Bipolar disorder and schizophrenia are causes of major suffering in patients. Nevertheless, they also affect family and caregiver functioning. This is important because the participation and involvement of families and caregivers is essential to achieve an optimal treatment.
ObjectiveTo describe the level of expressed emotions, burden, and family functioning of bipolar and schizophrenic patients and, to evaluate the efficacy of the multimodal intervention (MI) versus traditional intervention (TI) in family functioning and its perception by patients and caregivers.
Material and methodsA prospective, longitudinal, therapeutic-comparative study was conducted with 302 patients (104 schizophrenic and 198 bipolar patients) who were randomly assigned to a MI or TI groups of a multimodal intervention programme PRISMA. MI group received care from psychiatry, general medicine, neuropsychology, family therapy, and occupational therapy. TI group received care from psychiatry and general medicine. Hamilton, Young and SANS, SAPS scales were applied to bipolar and schizophrenic patients, respectively. The EEAG, FEICS, FACES III and ECF were also applied at the initial and final time.
ResultsThere were statistically significant differences in socio-demographic and clinical variables in schizophrenia vs bipolar group: 83% vs 32.2% were male, 37 vs 43 mean age, 96% vs 59% were single, 50% vs 20% unemployed, and 20% vs 40% had college studies. In addition, 2 vs 2.5 numbers of hospitalisations, 18 vs 16 mean age of substance abuse onset and, 55 vs 80 points in EEAG. There were no statistically significant differences in family scales after conducting a multivariate analysis on thr initial and final time in both groups.
ConclusionsThis study did not show changes in variables of burden and family functioning between bipolar and schizophrenic groups that were under TI vs MI.
El trastorno afectivo bipolar (TAB) y la esquizofrenia son causas importantes de sufrimiento para los pacientes y sus familias, pues se afectan su funcionamiento y su dinámica normal. Esto es importante, ya que la implicación de la familia es esencial para un tratamiento óptimo del paciente.
ObjetivoDescribir el nivel de emociones expresadas, la carga y el funcionamiento de las familias de los pacientes bipolares y esquizofrénicos y evaluar la eficacia de la intervención multimodal (IM) en comparación con la intervención tradicional (IT) en el funcionamiento familiar y en la percepción que de este tienen el paciente y sus cuidadores.
Material y métodosSe realizó un estudio prospectivo, longitudinal, terapéutico-comparativo, con una muestra de 302 pacientes (104 con diagnóstico de esquizofrenia y 198 con TAB) aleatorizados a un grupo de IM y otro de IT dentro de un programa de salud mental con énfasis en reducción de la carga, el daño y el gasto social de la enfermedad mental (PRISMA). Los pacientes asignados a la IM recibían atención por psiquiatría, medicina general, neuropsicología, terapia de familia y terapia ocupacional, y los pacientes asignados a IT recibían atención por psiquiatría y medicina general. Las escalas realizadas al inicio y al final de las intervenciones fueron las de Hamilton y Young, SANS y SAPS, para pacientes bipolares y esquizofrénicos respectivamente. A ambos grupos se aplicaron las escalas EEAG, FEICS, FACES III y ECF.
ResultadosSe encontraron diferencias estadísticamente significativas en las variables sociodemográficas y clínicas entre los grupos de pacientes con TAB y con esquizofrenia. Tras hacer un análisis multivariable MANCOVA, no se observaron diferencias estadísticamente significativas en los resultados entre los momentos inicial y final en los grupos de pacientes con TAB y con esquizofrenia según las escalas FEICS, FACES III y ECF.
ConclusionesEste estudio no evidencia un cambio en la carga y el funcionamiento familiar entre los grupos sometidos a IM y a IT de pacientes bipolares y esquizofrénicos.
