect techniques: the Spanish singing professor Manuel García (1805–1868) used mirrors to observe his glottis and the glottis of his students during vocalization.2 Around 1877, Friedrich von Esmarch popularized the mandibular subluxation maneuver for patency of the airway, as we actually know it.3 In 1895 Alfred Kirstein suggested that the larynx could be visualized through instruments similar to the esophagoscope4; three years later, Gustav Killian developed a laryngoscope similar to those currently used,5 and it became widely used to met the need of ensuring patency for the inflow of air into the lungs due to the increasing use of muscle relaxants.
The rapid sequence intubation (RSI) is a technique developed to rapidly secure the airway, maximally reducing the time interval between the loss of the airway protective reflexes and the oro/nasotracheal intubation. Its importance lies in providing a safe intubation in patients at high risk of bronchoaspiration.
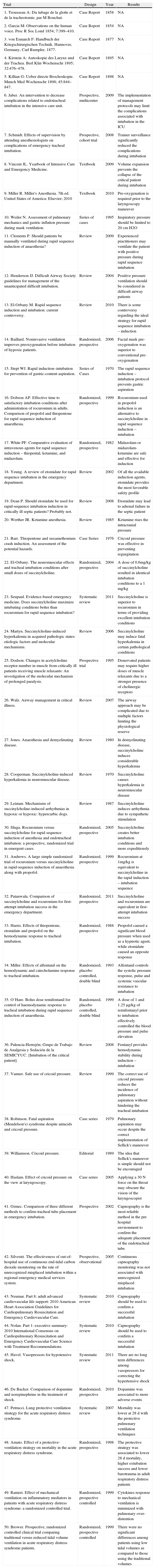
In 2010 Jaber et al.6 published a study using a “before-after” model to compare the results of implementing an intubation protocol for ICU patients. The main complications of intubation – cardiovascular collapse and hypoxemia – were cut in half in the intervention group. According to the research it can be concluded that the protocols, conceived as orderly and sequential actions, as is the case in cardiovascular resuscitation, also improve morbi-mortality of the critical patient requiring intubation. Its protocol includes 10 steps (Table 2).
Suggested steps for rapid sequential intubation of the critical patient.
| Pre-intubation |
| 1. Two operators present |
| 2. Fluid load: 500cc of crystalloids or 250cc starch in the absence of cardiogenic pulmonary edema |
| 3. Prepare sedation for an extended period of time |
| 4. Minute pre-oxygenation with non invasive positive pressure ventilation in case of acute respiratory failure |
| During intubation |
| 5. Induction and rapid sequence intubation: |
| – Etomidate 0.2–0.3mg/kg or ketamine 1.5–3mg/kg + |
| – Succinylcholine 1–1.5mg/kg (avoid its use in allergic, hyperkalemic or severely acidotic patients, in patients with acute or chronic neuromuscular disease or in burned patients with over 48hours of evolution or spinal trauma) |
| 6. Sellick's Maneuver |
| Post-intubation |
| 7. Immediate confirmation of tube placement using capnography |
| 8. Norepinephrine when blood systolic pressure remains below 35mmHg |
| 9. Start long term sedation |
| 10. Start protective ventilation: tidal volume 6–8ml/kg of ideal weight, PEEP<5cm H2O and respiratory rate between 12 and 20cycles/min, FIO2100% and plateau pressure 30cm H2O |
We shall now review the levels of evidence for each one of these recommendations.
