The aim of the study is to compare the emotional effects of COVID-19 among three different groups, namely: health personnel, medical students, and a sample of the general population.
Methods375 participants were recruited for this study, of which 125 were medical students (preclinical studies, 59; clinical studies, 66), 125 were health personnel (COVID-19 frontline personnel, 59; personnel not related with COVID-19, 66), and 125 belonged to the general population. The PHQ-9, GAD-7, and CPDI scales were used to assess the emotional impact. A multinomial logistic regression was performed to measure differences between groups, considering potential confounding factors.
ResultsRegarding CPDI values, all other groups showed reduced values compared to COVID-19 frontline personnel. However, the general population, preclinical and clinical medical students showed increased PHQ-9 values compared to COVID-19 frontline personnel. Finally, confounding factors, gender and age correlated negatively with higher CPDI and PHQ-9 scores.
ConclusionsBeing frontline personnel is associated with increased COVID-19-related stress. Depression is associated, however, with other groups not directly involved with the treatment of COVID-19 patients. Female gender and younger age correlated with COVID-19-related depression and stress.
El objetivo del estudio es comparar los efectos emocionales de la COVID-19 entre 3 grupos diferentes, a saber: personal de salud, estudiantes de Medicina y una muestra de la población general.
MétodosSe incluyó a 375 participantes en este estudio, de los que 125 eran estudiantes de Medicina (estudios preclínicos, 59; estudios clínicos, 66), 125 eran personal de salud (personal de primera línea contra la COVID-19, 59; personal no relacionado con la COVID-19, 66) y 125 pertenecían a la población general. Las escalas PHQ-9, GAD-7 y CPDI se utilizaron para evaluar el impacto emocional. Se realizó una regresión logística multinomial para medir las diferencias entre grupos, considerando posibles factores de confusión.
ResultadosCon respecto a los valores del CPDI, todos los demás grupos mostraron valores reducidos en comparación con el personal de primera línea contra la COVID-19. Sin embargo, la población general y los estudiantes de Medicina preclínica y clínica mostraron un aumento de los valores del PHQ-9 en comparación con el personal en primera línea. Por último, los factores de confusión, sexo y edad se correlacionaron negativamente con puntuaciones más altas del CPDI y el PHQ-9.
ConclusionesSer personal de primera línea se asocia con más estrés relacionado con la COVID-19. Sin embargo, la depresión está asociada con otros grupos que no están directamente involucrados en el tratamiento de los pacientes con COVID-19. Las mujeres y los participantes más jóvenes se correlacionaron con la depresión y el estrés relacionados con la COVID-19.
Since the first case reports, the coronavirus disease of 2019 (COVID-19) has spread rapidly and has caused diverse negative changes in the world population. These involved not only social restrictions, but also negative consequences for the mental health of society. Different groups, who work actively with COVID-191 as well as those who have to comply with the COVID-19 lockdown rules,2 are exposed to higher stress, anxiety, and depression rates. For instance, two cross-sectional studies revealed that during the COVID-19 pandemic, college students reported high levels of mental health distress and academic difficulties,3,4 causing a significant negative impact on their mental health.3,4 Another study in Pakistan, which involved active COVID-19 frontline health personnel, found higher prevalence rates with moderate-to-severe anxiety and depression scores.5 Similar results have been found in the study of AlAteeq et al. This study revealed that depression and anxiety symptoms are prevalent among COVID-19 health personnel.6 Depression and anxiety are not only prevalent in health personnel, but also in medical students, who are health personnel in training. In this case, a study with medical students reported that almost two-thirds of the medical students showed moderate-to-severe symptoms of depression.7 Furthermore, the same study found that half of these students showed higher anxiety symptoms. In this case, and similar to the health personnel, medical students are affected severely by mental health issues related to the COVID-19 pandemic-7-9 These negative consequences of the COVID-19 pandemic have also affected the general population not related directly to COVID-19. A Peruvian study showed that almost half of the participants showed mild to severe scores related to COVID-19 related stress.10 Other non-healthcare workers have reported that processing COVID-19 information is correlated positively with distress levels.11 Another example with the general population not related to health professions is the study of Zhang et al. Higher levels of depression were found among the general population during the COVID-19 pandemic, mostly related to stress and hopeless feelings.12
Pandemics (e.g., COVID-19) are mostly related to higher rates of depression,13–15 anxiety16,17 and stress18,19 reported in general population, health personnel and medical students. Despite the numerous reports, few studies compare the aforementioned groups. The information obtained regarding this matter will establish better intervention policies to prioritize the most affected population groups, offering medical intervention, social and therapeutic support. To this end, the main objective of this study is to find out differences between medical students, COVID-19 frontline health personnel, health personnel not exposed to COVID-19, and the general population, regarding depression, anxiety, and distress scores.