Chronic mental disorders such as schizophrenia and bipolar disorder are among the leading causes of disability and morbidity and admission to hospital in the local population. Although they are treatable, and in recent decades advances in psychopharmacology have provided better therapeutic options and greater patient stability, these disorders continue to occupy the top spots in global disability statistics.1
In bipolar disorder the disability is not only associated with affective episodes and residual symptoms; studies show that, even during periods of euthymia, patients have poor cognitive performance in areas such as attention, executive function and memory.2–5 Moreover, it is argued that lifestyle, personality characteristics and ways of coping with mental illness also have an important influence on the demand for care from emergency services, hospital admission and length of stay, and adherence and response to treatment.6 The situation is similar in patients with schizophrenia, many of whom suffer from persistent residual positive and negative symptoms which are directly related to work-related, social and family disability.7,8
The knowledge accumulated up to now on bipolar disorder and schizophrenia tells us that there are alterations in multiple dimensions of the human being, and the complexity of patients requires more comprehensive complementary strategies than those currently available. One answer to this need is to offer patients with bipolar disorder and schizophrenia a multidisciplinary intervention programme in which, in addition to pharmacological treatment, patients have adequate intervention in psychoeducation, psychology, neuropsychological rehabilitation, occupational therapy, family therapy and general medicine, with a treatment plan tailored to individual needs.9–11 Although many of these therapies have been evaluated separately and have proved useful in both disorders, there is little information on the effectiveness of multimodal intervention (MI) programmes compared with traditional intervention (TI) in the different therapeutic targets.
Family dynamics is one of the most important domains in the therapeutic approach and evaluation of patients with chronic mental illness,12 and it is known that there is a bidirectional interaction between patients and their families. The presence of a patient with schizophrenia or bipolar disorder interferes with many aspects of family dynamics, generating a need for support, counselling and psychoeducation on the disease and treatment, as well as indications about how to relate to the patient.13–16 The role of the family is essential, since the lived experience and the proximity with the patient can provide the information necessary to define a work plan and talk about the relationships that exist within the family.17
Studies of patients’ family environments have focused on expressed emotion (EE), that is, individual attitudes or predispositions that facilitate or interfere with interpersonal relationships and constitute a relational process between patients and their relatives.18,19 Important aspects of EE are criticism and emotional over-involvement. Criticism is defined as a negative filter that distorts how people see themselves and others, and over-involvement is the lack of appropriate emotional boundaries between the members of a family. These emotions are highly correlated with the worsening of symptoms and the need for hospitalisation.20–22 The investigation of new strategies with which to address these critical points is necessary in order to help improve patients’ functionality and prognosis.