Two operators presentThe short time available in the ICU and the critical scenario make it difficult to properly assess the airway. The presence of a senior physician next to the person doing the intubation has proven to reduce the complications associated with the procedure: esophageal intubation (0.9% vs. 3.4%), traumatic intubation (1.7% vs. 6.8%), bronchoaspiration (0.9% vs. 5.8%), teeth damage (0% vs. 1.0%) and selective intubation (2.6% vs. 7.2%). The global rate of complications also decreased significantly (6.1% vs. 21.7%, p<0.0001).7
Volume expansionThere is no evidence to date of the administration of a fluid bolus prior to intubation; however, it is logical to think that this could be beneficial for the critical patient pre-intubation – except for patients with cardiogenic pulmonary edema – due to the following reasons: (1) usually the patient is hypovolemic and (2) anesthetic agents block the sympathetic response that maintains the hemodynamic variables against hypotensive stimuli; and (3) mechanical ventilation reduces the cardiac output when compromising the preload.8
Pre-oxygenationDuring pre-oxygenation, the nitrogen contained in the pulmonary alveoli is exchanged by oxygen, providing the patient with an additional oxygen reserve; hence, maneuvers such as laryngoscopy and intubation may be done avoiding deoxygenation. 100% oxygen is supplied through the face mask: if the patient's awareness permits, he/she is asked to breath deeply for ninety seconds or, oxygen is passively supplied for three minutes.9
It has been usually argued that during RSI positive pressure ventilation (PPV) should be avoided because gastric insufflation favors bronchoaspiration.10 However, after August 19, 1961 when Sellick published his famous cricoid pressure maneuver to avoid regurgitation of the gastric contents during the induction of anesthesia, the recommendations state in a footnote that experienced practitioners may administer PPV, if the inspiratory pressure does not exceed 20cm H2O.11,12 Moreover, there are certain cases in which PPV prior to intubation, within the context of RSI, is strongly recommended: obese patient, pregnant women, pediatric patient and critically ill patients.13 A recent clinical study in 53 patients showed that pressure-supported non-invasive ventilation, as a pre-oxygenation method, was more effective than non-inhalation ventilation mask and reserve bag.14
Induction and rapid sequence intubationStept and Safar published in July 1970 the iconic protocol for induction – intubation to prevent gastric aspiration.15 The key objective of the rapid sequence intubation technique is to reduce the period of time between loosing the airway protective reflexes and the intubation with an oro/nasotracheal tube with pneumatic plugging sleeve.16 The technique was intended for patients at high risk of aspiration.
The original algorithm considers the administration of a predetermined intravenous dose of sodium thiopental (150μg), followed by the immediate administration of succinylcholine (100mg), establishing intubation conditions in less than one minute.15 Sodium thiopental acts as a hypnotic agent, while succinylcholine relaxes the adductor laryngeal muscles.
There has been considerable controversy about the best hypnotic agent for RSI. Two aspects should then be considered: (1) intubation conditions and (2) hemodynamic variability. Dobson et al.16 compared thiopental and rocuronium vs. propofol and rocuronium, and found better intubation conditions with propofol, apparently due to propofol's enhanced effectiveness to inhibit the pharyngeal and laryngeal reflexes.
It should be kept in mind that the ideal hypnotic agent for an ICU patient is one that leads to minimum change in the hemodynamic parameters; however, contrary to our objectives, thiopental and propofol, cause marked hypotension. Etomidate and ketamine are effective hypnotic agents in patients hemodynamically compromised,17,18 and hence are the agents of choice in ICU patients. Please keep in mind that etomidete's ability to induce adrenal failure and thus its use is contraindicated in septic patients.19 Likewise, ketamine should not be used in patients with elevated intraocular pressure or in patients with space occupying lesions due to its known effect of raising the intracranial pressure.20
Should you administer a predetermined fixed dose of the hypnotic agent (as suggested by Stept and Safar in their original paper) or, on the contrary should the agent be titrated until loss of consciousness is obtained? With the former approach there is a risk of under or over-dosing the patient allowing the patient to be conscious or inducing drastic hemodynamic changes with the latter.13 In both cases, the muscle relaxant is administered upon loss of consciousness. Those who are against of the titration technique claim that the induction last longer as compared to the classic technique; however, some authors like Barr and Thornley21 have shown that while total induction time is longer, the period of time between loss of consciousness and intubation remains unchanged.
In the RSI puzzle, succinylcholine is the key player: why? What makes succinylcholine so special? Studies show that when succinylcholine is used in RSI protocols, identical intubation conditions are achieved, regardless of the hypnotic agent selected.22 A recent systematic review by Cochrane evidences that succinylcholine is superior to rocuronium to create excellent intubation conditions and should be the first choice in rapid sequence intubation for the normal patient.23 While the proposal of Stept and Safar included a standard 100mg dose for an average 70kg individual, later studies established that the dose should be 1mg/kg.