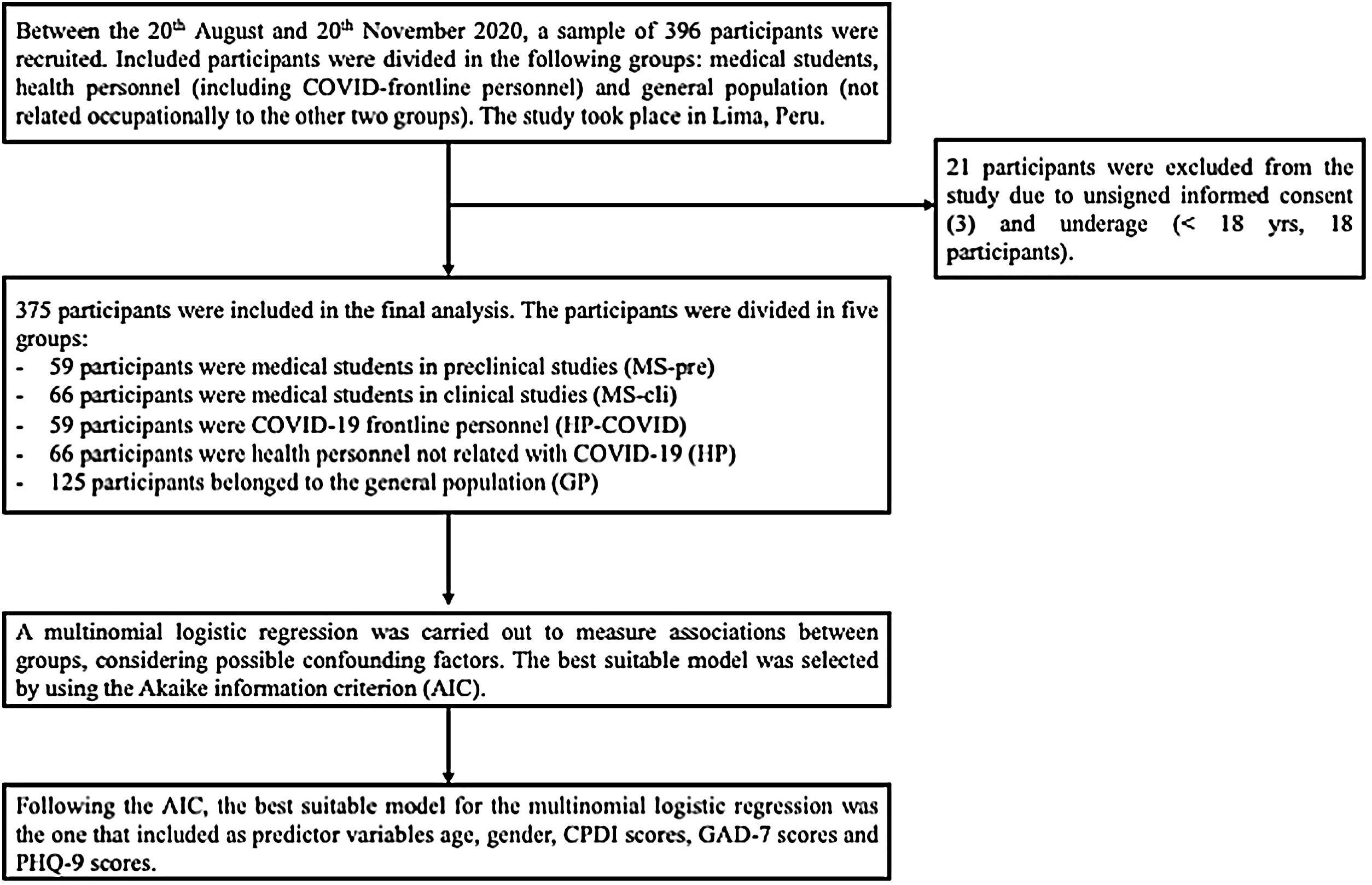
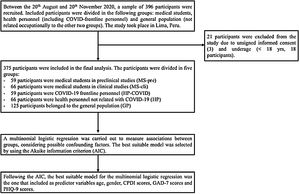
Material and methodsStudy design and selection criteriaFor this study, 375 participants between 18 and 80 years old were recruited voluntarily from Lima (Peru) for an online survey. The volunteers included medical students from the faculty of Medicine of Cayetano Heredia University (UPCH) and health personnel from Lima's health centers. The participants were recruited between 20th August and 20th November 2020 and allocated into 5 groups: general population (GP; n=125), medical students in preclinical studies (MS-pre; n=59), medical students in clinical studies (MS-cli; n=66), COVID-19 frontline health personnel (HP-COVID; n=59) and health personnel not involved with COVID-19 patients (HP; n=66). A complete description is shown in “Results”. A flowchart of the study is presented in Figure 1.
Participants younger than 18 years old, with insufficient knowledge of Spanish and medical difficulties that could restrict the participation (i.e., learning difficulties, especially illiteracy as well incomplete school studies, or blindness in the online survey were not included in this study.
All participants were fully informed of the study and gave their consent to participate. This study was approved by the ethics committee from the Faculty of Medicine of the Peruvian University Cayetano Heredia and carried out in accordance with the Helsinki Declaration and the ethical standards of the APA.
Data collectionOnline surveyThe information of this study comes from a database of a study project that englobes emotional impact and COVID-19 pandemics. Part of this information was published recently by Krüger-Malpartida et al.,10 and some methodological aspects of this article were followed also in this study.
For the data collection, an online survey was carried out. Due to the restrictive policies for avoiding COVID-19 contagions, all instruments and questions were digitalized and programmed in using a free internet survey program (Google Forms). Afterwards, the online survey was distributed through different social media (i.e., Facebook, Twitter, Instagram, LinkedIn, etc.) and using the principles of the snowballing sampling for the data recollection. In case of the medical students, we distributed also the online survey by using the e-mail program of the university and to different social groups of the UPCH medical faculty. The questions included: informed consent, general information (i.e., age, gender, district, confession/faith, and occupation), previous medical diagnosis and medication intake, and the COVID-19 peritraumatic distress index (CPDI) for the COVID-19 pandemic, GAD-7, and PHQ-9 instruments. Before answering the questions, each participant must accept its participation through the informed consent and declare that the participant is full age (i.e., 18 years old).
Finally, additional questions were asked, as follows: “In the last 14 days, did you have a cough, difficulty breathing, sore throat, and fever?” (COVID_1); “Do you have positive results for any COVID-19 test?” (COVID_2); “Have you been hospitalized (or are you hospitalized at the moment) due to COVID-19?” (COVID_3); “Do you have relatives with positive results for any COVID-19 test?” (COVID_4); “Do you have relatives who were hospitalized due to COVID-19?” (COVID_5), and “Do you have relatives who have passed away due to COVID-19?” (COVID_6).
COVID-19 peritraumatic distress indexThe authors of this study followed the definition of COVID-19 related stress used in a recent study of Krüger-Malpartida et al., published elsewhere10. Some methodological aspects of this article were followed also in this study.
The CPDI was first applied in China20 and recently validated in other countries.20,21 In addition, the Spanish version of this instrument was also validated for its use in Peru.22 This instrument was designed for a populational evaluation of changes related to mood, behavior, cognitive skills, circadian rhythm, and other somatic symptoms due to the COVID-19 pandemic.
This instrument consists of 24 items, with a four-factor design: negative mood, cognition, behavioral change, somatization, and hyperarousal/exhaustion. Each item was evaluated by using Likert elements (from 0 to 4: never, occasionally, sometimes, often, and most of the time).10 The sum of each value per question results in the raw score. The displayed score is obtained by adding 4 to the raw score and used to calculate the CPDI severity degrees. For this reason, this instrument defines different categories for peritraumatic stress due to the COVID-19 pandemic: normal (0 to 28 display points), mild (29 to 52 display points, and severe (53 to 100 display points).10
Depressive and anxiety symptomsThe authors of this study followed the definition of depression and anxiety used in a recent study of Krüger-Malpartida et al., published elsewhere.10 Some methodological aspects of this article were followed also in this study.