The mental health programme focusing on reducing the burden, suffering and social spending in mental illness (PRISMA) was designed with several objectives, one of which is the aim to describe the level of expressed emotion (criticism and over-involvement), burden and functioning in a population of patients with bipolar disorder and schizophrenia, and to assess the efficacy of an MI compared with a TI in terms of family functioning and how it is perceived by patients and their carers.
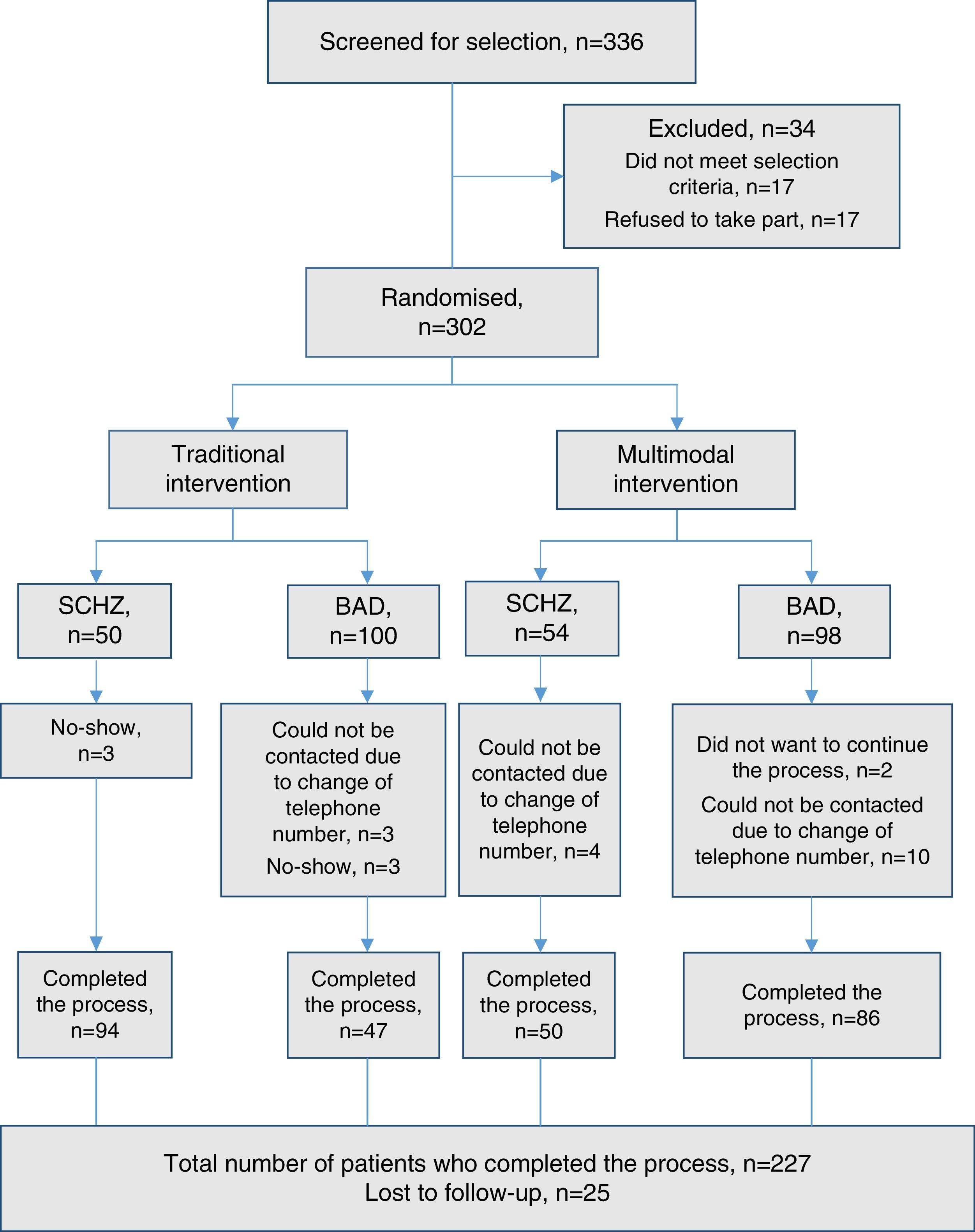
Material and methodsParticipantsA prospective, open-label, longitudinal, therapeutic-comparative clinical trial was conducted with a total sample of 302 patients (104 with schizophrenia and 198 bipolar disorder) who were randomly assigned to the MI or TI groups within a mental health programme focusing on reducing burden, suffering and social spending in mental illness: PRISMA. A professional outside the group with no contact with the patients or the intervention staff performed the randomisation using the Epidat 3.1 programme. After the random assignment, the groups were distributed as follows: MI (50 patients with schizophrenia and 100 with bipolar disorder); and TI (54 patients with schizophrenia and 98 with bipolar disorder).
Patients were selected from the Mood Disorders and Psychosis Clinic at Hospital Universitario San Vicente Fundación or those referred from other institutions by psychiatrists or health workers who knew the programme. Patients had to have been previously diagnosed with bipolar disorder or schizophrenia. The initial assessment of patients began in January 2012; the programme was carried out for approximately 2 years, and the final assessment ended in February 2015.
Patients who met the following inclusion criteria were included: (a) patients diagnosed with bipolar I disorder and schizophrenia according to the Diagnostic Interview for Genetic Studies (DIGS)23; (b) age from 18 to 60 years; (c) having had schooling from the age of 5 to 16 years; (d) having agreed to participate in the study and signed the informed consent form previously explained by the healthcare professional; and (e) be in good health, sufficient to apply the tests.
Among the exclusion criteria were having comorbidities such as other neurological or psychiatric disorders, mental retardation, classic autism or personality disorder. Also excluded were subjects with a history of electroconvulsive therapy in the past 6 months or severe head injury.
The expected primary outcomes were improvement in the level of expressed emotion (criticism and over-involvement), burden and family functioning in patients with bipolar disorder and schizophrenia exposed to two interventions to be compared, traditional vs multimodal.
Informed consent was obtained from all patients after an explanation and resolution of doubts by the healthcare professional. The research project was approved by the respective bioethics committees.
InstrumentsPatients were diagnosed with bipolar I disorder and schizophrenia using the DIGS, translated and validated for Colombia,23 according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (Text Revision) (DSM-IV-TR).24 The 17-item Hamilton Rating Scale for Depression (HRSD)25 and the Young Mania Rating Scale (YMRS),26 both validated in Spanish, were used for patients with bipolar I disorder, and the Scale for the Assessment of Negative Symptoms (SANS) and the Scale for the Assessment of Positive Symptoms (SAPS)27 were applied to subjects with schizophrenia. In addition, both groups of patients were evaluated with the Global Assessment of Functioning (GAF) scale for the past month and at the worst point of the last episode.
For the evaluation of family variables, the following instruments were used:
- 1.
