The Covid-19 pandemic has generated an unprecedented multimodal (health, occupational, economic, and social) crisis, which will impact developing countries. Confinement as a preventive measure is itself a threat that produces a social impact. Pandemic and confinement have become a psychosocial adversity factor that affects families and their children. During the pandemic, children and adolescents with a psychiatric disorder may experience exacerbation of their symptoms. However, little is known about this, since studies on this population during the pandemic are scarce.
ObjectiveTo review the data available in the current literature on the effect of the pandemic on children and adolescents with a previous psychiatric disorder.
MethodsA literature search was carried out using PubMed, Scielo and, due to the exceptional conditions of the pandemic situation, directly using internet search engines. Both English and Spanish papers were included.
ResultsThe information found is presented in the following sections: family and children during the pandemic, evaluation of mental disorders in children and young people during the pandemic, pre-existing psychiatric disorders during the pandemic, and telepsychiatric care. Specific information is presented on attention deficit hyperactivity disorder, autism spectrum disorder, intellectual disability, anxiety disorder, obsessive compulsive disorder, and post-traumatic stress disorder. The current pandemic due to COVID-19 and confinement are a psychosocial adversity that threatens the stability of the family. Such a stressor can cause exacerbation of symptoms of a previous mental disorder. Children and adolescents with psychiatric disorders are a vulnerable population and require specialised care. Telepsychiatry is becoming a modality with multiple advantages.
La pandemia por Covid-19 ha generado una crisis multimodal inédita: sanitaria, laboral, económica, social, que repercutirá especialmente a los países en vía de desarrollo. El confinamiento como medida preventiva es su vez una amenaza que producen un impacto social. Pandemia y confinamiento se han convertido en un factor de adversidad psicosocial que afecta las familias y sus hijos. Durante la pandemia, los niños y adolescentes con un trastorno psiquiátrico podrían presentar exacerbación de sus síntomas. Sin embargo, poco se conoce al respecto, pues los estudios sobre esta población durante la pandemia son escasos.
ObjetivoRevisar los datos disponibles en la literatura actual acerca del efecto de la pandemia sobre los niños y adolescentes que presentan un trastorno psiquiátrico previo.
MétodosSe realizó una búsqueda de la literatura a través de PubMed, Scielo y, por las condiciones excepcionales de la situación de pandemia, de manera directa en buscadores de internet. Se incluyeron artículos en ingles y español.
ResultadosLa información encontrada se presenta en los siguientes apartados: la familia y los hijos durante la pandemia, evaluación de los trastornos mentales en niños y jóvenes durante la pandemia, trastornos psiquiátricos preexistentes durante la pandemia, y atención en telepsiquiatría. Se presenta información específica sobre el trastorno por déficit de atención e hiperactividad, trastorno del espectro autista, discapacidad intelectual, trastorno de ansiedad, trastorno obsesivo compulsivo y el trastorno por estrés postraumático. La pandemia actual por COVID-19 y el confinamiento son una adversidad psicosocial que atenta contra la estabilidad de la familia. Tal estresor pude causar exacerbación de los síntomas de un trastorno mental previo. Los niños y adolescentes con trastornos psiquiátricos son una población vulnerable que requiere de una atención especializada. La telepsiquiatría se convierte en una modalidad con múltiples ventajas.
The world is facing one of the most important global challenges since the second world war: the coronavirus disease 2019 (COVID-19). This epidemic outbreak began in December 2019, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1
We are currently facing a situation with tragic consequences, the COVID-19 pandemic that was declared a public health emergency by the WHO.2 An unprecedented multi-faceted (health, occupational, economic and social) crisis that will particularly impact developing countries. The preventive measures for avoiding catching the virus include social distancing and confinement, which also constitute a different type of threat as they produce a major impact on society.3
Resilience is defined as the capacity to cope with environmental circumstances that probably require of children a significant degree of psychological, social or neurobiological adaptation and that constitute a deviation from the expected environment.4 Adverse childhood experiences are common. For example, some studies show that up to 66.7% of adolescents have experienced at least one adversity, and almost 50% more than one. The most frequently reported adversities are illnesses affecting the parents (24%), financial difficulties (22%), family discord (18%) and parental alcohol consumption (17%).5–7 During pandemics, the scale of these adversities may increase.