The Peruvian version of the PHQ-923 was used to assess the severity of depressive symptoms. The PHQ-9 delivers values in the range between 0 and 27. The highest value indicates a higher depression score. This instrument was validated in Peru with a representative sample (n=30 446) and showed significant internal consistency (Cronbach's α=.87). This inventory defines different categories for depression scores: minimal (1 to 4 points), mild (5 to 9 points), moderate (10 to 14 points), and severe (15 to 27 points).23
For anxiety symptoms, the Peruvian version of the GAD-724 was used to assess the severity of anxiety symptoms. The GAD-7 delivers values in the range between 0 and 21 points. The highest value indicates a higher anxiety score. This instrument was also validated in Peru with a representative sample (n=2978), showing significant internal consistency (Cronbach's α=.89). This inventory also defines different categories for anxiety scores: minimal (0 to 4 points), mild (5 to 10 points), moderate (11 to 15 points, and severe (16 to 21 points).24
Statistical analysisStatistical analyses were performed using SPSS version 26.0 (Statistical Package for the Social Sciences, IBM Corp., United States of America) and jamovi 1.2.5.025.
Descriptive data were managed with count data and percentages. To improve readability, the information is presented in tables. Quantitative variables approximately fitting a normal distribution are specified in the text as the mean±standard deviation, and those with a non-normal distribution are expressed as the median (Me) [interquartile range]. Categorical variables were specified with count data and percentages. Data were rounded to 2 decimals. Values smaller than 0.001 were shown as <.001 and values greater than one million were expressed in scientific notation.
Multinomial logistic regression was computed for comparing the 5 groups, considering the group status (GP, MS-pre, MS-cli, HP or HP-COVID) as a dependent variable. Regarding predictor variables, the following were used as predictor variables and added in 4 different blocks, as follows:
Block 1: CPDI scores, GAD-7 scores, PHQ-9 scores.
Block 2: age, gender, CPDI scores, GAD-7 scores, PHQ-9 scores.
Block 3: COVID_1, COVID_2, COVID_3, COVID_4, COVID_5, COVID_6, age, gender, CPDI scores, GAD-7 scores, PHQ-9 scores.
Block 4: residence, religion/faith, medication intake, previous medical disease, COVID_1, COVID_2, COVID_3, COVID_4, COVID_5, COVID_6, age, gender, CPDI scores, GAD-7 scores, PHQ-9 scores.
The “block” that best explained the data was chosen by using the Akaike information criterion (AIC).
The results of this statistical modeling are presented in “Results”. The odds ratio (OR) was flagged as “significant” if the 2-tailed P-value was <.05. The 95% confidence intervals (95%CI) were calculated for this model.
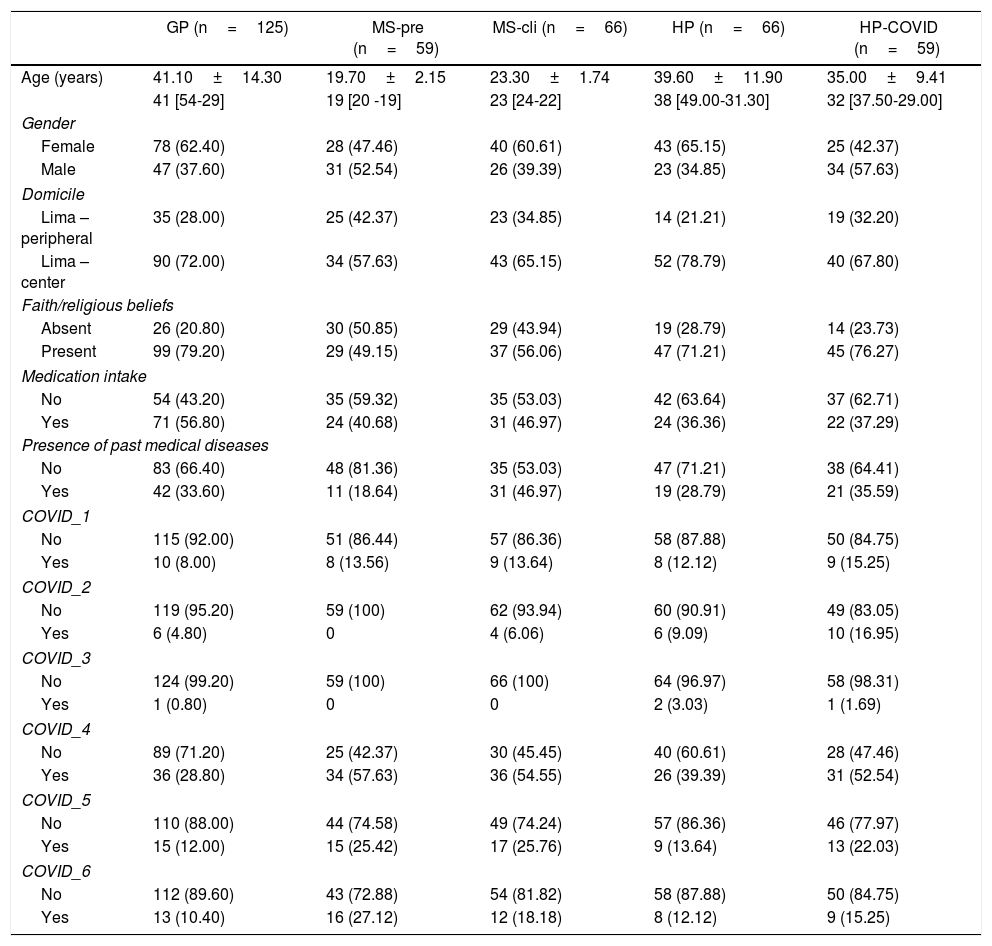
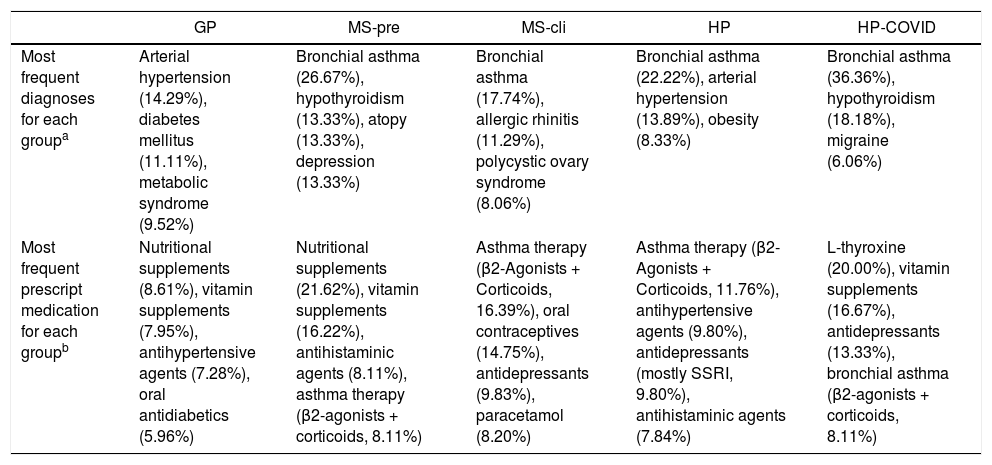