Family Emotional Involvement and Criticism Scale (FEICS). The FEICS consists of two subscales: criticism and involvement; each consists of 7 items and they are intercalated in the scale: the criticism-related items are the even numbers and the involvement-related items are odd numbers. Each item is evaluated according to an ordinal scale (from almost never to almost always, with scores from 1 to 5), so the total for each subscale can be from 7 to 35 points. The version of the FEICS used in this study was translated and validated by the Department of Psychiatry of the University of Antioquia.28
- 2.
Family Adaptability and Cohesion Evaluation Scale (FACES III), a scale for evaluating family functioning. FACES III29 consists of 40 items, each with a Likert-type scale of five options (almost always, very often, sometimes yes and sometimes no, seldom, almost never), divided into two parts: part 1, with 20 items, assesses the level of cohesion and flexibility in the family as the subject perceives it at that moment (“actual family”), and part 2, with 20 items that assess the level of cohesion and flexibility that the subject would like there to be in their family (“ideal family”). This part includes the same items as the first, but the general allocation of points is different. From the differences between the “actual” and “ideal” scales, we can obtain the satisfaction index that the person has with their family functioning.
- 3.
Self-applied Family Burden Scale (FBS). The FBS30 is an adaptation in the form of a self-applied scale from sections of the psychosocial performance scale (Spanish adaptation of the Social Behaviour Assessment Schedule).4 This is a discriminative-type scale. The aspects assessed are objective burden, attribution level and subjective burden. The objective burden section evaluates changes in the daily functioning of the people who form part of the patient's environment. In cases where there is an objective burden (score other than 0), the level of attribution is evaluated, i.e. whether or not informants consider their problems to be related to the patient and to what extent (0=not related; 1=possibly related; 2=clearly related). Lastly, the subjective burden section is an evaluation of the stress that all the items corresponding to the subject's behaviour, their performance of social roles and the adverse effects on others cause in the informant.
At the start of the programme patients were selected and, if they met the inclusion criteria, they were given appointments to attend in groups. The first day the programme was explained to them, and patients who agreed to participate signed the consent form. An identification form was then filled out, in which the patients were assigned a code within the programme and they were referred to healthcare professionals from each specialty to be evaluated using different instruments. The evaluation of family therapy was done individually with patients and mixed (group-individual) with carers.
The evaluation of the patient lasted approximately 30min and consisted of a conversation aimed at collecting information from each patient's genogram and identifying from their perspective the difficulties or objectives of a possible family therapy intervention. The scales to be completed by the patient (FEICS and FACES III) and the carer (FEICS, FACES III and FBS) were then explained. The patients were accompanied by a family therapist or co-therapist during the process to explain any uncertainties about the instrument.
After applying the scales, a conversation lasting approximately 15min was held with each carer to supplement the family information provided by the patient and to obtain the carer's perspective in terms of needs or concerns for a possible family therapy intervention. To avoid fatigue on the day of the evaluation, the day was divided into two blocks, with patients and relatives being offered refreshments and help with travelling expenses.
InterventionMultimodal interventionAn outpatient MI was carried out for patients with bipolar disorder and schizophrenia, which included care from general medicine, psychiatry, psychology, family therapy, neuropsychological rehabilitation, and occupational therapy. Each patient was offered from 12 to 18 intervention sessions, distributed according to a needs assessment performed by the therapeutic group in the initial evaluation. In addition, 10 weekly sessions of psychoeducation were offered for patients with bipolar disorder and relatives with schizophrenia.
The MI programme consisted of periodic interventions by general medicine to assess for other non-mental illnesses and initiate or adjust treatment for comorbidities. In addition, a medical approach focused on promoting healthy lifestyles, in terms of sports, nutrition and hours and quality of sleep, among other areas. There were psychiatric evaluations, the aim of which was to assess and monitor the patient's actual clinical condition, apply clinical scales and adjust pharmacological treatment. The intervention also included occupational therapy appointments for assessing each patient's general, social, family and work functioning, as well as their occupational capacity, in order to establish a therapeutic strategy. Socio-occupational rehabilitation focused on increasing the patient's functional independence, developing integration strategies and preventing disability, in order to encourage social interaction, decrease anxiety and stimulate cognitive function.