Rutter8 was one of the first authors to point to the role of psychosocial adversity in the aetiology of mental disorders. He revealed that the development of psychopathology was associated with other factors of adversity that a child will have.9 Subsequent studies with his group identified the adversity indicators,10 and considered six family and environmental characteristics: low social class, serious marital discord, families with more than four children, paternal criminality, paternal mental disorder and a stay in a care home. The presence of two factors increases the likelihood of mental disorders by up to four times, and four factors by up to ten times.10 Few studies in Latin America have studied this association between psychosocial adversity and mental disorders, although they do confirm this relationship.11
Studies in children during this pandemic are scarce. One study reports that factors such as a prolonged quarantine, fear of infection, frustration and boredom, the lack of contact with classmates and teachers, the lack of space at home and the loss of loved ones generate psychological repercussions in children and adolescents.12
The objective of this article is to review the available data in the current literature about the effect of the pandemic in children and adolescents who already have a psychiatric disorder.
MethodsA literature search was performed on PubMed, SCIELO and, on account of the pandemic's exceptional conditions, directly in search engines such as Google and Safari. This search yielded information from official specialised organisations and those dedicated to child and adolescent psychiatry and worldwide public health topics, such as the World Health Organisation (WHO) the American Academy of Child and Adolescent Psychiatry (AACAP), the United Nations Children's Fund (UNICEF) and the Instituto Colombiano de Bienestar Familiar (ICBF) [Colombian Institute of Family Welfare]. No date limitation was placed on the articles found and only articles published in English and Spanish were included. The bibliographic references of the articles located were also reviewed in order to expand the sources of information. The following keywords were used for the search: pandemic, COVID-19, children, adolescents, family, risk factor, emotional stress, telepsychiatry, mental telehealth, telemedicine, attention deficit-hyperactivity disorder, autism spectrum disorder, neurology, bipolar, anxiety, schizophrenia, intellectual disability, oppositional defiant disorder, psychosis, anxiety, phobia, depression and bereavement. Combinations of these keywords in English and Spanish were also used.