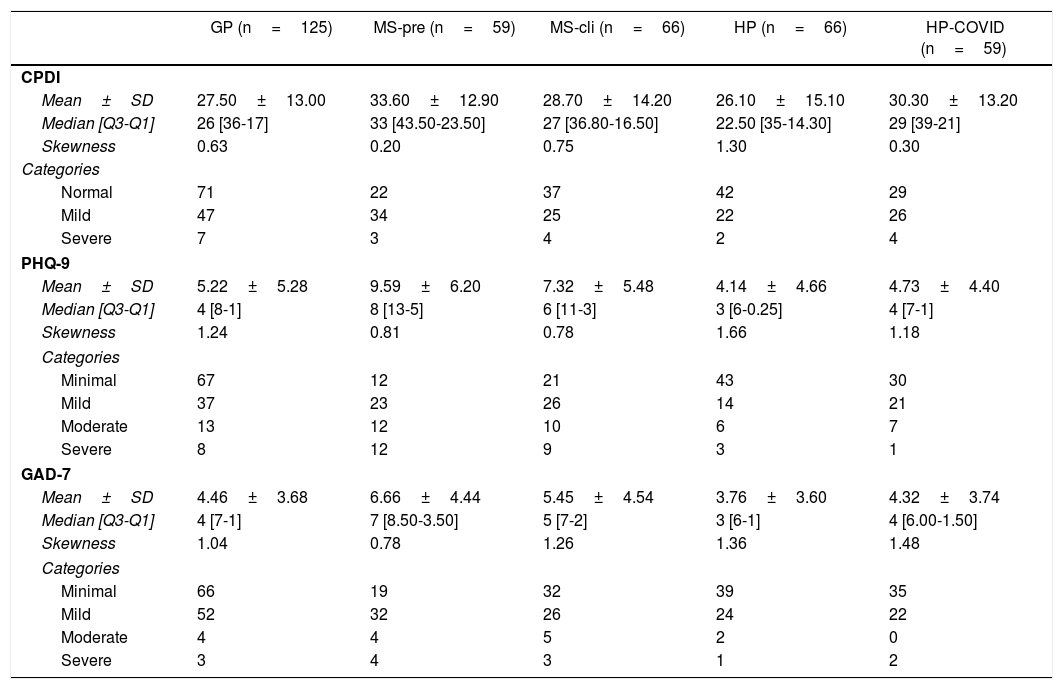
ResultsGeneral sample descriptions, including medication intake and previous clinical diagnoses of the 5 groups included in the study, are listed in Table 1. Previous information regarding COVID-19 infection, including COVID-19 infection of relatives, is represented in Table 1. Information regarding the most frequent previous clinical diagnosis and the most frequent prescribed medication is represented in Table 2. Descriptive data regarding anxiety scores, depression scores, and CPDI scores are presented in Table 3.
General socio-demographic data and COVID-19 contact information.
| GP (n=125) | MS-pre (n=59) | MS-cli (n=66) | HP (n=66) | HP-COVID (n=59) | |
|---|---|---|---|---|---|
| Age (years) | 41.10±14.30 | 19.70±2.15 | 23.30±1.74 | 39.60±11.90 | 35.00±9.41 |
| 41 [54-29] | 19 [20 -19] | 23 [24-22] | 38 [49.00-31.30] | 32 [37.50-29.00] | |
| Gender | |||||
| Female | 78 (62.40) | 28 (47.46) | 40 (60.61) | 43 (65.15) | 25 (42.37) |
| Male | 47 (37.60) | 31 (52.54) | 26 (39.39) | 23 (34.85) | 34 (57.63) |
| Domicile | |||||
| Lima – peripheral | 35 (28.00) | 25 (42.37) | 23 (34.85) | 14 (21.21) | 19 (32.20) |
| Lima – center | 90 (72.00) | 34 (57.63) | 43 (65.15) | 52 (78.79) | 40 (67.80) |
| Faith/religious beliefs | |||||
| Absent | 26 (20.80) | 30 (50.85) | 29 (43.94) | 19 (28.79) | 14 (23.73) |
| Present | 99 (79.20) | 29 (49.15) | 37 (56.06) | 47 (71.21) | 45 (76.27) |
| Medication intake | |||||
| No | 54 (43.20) | 35 (59.32) | 35 (53.03) | 42 (63.64) | 37 (62.71) |
| Yes | 71 (56.80) | 24 (40.68) | 31 (46.97) | 24 (36.36) | 22 (37.29) |
| Presence of past medical diseases | |||||
| No | 83 (66.40) | 48 (81.36) | 35 (53.03) | 47 (71.21) | 38 (64.41) |
| Yes | 42 (33.60) | 11 (18.64) | 31 (46.97) | 19 (28.79) | 21 (35.59) |
| COVID_1 | |||||
| No | 115 (92.00) | 51 (86.44) | 57 (86.36) | 58 (87.88) | 50 (84.75) |
| Yes | 10 (8.00) | 8 (13.56) | 9 (13.64) | 8 (12.12) | 9 (15.25) |
| COVID_2 | |||||
| No | 119 (95.20) | 59 (100) | 62 (93.94) | 60 (90.91) | 49 (83.05) |
| Yes | 6 (4.80) | 0 | 4 (6.06) | 6 (9.09) | 10 (16.95) |
| COVID_3 | |||||
| No | 124 (99.20) | 59 (100) | 66 (100) | 64 (96.97) | 58 (98.31) |
| Yes | 1 (0.80) | 0 | 0 | 2 (3.03) | 1 (1.69) |
| COVID_4 | |||||
| No | 89 (71.20) | 25 (42.37) | 30 (45.45) | 40 (60.61) | 28 (47.46) |
| Yes | 36 (28.80) | 34 (57.63) | 36 (54.55) | 26 (39.39) | 31 (52.54) |
| COVID_5 | |||||
| No | 110 (88.00) | 44 (74.58) | 49 (74.24) | 57 (86.36) | 46 (77.97) |
| Yes | 15 (12.00) | 15 (25.42) | 17 (25.76) | 9 (13.64) | 13 (22.03) |
| COVID_6 | |||||
| No | 112 (89.60) | 43 (72.88) | 54 (81.82) | 58 (87.88) | 50 (84.75) |
| Yes | 13 (10.40) | 16 (27.12) | 12 (18.18) | 8 (12.12) | 9 (15.25) |
GP: general population; HP: health personnel (not COVID-19 frontline health personnel); HP-COVID: COVID-19 frontline health personnel; MS-cli: medical students, clinical studies; MS-pre: medical students, pre-clinical studies.