Patients were also offered neuropsychological rehabilitation sessions that were complemented by ecological strategies from the Hospital Clínic de Barcelona Research Group's Functional Remediation Programme. Before starting the intervention programme, one of the therapists spent 3 months as a trainee observing and learning about the individual application of this programme. Patients also received individual intervention with cognitive-behavioural psychology and family therapy according to their particular needs identified at the beginning of the programme.
Psychoeducation was provided in group sessions and was designed to offer general knowledge about the disorder, symptoms, recognition of prodromal symptoms, stress management, pharmacological treatment, adverse effects, healthy lifestyles and the rights and duties of the patient, among other topics. The coordinator of the psychoeducation groups was an occupational therapist with experience in group psychotherapy, and the therapists in the programme participated as co-therapists.
Traditional interventionThe TI consisted of assessments by general medicine and psychiatry, a total of 1–2 sessions of each during the follow-up period with the aim of achieving a level of care similar to that currently offered by the health service. No psychoeducational groups were provided in the TI.
Statistical analysisFor the quantitative description of the socio-demographic and clinical variables, measures of central tendency (arithmetic mean), measures of position (median) and measures of dispersion (standard deviation and interquartile range) were used. In the qualitative variables report, absolute frequencies and proportions were used. In the qualitative variables, normality in the distribution was evaluated using the Shapiro–Wilk test, and independence (with respect to groups and subgroups) was measured by the χ2 test and the log-likelihood ratio statistic.
For the comparison of quantitative variables between groups and subgroups, a Student's t test and the Mann–Whitney U test were used, depending on the case. To compare the measurements of the first and second moments, Student's t-test was used for related samples and the Wilcoxon test for paired observations. In the self-applied family burden scale (FBS), the results of the two moments were compared using the marginal homogeneity test. Lastly, a multivariate analysis was performed with repeated measures for each scale (FBS, FACES III) using the multivariate analysis of covariance (MANCOVA) model, where the dependent variables were the concepts evaluated within each scale and the independent variables, socio-demographic and clinical characteristics.
ResultsInitially, 336 subjects with bipolar disorder and schizophrenia were recruited, with 34 of them being excluded once the selection criteria were applied. Consequently, 302 subjects were evaluated, 198 diagnosed with bipolar disorder and 104 schizophrenia. After allocating the subjects to the two arms, the MI group consisted of 50 patients with schizophrenia and 100 with bipolar disorder and the TI group had 54 patients with schizophrenia and 98 with bipolar disorder. Fig. 1 shows the flow of patients during the study.
During the follow-up and intervention period, some participants were lost to follow-up and others withdrew, leaving a final sample of 259 patients: 92 with schizophrenia and 167 with bipolar disorder. This information is provided in detail in the patient flowchart (Fig. 1).
During the enrolment, follow-up and intervention period, there were no unintended injuries or effects in either of the intervention groups.
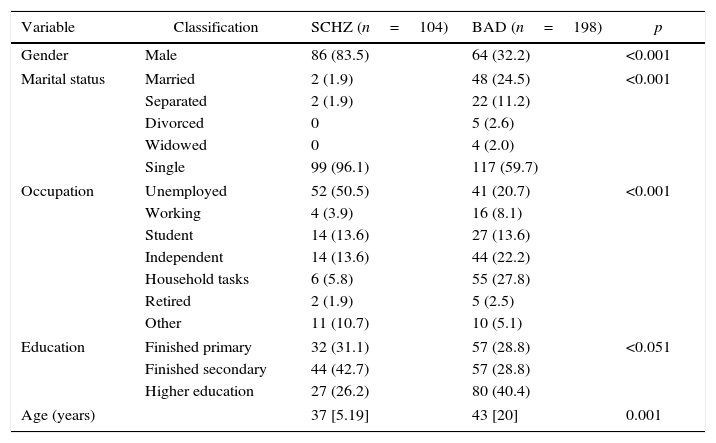
Socio-demographic characteristics of the patients with bipolar disorder and schizophrenia in the PRISMA programmeAfter evaluating the socio-demographic variables of patients with bipolar disorder and schizophrenia in the PRISMA programme, a high proportion of patients with schizophrenia were found to be male (83%) and among the patients with bipolar disorder, the majority were female (67.8%); mean age was 37 among patients with schizophrenia and 43 among patients with bipolar disorder. When marital status, occupation and educational level were evaluated, 96% of the patients with schizophrenia were found to be single, 50% unemployed and only 26% reported having higher education (technical, technological or for a profession). Of the patients with bipolar disorder, 59% were single, 20% unemployed and 40% had completed higher education. There were statistically significant differences in all four demographic variables (age, gender, marital status, occupation and education) (Table 1).