ResultsThe data obtained from the search about pre-existing psychiatric disorders in children and adolescents during the COVID-19 pandemic are presented.
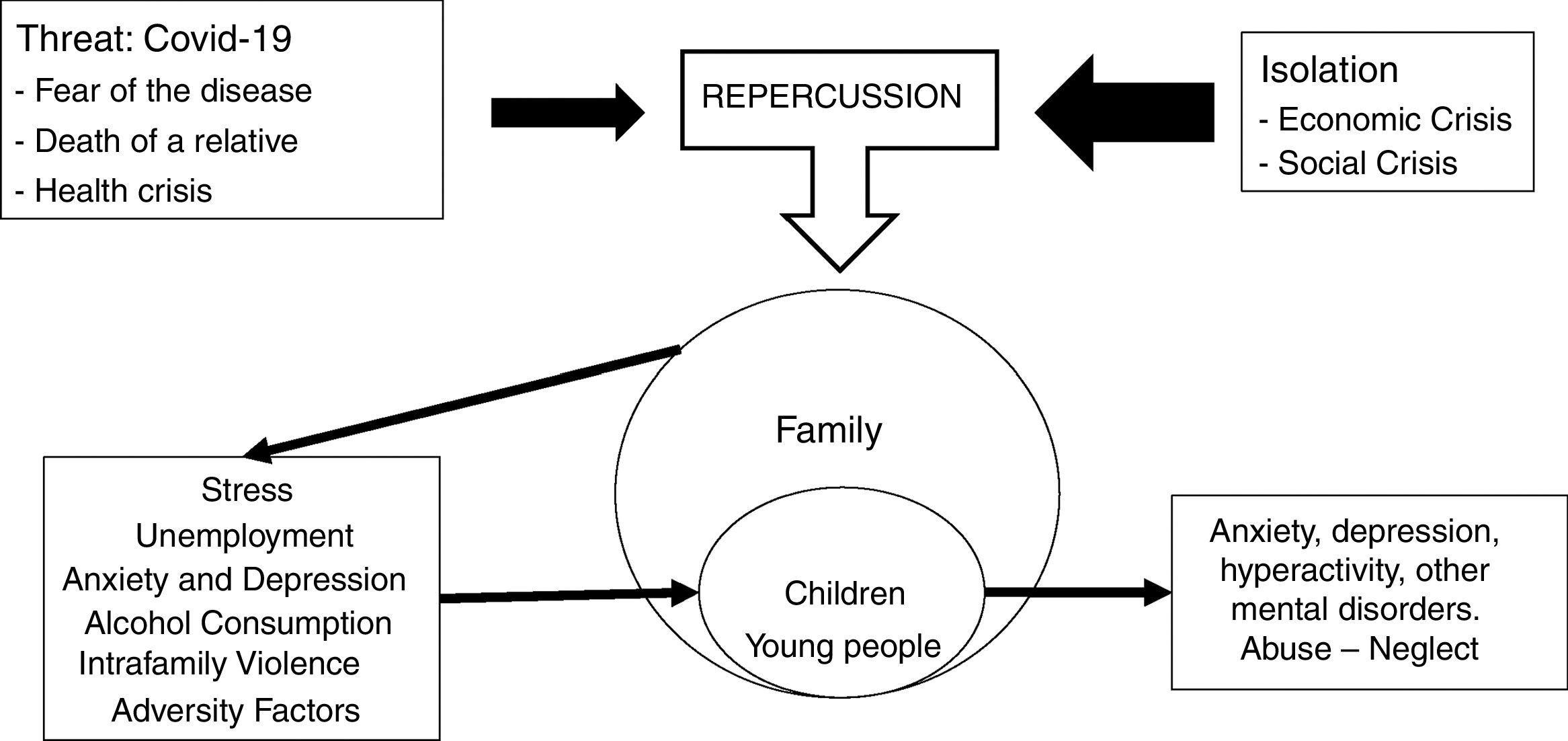
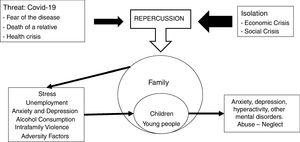
Families and children during COVID-19The coronavirus and COVID-19 are a threat with complex characteristics and an uncertain duration that has led numerous countries to introduce a mandatory lockdown.13 The repercussions in the social context stemming from the dynamic between the threat (the virus) and the preventive measures (lockdown) exert a pressure that ultimately affects the family nucleus. Lockdown, meanwhile, is a measure that has generated high rates of unemployment and a lack of livelihood for self-employed workers. A long lockdown and the imposition of restrictions on freedom are risk factors for a greater psychological impact.14Fig. 1 displays the relationship between the different elements.
Families have undergone abrupt and highly impactful changes in the course of the pandemic. Moreover, prolonged lockdown and unemployment increase the risk among parents of greater consumption of alcohol and other substances, partner abuse, family discord, child abuse and sexual abuse.12 Lockdown involves continuous cohabitation with other people that necessitates a change in the family dynamics. Families already exposed to intrafamily violence will continue to have a latent risk, and the more financial difficulties the abusers have and the longer the lockdown lasts, the more possibilities there will be for abuse.15,16 During this pandemic, China presented a greater number of cases of depression and anxiety in adults,17 which are potential factors of adversity for cohabiting children and adolescents.
In general, children cope better with such situations if they have a stable and serene adult by their side. However, besides the factors related to the family environment, individual factors must also be considered: characteristics of the child (such as temperament), history of adversity, coping and resilience, which all together will modulate the response to the threat. For some children, the closure of schools entails factors such as not having access to education and food, a lack of face-to-face contact with their schoolmates and significant teachers, and being unable to carry out their sport and leisure activities, among other things.18
Evaluation of mental disorders in children and young people during the pandemicThere are certain common considerations for the evaluation and treatment of young people with different mental disorders in the context of COVID-19.19–23 Those collected in the recent literature are shown in Table 1.