COVID_1: in the last 14 days, did you have cough, difficulty breathing, sore throat and fever?; COVID_2: do you have positive results for any sort of COVID-19 test?; COVID_3: have you been hospitalized (or are you hospitalized at the moment) due to COVID-19?; COVID_4: do you have relatives with positive results for any sort of COVID-19 test?; COVID_5: do you have relatives who were hospitalized due to COVID-19?; COVID_6: do you have relatives who have passed away?
Data shown as n (%), mean±standard deviation, or median [interquartile range].
Most frequent diagnoses and prescript medication for each group.
| GP | MS-pre | MS-cli | HP | HP-COVID | |
|---|---|---|---|---|---|
| Most frequent diagnoses for each groupa | Arterial hypertension (14.29%), diabetes mellitus (11.11%), metabolic syndrome (9.52%) | Bronchial asthma (26.67%), hypothyroidism (13.33%), atopy (13.33%), depression (13.33%) | Bronchial asthma (17.74%), allergic rhinitis (11.29%), polycystic ovary syndrome (8.06%) | Bronchial asthma (22.22%), arterial hypertension (13.89%), obesity (8.33%) | Bronchial asthma (36.36%), hypothyroidism (18.18%), migraine (6.06%) |
| Most frequent prescript medication for each groupb | Nutritional supplements (8.61%), vitamin supplements (7.95%), antihypertensive agents (7.28%), oral antidiabetics (5.96%) | Nutritional supplements (21.62%), vitamin supplements (16.22%), antihistaminic agents (8.11%), asthma therapy (β2-agonists + corticoids, 8.11%) | Asthma therapy (β2-Agonists + Corticoids, 16.39%), oral contraceptives (14.75%), antidepressants (9.83%), paracetamol (8.20%) | Asthma therapy (β2-Agonists + Corticoids, 11.76%), antihypertensive agents (9.80%), antidepressants (mostly SSRI, 9.80%), antihistaminic agents (7.84%) | L-thyroxine (20.00%), vitamin supplements (16.67%), antidepressants (13.33%), bronchial asthma (β2-agonists + corticoids, 8.11%) |
GP: general population; HP: health personnel (not COVID-19 frontline health personnel); HP-COVID: COVID-19 frontline health personnel; MS-cli: medical students, clinical studies; MS-pre: medical students, pre-clinical studies.
CPDI, PHQ-9 and GAD-7 descriptive data.
| GP (n=125) | MS-pre (n=59) | MS-cli (n=66) | HP (n=66) | HP-COVID (n=59) | |
|---|---|---|---|---|---|
| CPDI | |||||
| Mean±SD | 27.50±13.00 | 33.60±12.90 | 28.70±14.20 | 26.10±15.10 | 30.30±13.20 |
| Median [Q3-Q1] | 26 [36-17] | 33 [43.50-23.50] | 27 [36.80-16.50] | 22.50 [35-14.30] | 29 [39-21] |
| Skewness | 0.63 | 0.20 | 0.75 | 1.30 | 0.30 |
| Categories | |||||
| Normal | 71 | 22 | 37 | 42 | 29 |
| Mild | 47 | 34 | 25 | 22 | 26 |
| Severe | 7 | 3 | 4 | 2 | 4 |
| PHQ-9 | |||||
| Mean±SD | 5.22±5.28 | 9.59±6.20 | 7.32±5.48 | 4.14±4.66 | 4.73±4.40 |
| Median [Q3-Q1] | 4 [8-1] | 8 [13-5] | 6 [11-3] | 3 [6-0.25] | 4 [7-1] |
| Skewness | 1.24 | 0.81 | 0.78 | 1.66 | 1.18 |
| Categories | |||||
| Minimal | 67 | 12 | 21 | 43 | 30 |
| Mild | 37 | 23 | 26 | 14 | 21 |
| Moderate | 13 | 12 | 10 | 6 | 7 |
| Severe | 8 | 12 | 9 | 3 | 1 |
| GAD-7 | |||||
| Mean±SD | 4.46±3.68 | 6.66±4.44 | 5.45±4.54 | 3.76±3.60 | 4.32±3.74 |
| Median [Q3-Q1] | 4 [7-1] | 7 [8.50-3.50] | 5 [7-2] | 3 [6-1] | 4 [6.00-1.50] |
| Skewness | 1.04 | 0.78 | 1.26 | 1.36 | 1.48 |
| Categories | |||||
| Minimal | 66 | 19 | 32 | 39 | 35 |
| Mild | 52 | 32 | 26 | 24 | 22 |
| Moderate | 4 | 4 | 5 | 2 | 0 |
| Severe | 3 | 4 | 3 | 1 | 2 |
CPDI: COVID-19 peritraumatic distress index; GAD-7: general anxiety disorder questionnaire 7; GP: general population; HP: health personnel (not COVID-19 frontline health personnel); HP-COVID: COVID-19 frontline health personnel; MS-cli: medical students, clinical studies; MS-pre: medical students, pre-clinical studies; PHQ-9: patient health questionnaire 9; Q1: 25th percentile; Q3: 75th percentile; SD: standard deviation.