Socio-demographic variables of the patients with bipolar disorder and schizophrenia.
| Variable | Classification | SCHZ (n=104) | BAD (n=198) | p |
|---|---|---|---|---|
| Gender | Male | 86 (83.5) | 64 (32.2) | <0.001 |
| Marital status | Married | 2 (1.9) | 48 (24.5) | <0.001 |
| Separated | 2 (1.9) | 22 (11.2) | ||
| Divorced | 0 | 5 (2.6) | ||
| Widowed | 0 | 4 (2.0) | ||
| Single | 99 (96.1) | 117 (59.7) | ||
| Occupation | Unemployed | 52 (50.5) | 41 (20.7) | <0.001 |
| Working | 4 (3.9) | 16 (8.1) | ||
| Student | 14 (13.6) | 27 (13.6) | ||
| Independent | 14 (13.6) | 44 (22.2) | ||
| Household tasks | 6 (5.8) | 55 (27.8) | ||
| Retired | 2 (1.9) | 5 (2.5) | ||
| Other | 11 (10.7) | 10 (5.1) | ||
| Education | Finished primary | 32 (31.1) | 57 (28.8) | <0.051 |
| Finished secondary | 44 (42.7) | 57 (28.8) | ||
| Higher education | 27 (26.2) | 80 (40.4) | ||
| Age (years) | 37 [5.19] | 43 [20] | 0.001 | |
BAD: bipolar affective disorder.
The values are expressed as n (%) or median [interquartile range].
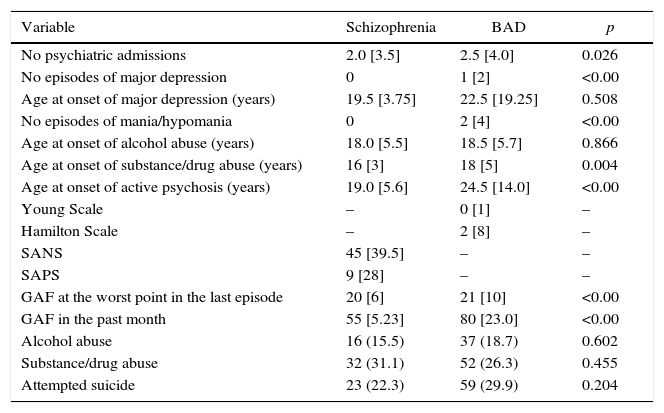
The group of patients with schizophrenia reported an average of 2 hospitalisations over the course of their lives, 15% had a history of alcohol abuse and 31% had a history of psychoactive substance abuse, with a mean age at onset of alcohol consumption of 18 and at onset of psychoactive substance abuse of 16. The average SANS and SAPS scores were 45 and 9 respectively, with a GAF score in the previous month of 55. In the bipolar disorder group, the mean number of hospitalisations was 2.5, with an average of 2 episodes of mania/hypomania and a GAF score in the previous month of 80; 29% had a history of suicide attempts and 26% a history of alcohol/substance/drug abuse.
Statistical differences between the two groups (schizophrenia and bipolar disorder) were found in the number of hospitalisations (p=0.026), the age of onset of substance/psychoactive drug abuse (p=0.004) and in the score on the GAF scale in the past month (p=0.001).
There were no statistically significant differences between the two groups in the following variables: alcohol abuse (p=0.602); psychoactive substance abuse (p=0.455); history of suicide attempts (p=0.204); and age of onset of alcohol abuse (p=0.86) (Table 2).
Variables by disorder.
| Variable | Schizophrenia | BAD | p |
|---|---|---|---|
| No psychiatric admissions | 2.0 [3.5] | 2.5 [4.0] | 0.026 |
| No episodes of major depression | 0 | 1 [2] | <0.00 |
| Age at onset of major depression (years) | 19.5 [3.75] | 22.5 [19.25] | 0.508 |
| No episodes of mania/hypomania | 0 | 2 [4] | <0.00 |
| Age at onset of alcohol abuse (years) | 18.0 [5.5] | 18.5 [5.7] | 0.866 |
| Age at onset of substance/drug abuse (years) | 16 [3] | 18 [5] | 0.004 |
| Age at onset of active psychosis (years) | 19.0 [5.6] | 24.5 [14.0] | <0.00 |
| Young Scale | – | 0 [1] | – |
| Hamilton Scale | – | 2 [8] | – |
| SANS | 45 [39.5] | – | – |
| SAPS | 9 [28] | – | – |
| GAF at the worst point in the last episode | 20 [6] | 21 [10] | <0.00 |
| GAF in the past month | 55 [5.23] | 80 [23.0] | <0.00 |
| Alcohol abuse | 16 (15.5) | 37 (18.7) | 0.602 |
| Substance/drug abuse | 32 (31.1) | 52 (26.3) | 0.455 |
| Attempted suicide | 23 (22.3) | 59 (29.9) | 0.204 |
BAD: bipolar affective disorder.