Up to this point, we have explained in detail why succinylcholine is the muscle relaxant of choice for rapid sequence intubation in the standard patient. However, ICU patients are not candidates for receiving succinylcholine, due to the extended periods of immobility these patients endure; already after 6–12hours of immobilization, patients up-regulate the nicotinic acetylcholine receptors, both within and outside the neuromuscular plate and start the expression of the α7AChR isoform.24,25 In view of the depolarization by succinylcholine, the normal receptors and the new isoforms start releasing intracellular potassium26; this is compounded by the fact that isoform α7AChR strongly and persistently depolarizes, not just in response to endogenous succinylcholine and acetylcholine, but also on account of its choline metabolite. Additionally, the absolute rise in the number of receptors leads to an overproduction of potassium.23 Following the administration of 1mg/kg of succinylcholine, the serum potassium elevation in a normal individual usually does not exceed 0.5mmol/l, while in an immobile individual may raise to 3mmol/l.27,28
Leiman showed that in addition to the raise in potassium following a succinylcholine injection, the automaticity of the cardiac cells increases and the threshold for ventricular fibrillation decreases as a result of the rise in catecholamines. Succinylcholine briefly raises the levels of norepinephrine and epinephrine due to its impact on the presynaptic nicotinic receptors of the postganglionic sympathetic nerve endings.29
Then, what is the option to relax patients in the ICU? Rocuronium is a non-depolarizing muscle relaxant with the fastest onset of action. At a 0.8–1.2mg/kg dose it provides excellent intubation conditions in 60seconds.26 Three clinical trials showed that in emergency situations, rocuronium was equivalent to succinylcholine in developing acceptable intubation conditions.30–32 In view of the available evidence and considering the unjustified risks when administering depolarizing muscle relaxants, we walk away from Jaber's protocol to recommend the use of rocuronium over succinylcholine in ICU patients.
Should opioids be used in RSI?Opioids were initially excluded from RSI due to their slow onset of action and extended effect.13 With the introduction of the modern opioids (fentanyl, alfentanyl and remifentanyl), several studies have shown an adequate profile of an almost total attenuation of the cardiovascular response,33–35 and improved intubation conditions. Though Jaber failed to consider the use of opioids in his protocol, in view of the available evidence we suggest the inclusion of one of the fast-acting opioids in the RSI protocols for ICU patients. Whichever the choice, it should be administered before the hypnotic agent. Fentanyl is widely used at a 1-2μg/kg dose because it is more liposoluble than morphine, releases less histamine and provides hemodynamic stability.36
Sellick's maneuverBy applying pressure over the cricoid cartilage against the cervical vertebrae of a corpse, Sellick realized that regurgitation of the gastric contents in the pharynx could be prevented. Then he applied the technique in 26 patients with high risk of aspiration during anesthetic induction, and none of them experienced regurgitation or vomiting. Since then, Sellick's maneuver (SM) is a must when intubating patients at high risk of aspiration. The current recommendation is to apply a pressure of 10 Newton (N) (1kg) in the patient when awake and 30N (3kg)37 in the unconscious patient. There have been however several reports about fatal aspiration and regurgitation, despite the use of the SM.38,39 Other studies report worsening of the intubation conditions.40 Inappropriate timing for administering the SM, excessive strength or compression of the thyroid instead of the cricoid cartilage, would be the reasons for the SM associated issues.10 However, when the maneuver is adequately performed – as shown by Sellick – it contributes to prevent the passage of gastric contents into the airway.
Immediate confirmation of tube placement with capnographyTwo studies showed that capnography has a 100% sensitivity and specificity to confirm the correct placement of the tube in the trachea, in patients with cardiorespiratory arrest.41,42 The American Heart Association (AHA), the European Resuscitation Council and the International Liaison Committee of Resuscitation (ILCOR) recommend that, in addition to auscultation and to the direct visual examination, capnography should be used to confirm a successful intubation.43,44
Norepinephrine if the diastolic pressure remains under 35mmHgThe most recent Cochrane review on hypotensive shock45 23 clinical controlled, randomized studies including 3212 patients with hypotensive shock were analyzed. The authors concluded that there is no difference among the six vasopressors (norepinephrine, dopamine, epinephrine, vasopressin, terlipressin, dobutamine) analyzed in terms of mortality and that probably, the choice of vasopressor does not affect the final result. However, in one of the largest studies comparing norepinephrine versus dopamine,46 the subgroup analysis according to the type of shock, showed a beneficial effect on the 28-day mortality in patients with cardiogenic shock treated with norepinephrine; the drawback was that the randomization was not stratified and hence the differences could have been random. Until additional information is made available, it is impossible to determine which is the vasopressor of choice for the management of persistent hypotension.