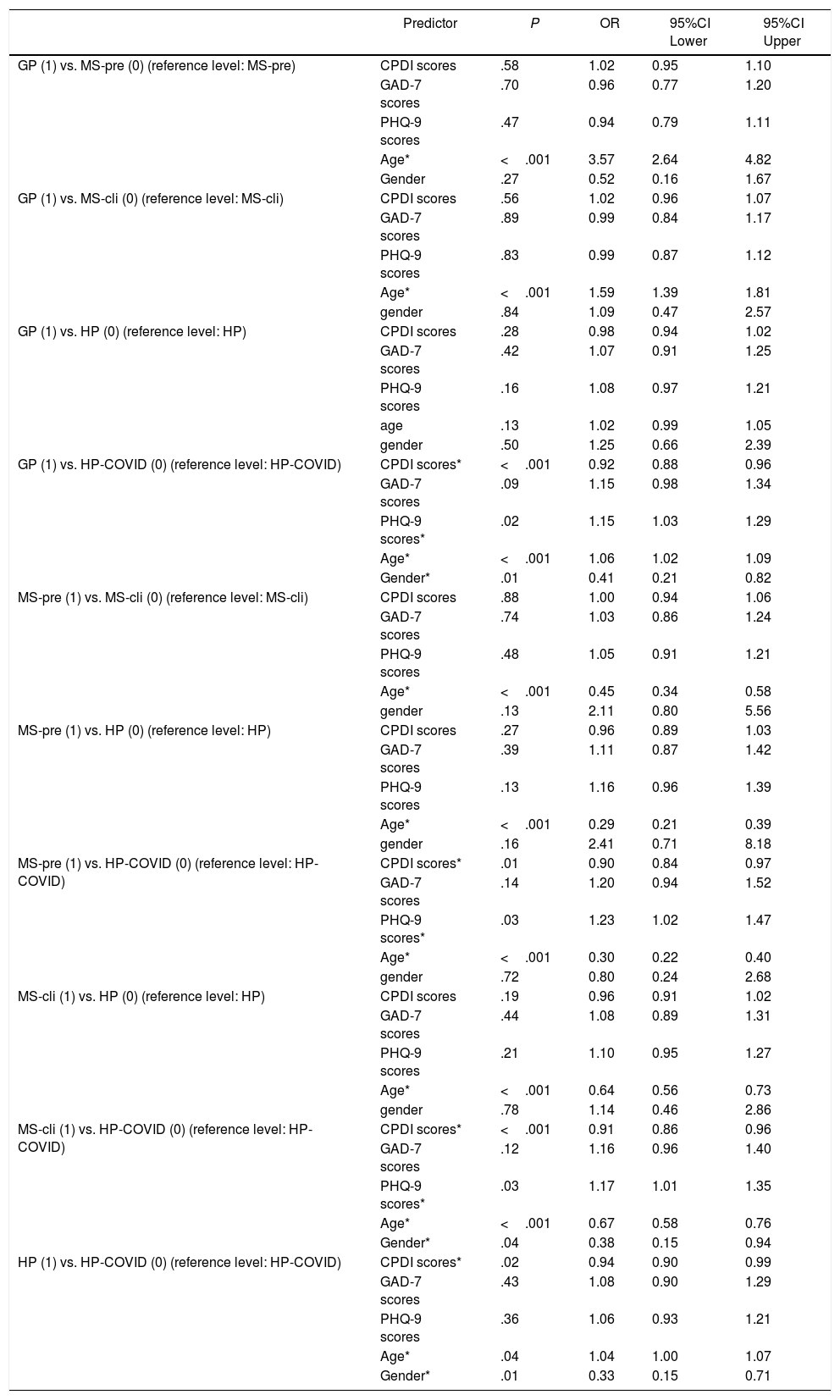
This study's objective was to find out differences between the 5 established groups (i.e., GP, MS-pre, MS-cli, HP and HP-COVID) regarding depression, anxiety, and distress scores. Variables were introduced stepwise in 4 different blocks. The block which best explained the data was chosen using a smaller AIC. In this case, Block 2 was chosen as the model that could best explain the data of the 5 groups (Block 1, χ2(df=12)=63.10, AIC=1139; Block 2, χ2(df=20)=408.40, AIC=809; Block 3, χ2(df=44)=442.40, AIC=823; Block 4, χ2(df=56)=462.10, AIC=828). Block 2 included the variables age, gender, CPDI scores, GAD-7 scores, PHQ-9 scores as predictors.
Different correlations were found between the 5 groups. These are presented in Table 4. In summary, being part of the GP correlated positively with higher PHQ-9 values, when compared to the HP-COVID group (GP vs. HP-COVID, OR=1.15; 95%CI, 1.03-1.29; P=.02). Similar positive correlations were observed in the MS-pre (MS-pre vs. HP-COVID, OR=1.23; 95%CI, 1.02-1.47; P=.03). Moreover, being part of the MS-cli group correlated with higher PHQ-9 values, when compared to HP-COVID (MS-cli vs. HP-COVID, OR=1.17; 95%CI, 1.01-1.35; P=.03). Within those comparisons, significant correlations were found between PHQ-9 scores, gender and age (Table 4).
Multinomial logistic regression.
| Predictor | P | OR | 95%CI Lower | 95%CI Upper | |
|---|---|---|---|---|---|
| GP (1) vs. MS-pre (0) (reference level: MS-pre) | CPDI scores | .58 | 1.02 | 0.95 | 1.10 |
| GAD-7 scores | .70 | 0.96 | 0.77 | 1.20 | |
| PHQ-9 scores | .47 | 0.94 | 0.79 | 1.11 | |
| Age* | <.001 | 3.57 | 2.64 | 4.82 | |
| Gender | .27 | 0.52 | 0.16 | 1.67 | |
| GP (1) vs. MS-cli (0) (reference level: MS-cli) | CPDI scores | .56 | 1.02 | 0.96 | 1.07 |
| GAD-7 scores | .89 | 0.99 | 0.84 | 1.17 | |
| PHQ-9 scores | .83 | 0.99 | 0.87 | 1.12 | |
| Age* | <.001 | 1.59 | 1.39 | 1.81 | |
| gender | .84 | 1.09 | 0.47 | 2.57 | |
| GP (1) vs. HP (0) (reference level: HP) | CPDI scores | .28 | 0.98 | 0.94 | 1.02 |
| GAD-7 scores | .42 | 1.07 | 0.91 | 1.25 | |
| PHQ-9 scores | .16 | 1.08 | 0.97 | 1.21 | |
| age | .13 | 1.02 | 0.99 | 1.05 | |
| gender | .50 | 1.25 | 0.66 | 2.39 | |
| GP (1) vs. HP-COVID (0) (reference level: HP-COVID) | CPDI scores* | <.001 | 0.92 | 0.88 | 0.96 |
| GAD-7 scores | .09 | 1.15 | 0.98 | 1.34 | |
| PHQ-9 scores* | .02 | 1.15 | 1.03 | 1.29 | |
| Age* | <.001 | 1.06 | 1.02 | 1.09 | |
| Gender* | .01 | 0.41 | 0.21 | 0.82 | |
| MS-pre (1) vs. MS-cli (0) (reference level: MS-cli) | CPDI scores | .88 | 1.00 | 0.94 | 1.06 |
| GAD-7 scores | .74 | 1.03 | 0.86 | 1.24 | |
| PHQ-9 scores | .48 | 1.05 | 0.91 | 1.21 | |
| Age* | <.001 | 0.45 | 0.34 | 0.58 | |
| gender | .13 | 2.11 | 0.80 | 5.56 | |
| MS-pre (1) vs. HP (0) (reference level: HP) | CPDI scores | .27 | 0.96 | 0.89 | 1.03 |
| GAD-7 scores | .39 | 1.11 | 0.87 | 1.42 | |
| PHQ-9 scores | .13 | 1.16 | 0.96 | 1.39 | |
| Age* | <.001 | 0.29 | 0.21 | 0.39 | |
| gender | .16 | 2.41 | 0.71 | 8.18 | |
| MS-pre (1) vs. HP-COVID (0) (reference level: HP-COVID) | CPDI scores* | .01 | 0.90 | 0.84 | 0.97 |
| GAD-7 scores | .14 | 1.20 | 0.94 | 1.52 | |
| PHQ-9 scores* | .03 | 1.23 | 1.02 | 1.47 | |
| Age* | <.001 | 0.30 | 0.22 | 0.40 | |
| gender | .72 | 0.80 | 0.24 | 2.68 | |
| MS-cli (1) vs. HP (0) (reference level: HP) | CPDI scores | .19 | 0.96 | 0.91 | 1.02 |
| GAD-7 scores | .44 | 1.08 | 0.89 | 1.31 | |
| PHQ-9 scores | .21 | 1.10 | 0.95 | 1.27 | |
| Age* | <.001 | 0.64 | 0.56 | 0.73 | |
| gender | .78 | 1.14 | 0.46 | 2.86 | |
| MS-cli (1) vs. HP-COVID (0) (reference level: HP-COVID) | CPDI scores* | <.001 | 0.91 | 0.86 | 0.96 |
| GAD-7 scores | .12 | 1.16 | 0.96 | 1.40 | |
| PHQ-9 scores* | .03 | 1.17 | 1.01 | 1.35 | |
| Age* | <.001 | 0.67 | 0.58 | 0.76 | |
| Gender* | .04 | 0.38 | 0.15 | 0.94 | |
| HP (1) vs. HP-COVID (0) (reference level: HP-COVID) | CPDI scores* | .02 | 0.94 | 0.90 | 0.99 |
| GAD-7 scores | .43 | 1.08 | 0.90 | 1.29 | |
| PHQ-9 scores | .36 | 1.06 | 0.93 | 1.21 | |