The values are expressed as n (%) or median [interquartile range].
After comparing the demographic (gender, marital status, occupation and educational level) and clinical characteristics of the subgroups of patients with bipolar disorder and schizophrenia assigned to MI and TI, statistically significant differences were only found in the educational level of the bipolar disorder group in the MI programme, where 50% of the patients had some level of higher education compared with 29% of the TI group (p=0.044). There were no statistically significant differences between the subgroups of patients with bipolar disorder in the Hamilton and Young scale scores or between the subgroups of patients with schizophrenia in the SAPS and SANS scores. There were no differences in the scores for functionality in the past month between the MI and TI subgroups for patients with bipolar disorder or schizophrenia.
Emotional involvement and criticism according to FEICS in families of patients with schizophrenia or bipolar disorder at the beginningIn the family criticism domain of the FEICS, 27% of patients with schizophrenia and 21% of subjects with bipolar disorder gave their family a “high” criticism score. According to the family members’ ratings, the level of criticism in both groups was lower than that reported by the patients. In the group with bipolar disorder, 16% of the relatives rated the level of criticism as “high” and 42% as “low”. There were no statistically significant differences in the FEICS criticism score level between patients with bipolar disorder and patients with schizophrenia (p=0.468), or between the families of each group (p=0.508). It is important to point out that more than 40% of the relatives classified the level of family criticism as “low”. No statistically significant differences were found between the two groups of patients in total scores for family criticism.
When the FEICS domain of over-involvement was evaluated, statistically significant differences were found between the scores of the relatives of patients with bipolar disorder and those of patients with schizophrenia (p=0.030). Involvement considered “high” was greater in the bipolar disorder group (26%) than in the schizophrenia group (14.3%). The patients’ scores for this domain showed a higher level of over-involvement in the schizophrenia group than in the bipolar disorder group (p=0.058). No statistically significant differences were found between the two groups in the total involvement scores.
Cohesion and adaptability according to FACES III in families of patients with schizophrenia compared with families of patients with bipolar disorder at baselineA difference between the two groups was found in the total family adaptability score on the scale completed by the patient, with a higher median score in the schizophrenia group (p=0.051). No statistically significant differences were found in the other total cohesion and adaptability scores or in the scores for these subdomains. In the adaptability scores there was a tendency to find differences, but they were not statistically significant (p=0.092).
Family burden for patients with schizophrenia compared with patients with bipolar disorder at baselineWhen the objective burden of the relatives was measured, 95% of them (bipolar disorder and schizophrenia) reported “moderate burden” or “severe burden”. One in every 4 of the patients’ relatives reported having “severe objective burden”. When assessing the attribution of the burden (emotional, work, leisure, relational, economic and at home) to the patient's health status, only 15% of the relatives found a “clear relationship”. Fifty-three percent (53%) of the relatives of patients with bipolar disorder found “no relationship” between the burden and the patient's health status. When comparing the scores for this scale from the bipolar disorder and schizophrenia groups, no statistically significant differences were found.
Comparison between baseline and end of intervention of the FACES III and FEICS scores for patients with bipolar disorder and schizophreniaWhen comparing the FACES III and FEICS between baseline and end of intervention for patients with bipolar disorder in each of the intervention arms (MI vs TI), an improvement in the total family cohesion score was identified in the MI subgroup (p=0.041) that was not observed in the TI group. No statistically significant differences were found between the two subgroups in the adaptability domain or on the FEICS scale. The TI group showed significant changes in the variables of adaptability (p=0.024) and cohesion (p=0.021) on the scale applied to the relatives. However, these significant differences were not identified after performing a MANCOVA.
After comparing the patients with schizophrenia assigned to the MI subgroup at baseline and at the end of the intervention, an increase in family involvement score was observed (p=0.017) that was not observed in the TI group. No changes were found in the criticism domain in either intervention arm. In the TI group, a significant increase in the adaptability score was observed according to the scores recorded by the relatives (p=0.023). These differences did not persist after the multivariate analysis.