Protective ventilationWhat is protective ventilation? According to Cochrane,47 protective ventilation is the ventilator strategy using tidal volumes below or equal to 7ml/kg, and plateau pressures below 31mm H2O. Amato et al.,48 among several authors, showed the benefits of using low tidal volumes: patients under protective ventilation die less (38% vs. 71%), mechanical ventilation weaning is easier and faster (66% vs. 29%) and barotrauma is lower (7% vs. 42%). In an independent study, Ranieri showed that protective ventilation decreases the cellular inflammatory response.49 The same Cochrane group found that those patients exhibited a lower mortality at 28 days, as compared to patients ventilated with high tidal volumes (9.4–9.9ml/kg) and plateau pressure above (31–37mm H2O). On the other hand, and contrary to Jaber's recommendations, the ALVEOLI50 trial failed to evidence discrepancies in mortality of the patients in response to PEEP variations, regardless of a high or low PEEP. A major requirement is to preserve a low tidal volume.
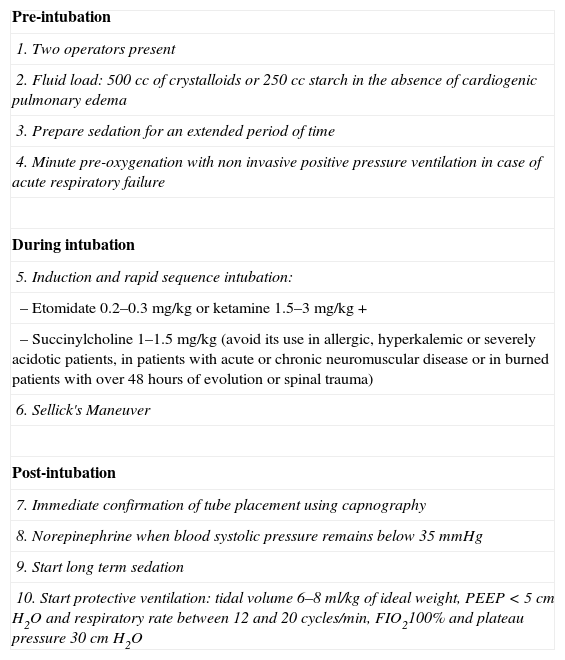
RecommendationBased on the scrutiny of the available medical literature on RSI in the ICU, we would like to suggest a modified sequence (Table 3), convinced that only a rigorous follow-up of our will show the benefit of the technique.
Steps suggested by the authors for rapid sequence intubation in intensive care patients.
| Pre-intubation |
| 1. Two operators available |
| 2. Fluid load: 500cc of crystalloids or 250cc starch if no cardiogenic pulmonary edema is present |
| 3. Prepare the sedation for an extended period of time |
| 4. Pre oxygenation for 3minutes with non-invasive positive pressure ventilation in case of acute respiratory failure |
| During intubation |
| 5. Induction and rapid sequence intubation |
| – Fentanyl 2μ/kg + |
| – Etomidate 0.2–0.3mg/kg (avoid in the septic patient) or ketamine 1.5–3mg/kg + |
| – Rocuronium 1.2mg/kg |
| 6. Sellick's Maneuver |
| Post-intubation |
| 7. Immediate confirmation of tube placement with capnography |
| 8. Dopamine or norepinephrine if the diastolic blood pressure remains below 35mmHg |
| 9. Start long term sedation |
| 10. Start protective ventilation: tidal volume 6–8ml/kg of ideal weight and plateau pressure 30cm H2O |
Source: The authors based on Jaber et al.6 and on literature review.
The adoption of protocols is a strategy that has proven to be of lower mortality in medical practice, for reasons including the fact that our reasoning may get blurred under highly stressing situations. Protocols are a tool to regain control of the situation and provide us with valuable time to analyze the circumstances surrounding the event. This modified Jaber's protocol for rapid sequence induction – intubation in the intensive care unit is intended as a handy therapeutic tool for critical patients; we hope that, just as with the original protocol, the modified algorithm will contribute to reduce the morbidity and mortality in our patients.
Financing sourcesNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Quintero IF, et al. Síndrome de hipotensión endocraneana: ¿una cefalea pospunción dural? Rev Colomb Anestesiol. 2013;41:24–33.