| Age* | .04 | 1.04 | 1.00 | 1.07 | |
| Gender* | .01 | 0.33 | 0.15 | 0.71 |
CPDI: COVID-19 peritraumatic distress index; GAD-7: general anxiety disorder questionnaire 7; GP: general population; HP: health personnel (not COVID-19 frontline health personnel); HP-COVID: COVID-19 frontline health personnel; MS-cli: medical students, clinical studies; MS-pre: medical students, pre-clinical studies; PHQ-9: patient health questionnaire 9.
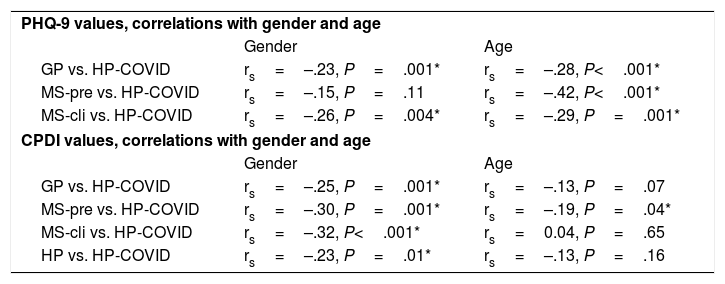
On the other hand, higher CPDI values correlated negatively in the comparison GP vs. HP-COVID (OR=0.92; 95%CI, 0.88-0.96; P<.001). Similar negative correlations were found also between MS-pre vs. HP-COVID (OR=0.90; 95%CI, 0.84-0.97; P=0.01), MS-cli vs. HP-COVID (OR=0.91; 95%CI, 0.86-0.96; P<.001), and HP vs. HP-COVID (OR=0.94; 95%CI, 0.90-0.99; P=.02). Within those comparisons, significant correlations were found between CPDI scores, gender and age (Table 5).
PHQ-9 and CPDI values, and their correlations with gender and age.
| PHQ-9 values, correlations with gender and age | ||
| Gender | Age | |
| GP vs. HP-COVID | rs=–.23, P=.001* | rs=–.28, P<.001* |
| MS-pre vs. HP-COVID | rs=–.15, P=.11 | rs=–.42, P<.001* |
| MS-cli vs. HP-COVID | rs=–.26, P=.004* | rs=–.29, P=.001* |
| CPDI values, correlations with gender and age | ||
| Gender | Age | |
| GP vs. HP-COVID | rs=–.25, P=.001* | rs=–.13, P=.07 |
| MS-pre vs. HP-COVID | rs=–.30, P=.001* | rs=–.19, P=.04* |
| MS-cli vs. HP-COVID | rs=–.32, P<.001* | rs=0.04, P=.65 |
| HP vs. HP-COVID | rs=–.23, P=.01* | rs=–.13, P=.16 |
CPDI: COVID-19 peritraumatic distress index; GAD-7: general anxiety disorder questionnaire 7; GP: general population; HP: health personnel (not COVID-19 frontline health personnel); HP-COVID: COVID-19 frontline health personnel; MS-cli: medical students, clinical studies; MS-pre: medical students, pre-clinical studies; PHQ-9: patient health questionnaire 9.
This study results in 2 different outcomes concerning differences on the emotional impact due to the COVID-19 pandemic between the five groups (i.e., GP, MS-pre, MS-cli, HP, and HP-COVID). On the one hand, this study showed that higher CPDI values correlate with the COVID-19 frontline health personnel compared with the other remaining four groups. On the other hand, the groups GP, MS-pre and MS-cli showed greater PHQ-9 values than COVID-19 frontline health personnel. No correlations were found with the GAD-7 between groups.
Our findings reveal 2 important points. First of all, higher psychological distress reflected in higher CPDI values. Secondly, higher depression values and reduced functionality reflected in higher PHQ-9 values. Moreover, our results revealed that higher psychological distress is mostly related to the COVID-19 frontline health personnel group. The current pandemic resulted for many health personnel overwhelming, mostly because of the different factors that daily they have to confront (i.e., long shifts, increased working hours, altered circadian rhythm, fears, death of patients and colleagues, constant increase of hospitalized patients, etc.). Most people tend to restrict or repress during a constant stress situation emotions and feelings in order to achieve tasks,26 that in this case involve the life of high-risk patients. This could be why the group of the COVID-19 frontline health personnel correlated higher psychological distress values. Finally, our results revealed that higher depression scores correlated with other groups not directly involved with COVID-19. Following the stress-vulnerability model,27 it is possible that some individuals could develop mental health issues due to an stressful event, such as the COVID-19 pandemics and its consequences on the society. The long-lasting isolation, the restriction of free movement and the limitation of different activities (e.g., studying, working, interacting with other people, etc.) could influence, in those vulnerable individuals, the occurrence of depressive symptoms through different biological factors.