Considerations for the evaluation and treatment of young people with different mental disorders in the context of COVID-19.19–23
| • Apply the strategies and recommendations intended for young people in the general population to maintain physical and mental health |
| • They are more vulnerable to the negative psychological effects of the pandemic and lockdown |
| • Behavioural problems may occur that affect compliance with social distancing measures |
| • They are more likely to have frequent contact with family members, caregivers, professionals and people in the community |
| • They could have systemic comorbidities that increase the risk of COVID-19-related complications |
| • They need to continue to have the same intensity of care provided by health professionals as before Telehealth strategies are recommended57 |
| • Be on the lookout for signs of stress in patients, family members and caregivers |
| • Ask caregivers to try and maintain a positive or neutral emotional expression as much as possible, since young people can learn to copy their parents’ coping strategies |
| • Offer pharmacological treatment if it is indicated If the patient is already on medication, they should continue as before |
| • Barriers to access or continuation of treatment may increase the risk of COVID-19 infection due to poorer behavioural control |
| • Patients or caregivers should avoid increasing medication doses on their own initiative |
| • Requests for additional medication should be analysed carefully, taking into account the context and impact of COVID-19 on the setting and treatment |
| • Non-pharmacological behavioural interventions are preferable to dose adjustments or the addition of new medications |
| • If additional medication is required, ensure regular monitoring by the treating team |
| • Pay special attention to the application of depot injections and determinations of the serum concentration of the drugs, since these activities could increase the risk of transmission of the virus |
| • Draw up a risk-benefit balance of the need for face-to-face care |
| • Give careful consideration to the need for hospitalisation, duly weighing up the risk to the young person and the impact upon the department |
| •If hospitalisation or critical care is required, the person and their family must be provided support to help them understand and manage the process |
The literature in this field is rather scant. The rapid spread of the pandemic has limited the performance of longer-lasting and better quality studies. The bulk of the literature is comprised of editorials, expert opinions and consensus documents issued by organisations. The existing publications about the most notable groups of mental disorders in childhood and adolescence are referred to below.
Attention deficit-hyperactivity disorder (ADHD)The European ADHD Guideline Group published a guide for the treatment of these patients during the pandemic.20 Families are advised to use behavioural strategies for parents to improve their care and to reduce opposing, defiant and disruptive behaviour.24 They could also try self-help25–27 or online28 versions of certain evidence-based treatments, being careful with the use of untested mobile applications. Those receiving other non-pharmacological therapies should be encouraged to continue doing exercises that can be transferred to the new activities.
Face-to-face cardiovascular risk screening could be postponed until further notice, since the risks outweigh the benefits. If possible, heart rate and blood pressure should be taken with household devices following the relevant guidelines.20 In the event of any cardiovascular symptoms (e.g. chest pain, prolonged palpitations and breathing difficulty) or any other worrying symptoms, the treating physician should be contacted.
Few recommendations are made about pharmacological treatment of ADHD. The use of antipsychotics and sedatives to treat disruptive behaviour should be limited whenever possible. Moreover, since confinement and social distancing can exacerbate the risks related to ADHD, there is no compelling reason to introduce “medication holidays” during this crisis.29
Initial insomnia may be an adverse effect of stimulant treatment, although it could also be caused by pandemic-associated factors (stress, getting up late, disruption of routines, etc.). Proper sleep hygiene should be ensured before considering the initiation or adjustment of hypnotic drugs (such as melatonin up to 5–6mg/night).30
Headache is a possible adverse effect of psychopharmacological treatment, and acetaminophen is recommended for this or other pains. There is uncertainty as to the possible unfavourable effects of ibuprofen in COVID-19 patients.31
Autism spectrum disorders (ASD)Young people with ASD require multimodal treatments and usually participate several hours a week in interventions with specialised therapists at home, in the hospital or in specialised centres. During lockdown, they may possibly not receive the same face-to-face support from therapists or outside interventions.
The doctor of psychology Antonio Narzisi, from the Department of Child Psychiatry and Psychopharmacology of the Stella Maris Foundation of the University of Pisa (Italy), published a set of tips to help the caregivers of children with ASD during the lockdown period21 (Table 2).