DiscussionThe results in this article form part of the report on a mental health programme focusing on reducing burden, suffering and social spending in mental illness (PRISMA) for patients with schizophrenia and bipolar disorder who were randomly assigned to an MI or TI. The primary objective of this part of the research was to assess changes in family dynamics after treatment. The groups of patients with bipolar disorder and schizophrenia assigned to each of the treatment arms (MI and TI) had similar demographic and clinical characteristics, and had adequate randomisation.
In the scores for the Caregiver Burden Scale (CBS), cohesion and adaptability (FACES III) and over-involvement and criticism (FEICS) at the beginning of the programme, a higher level of criticism was observed in patients with bipolar disorder than in patients with schizophrenia compared with their relatives; although the difference was large, it did not reach statistical significance in the end. When assessing the carer's burden with the CBS scale, it was observed that 1 in 4 patients with bipolar disorder and schizophrenia had “high objective family burden” (emotional, work, leisure time, relational, economic and at home), but when that burden was correlated with the patient's condition, only 50% on average considered that there might be “some relationship” or “a clear relationship” between the burden and the patient's illness. Close to 94% of the relatives reported having “some burden”.
Comparing the CBS, FACES III and FEICS scores at baseline and at the end of the intervention in the group assigned to the MI, we found some significant differences in family cohesion in the bipolar disorder group and adaptability in the schizophrenia group, although they did not persist after the multivariate analysis. In this research, the MI showed no benefit over the TI in modifying the variables of carer burden, cohesion, adaptability, over-involvement and family criticism. In view of the characteristics of the treatment, as the same patient might receive several interventions by different therapists within the same period of time, there was a possibility of variables worsening, as the therapy exposes issues and situations which are highly emotionally charged. However, this phenomenon did not occur, i.e. the MI did not make family dynamics worse.
Among the possible explanations for not finding significant differences, the authors propose the following hypotheses: (a) to see changes in family dynamics and therapeutic results from family therapy generally requires more extensive and continuous processes, and in this MI patients had other interventions included in their programme; more frequent and longer lasting interventions may be needed in this population to achieve better therapeutic effects; (b) the instrument used to measure the effect of the multimodal programme on family dynamics did not capture the variables in which there might have been changes, and other psychometric instruments should therefore be explored in the future; and (c) this study made predominantly quantitative measurements, but a narrative and qualitative approach might have identified significant changes in family dynamics that are difficult to quantify with the tools used. It is important to emphasise this last hypothesis, because strikingly, many of the patients and relatives who participated in the programme showed a high degree of satisfaction and recognised improvements in their processes. This breakthrough was also recognised by the family therapist who accompanied and assessed the patients and their relatives throughout the process.
The authors acknowledge that despite its strengths, such as sample size, adequate randomisation, design of individualised treatment programmes, management of a very sick population and the use of highly experienced therapists, this study also has its limitations. The most important limitations include the absence of masking to therapists and evaluators, and the lack of control of other parallel interventions that might have positively or negatively affected the final outcome. This was a population sample with heterogeneous pharmacotherapy and medical and psychiatric comorbidity, and high consumption of psychoactive drugs, meaning that all patients had some other type of care in their healthcare system which could not be eliminated from the study for economic and ethical reasons.
ConclusionsThis study showed no differences in the variables of family burden and family functioning in patients with bipolar disorder and schizophrenia who were in an MI programme compared with patients in the TI programme. Future studies might include longer periods for remaining in the MI and more frequent appointments and, additionally, they might explore family dynamics with other instruments to achieve greater effects.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThis project was funded by COLCIENCIAS, CODI-Universidad de Antioquia and Hospital Universitario de San Vicente Fundación.
Conflict of interestsNone.
The authors would like to thank COLCIENCIAS, CODI-Universidad de Antioquia, Hospital Universitario de San Vicente Fundación and PRISMA U.T.
Please cite this article as: Ramírez A, Palacio JD, Vargas C, Díaz-Zuluaga AM, Duica K, Agudelo Berruecos Y, et al. Emociones expresadas, carga y funcionamiento familiar de pacientes con esquizofrenia y trastorno afectivo bipolar tipo I de un programa de intervención multimodal: PRISMA. Rev Colomb Psiquiat. 2017;46:2–11.