To the best of our knowledge, there is information on this line of evidence that could be comparable to our results. For instance, Naser et al. published a cross-sectional study comparing the adverse effects of the COVID-19 pandemic in three different groups: university students, health care professionals, and the general population. They found that mental health problems (i.e., anxiety and depression) were more prevalent in university students.28
In this study, the groups of medical students showed correlations with PHQ-9 values compared to the HP-COVID group. However, no correlations were seen for anxiety scores (Table 4). These outcomes revealing higher depression values among medical students could be due to the social restrictions that obligate many medical students to abandon their studies.7,9,29 The switch to distance education and the suspension of clinical activities or night shifts could have negatively influenced this group's mental health, leading mostly to adverse mood effects.7,9,29
Krishnamoorthy et al. published a meta-analysis indicating that during pandemic, health professionals have a higher prevalence of psychological morbidities than the general population, characterized mostly by psychological distress and poor sleep quality.30 The results of this study indeed support that higher values of psychological distress are correlated to the COVID-19 frontline health personnel group. However, being part of the general population is mostly correlated with higher depression scores. Frontline professionals are faced most of the time with fears of getting infected or infecting others.30 Other concerns, like personal protection, death of their own colleagues, or excess working hours, could have influenced the obtained results.
On the other hand, the general population is exposed to isolation due to the sanitary restrictions.10,29,31 People belonging to the general population are confined in their homes and have their transit restricted.10,29,31 This could lead to higher values of depression, poor sleep quality, hopeless feelings, and suicidal thoughts.32,33
Also remarkable are the results between HP and HP-COVID (Table 4). In this case, being a COVID-19 frontline health professional is correlated with higher values of psychological distress due to COVID-19 (CPDI). Our results could be comparable with the findings of Cai et al.34 In this mentioned study, COVID-19 frontline medical workers have higher rates of mental health problems of any kind compared to non-frontline medical workers.34 Moreover, Cai et al. found correlations between anxiety symptoms, insomnia and depressive mood and being a frontline health professional.34
Finally, the variables age and gender are essential to mention. Significant correlations with the variables age and gender were found in the comparisons (Table 4 and Table 5). This could mean that age and gender could also have influenced in the correlations found by this multinomial logistic regression. In this case, younger age or female gender correlated with higher scores of the aforementioned psychological instruments (i.e., PHQ-9 and CPDI). These obtained results coincided with other studies that have found associations with female gender and age of the participant.21,28,35,36
Although these results contribute to the actual COVID-19 pandemic's panorama, concerning mostly adverse effects on mental health as an emotional impact, the reader must consider some limitations. Firstly, the sampling procedure (in this case the snowballing method) could contravene the principle of randomization. However, the social restrictions due to COVID-19 pandemic made it difficult to have direct contact with other persons, making the online distribution of the survey one of the most suitable methods for recruiting participants and recollecting data. Moreover, the sample size could be larger to generalize the results beyond the study's scope. However, the power obtained from this study with 375 participants and 5 groups was 1–β=.93, a value that overcame the 1–β=.80 threshold. Therefore, the sample size for the study design should be sufficient to examine the expected effects. Also, the higher total of women compared to men could have influenced the results. However, studies related to COVID-19 lockdown distress have also reported a higher proportion of female participants, which is also reflected in this study. As expected, there were many very low CPDI, PHQ-9 and GAD-7 scores in the evaluated participants, which led to skewed distributions. Multinomial logistic regression was computed to overcome this limitation because there is no consideration regarding skewed statistical distributions. Finally, medication intake, previous medical conditions, and district of residence could affect COVID-19 distress scores. All these variables were included in the model. However, these variables did not appear to affect the results of the current study.
In conclusion, being a COVID-19 frontline health personnel is associated with more psychological distress, involving harmful behavioral and emotional components. This could be related to the fact that frontline health professionals confront excess working hours, their colleagues’ death, fear of being infected, among others. On the other hand, higher depression scores were associated mostly with other groups not directly involved with COVID-19 patients’ treatment. This could be related to the sanitary emergency restrictions, the long-lasting isolation, the restriction of free movement, and the limitation of different activities, like studying and accomplishing essential duties (in medical students). Finally, female gender and younger age correlated with depression and stress related to COVID-19, also playing an important role in these findings.
Future studies and public health authorities may consider these obtained results for generating intervention and support. First of all, intervention studies and health policies should consider higher psychological distress in COVID-19 frontline health personnel for creating intervention strategies, such as group or individual psychotherapy. Furthermore, Balint groups and related interventions could also help to comprehend different situations with COVID patients as well to reduce the stress originated from the patient-health personnel relationships. Finally, future studies and public health interventions should consider severe stress cases and their management, especially a combined management with psychotherapy and pharmacotherapy. For the other groups, intervention studies and health policies should consider higher depression values. The intervention and assessment of the other groups (i.e., students, general population and health personnel not related to COVID-19) should be based on telepsychotherapeutic interventions or telepsychiatric consultations. In most severe depression cases, such as extreme agitation or suicide attempts, public health authorities should consider a 24-hour telephone support line for the population.
Author contributionsBruno Pedraz-Petrozzi: First author, wrote the introduction, methods, results, discussion and conclusions. Corrected the manuscript, did the data analysis and the literature search. Hever Krüger-Malpartida: First and corresponding author; PI of this working group, HKM contributed with the introduction, discussion and conclusions, corrected the manuscript and did the literature search. Martin Arévalo-Flores: contributed with the literature search, introduction and discussion, helped with the paper proofreading, corrections and the interpretation of the results in the discussion. Frine Samalvides-Cuba: Corrected the manuscript and helped with the proofreading and paper mentoring. Victor Anculle-Arauco: Helped with the data recollection and contributed with the proofreading. Maurcio Dancuart-Mendoza: Helped with the data recollection and contributed with the proofreading.
Conflict of interestsThe authors declare no conflict of interests.
The authors of this work would like to thank Dr. Natalie Tinney, M.D. (physician and English native speaker) and Dr. Cecilia Clement, M.D. (The University of Texas-Medical Branch, Galveston, Texas) for supporting with the proofreading, spelling and grammar correction of the English language.