Tips to help caregivers of children with ASD during lockdown.
| • Explanations should be kept simple and specific58 |
| • Augmentative and alternative communication may be used |
| • Ask therapists for help in preparing material |
| • For verbal young people, the explanation can be supported with conceptual maps |
| • Subdivide daily activities59 |
| • Use a different room for each activity |
| • The activity can be presented as a family game |
| • Use a board to write down scheduled activities |
| • Schedule game activities60 |
| • They can be individual or involve the family61 |
| • Choose the activities that the child prefers |
| • A good example are activities with pieces to assemble62,63 |
| • Use serious games (ones in which the purpose goes beyond mere entertainment, such as education, learning skills or behavioural changes)64,65 |
| • Educational alternative for video games or online games. Many of them are free and can be downloaded as mobile apps |
| • Share video games or internet66 |
| • Do not try to stop children from playing on the computer |
| • It is useful to establish a rule about sharing video games or internet |
| • This could reduce the risk of isolation or internet addiction |
| • Support and share special interests67 |
| • Plan some family activities in order to share these interests |
| • Contact with classmates and teachers68 |
| • At least one weekly contact with a classmate and a teacher |
| • The modality will depend on the young person's preferences |
| • Options: a letter, telephone call or video call69 |
| • An appropriate amount of free time should be allowed during the day |
Young people with ASD frequently present anxiety disorders32 and lockdown can be difficult for them to assimilate. During confinement, they may experience an increase in stereotypies in the initial phase, which appears as adaptive behaviour that will gradually disappear. Nevertheless, they may also demonstrate increased movements, as outings to places they formerly enjoyed going to be postponed. Similarly, their parents experience a greater degree of stress and susceptibility than parents of children with other disabilities.33
One follow-up option for therapists is to make videos about the child's behaviour during free play or structured sessions at home. This allows them to monitor the patients.
Intellectual disability (ID)The Faculty of Intellectual Disability Psychiatry of the Royal College of Psychiatrists of the United Kingdom published a guide on COVID-19 and persons with intellectual disability.19
Young people with ID or intellectual development disorder are at significant risk of infection due to a greater prevalence of systemic comorbidities, their personal habits, and the fact that some of them live in communal settings with constant exposure to other people (on account of the degree of support they require). They are also more vulnerable to changes in care.
Although the impact of the pandemic, lockdown and changes in the mental health care of these young people, and on their families and caregivers is still uncertain, it could generate an increase in malaise, disruptive behaviours, health-related anxiety and the onset of mental disorders or the exacerbation of existing ones.
It is proposed to identify families at greater risk or more vulnerable, such as those with young people who returned home from institutions or those whose housing is at risk. The recommendation is to work in collaboration with the social work team.
Children and adolescents with ID are among the most vulnerable due to their need for high-level clinical care in hospital services. Engaging them in treatment and recovery in the context of social distancing, particularly with those who contract the infection, is a challenge for staff. Some subjects will require physical or pharmacological restraint if they show agitation during lockdown, a measure that the treating psychiatrist should indicate on an individual basis.
Some critical care guidelines34 propose determining frailty to guide access to treatment. However, people with ID are more likely to obtain higher scores on frailty scales, without this necessarily meaning that they are less stable, which can also result in a disadvantage.
All patients should have a health action plan and a hospital passport with details about their health situation that increases their vulnerability to the complications of COVID-19. Ideally, staff trained in the treatment of patients with ID should be on hand to accompany them during the hospitalisation process. Finally, people with ID should be ensured equal access to health interventions.
Anxiety disordersThe child psychiatrist Nicola Keyhan published an article on the Canadian Paediatric Society website explaining how to provide support to young people with anxiety disorders during this pandemic.23 The strategies are summarised in Table 3.
Specific tips for the treatment of young people with anxiety disorders and pre-existing OCD in the COVID-19 context.
| Tips for providing support to young people with anxiety disorders during the COVID-19 pandemic23 |
| Minimise exposure to situations that generate great fear |
| Do not over-focus on prevention behaviours (e.g. hand washing) |
| Maintain normal routines |
| Insist on the ability to cope with the situation |
| Talk about the situation with the young people |
| Ask them what they know and their doubts about the pandemic |
| Correct information errors |
| Give reflexive, honest and reassuring answers, suited to their age |
| Avoid going into too much detail |
| Explore and validate thoughts and emotions |
| Ask about the experience of physical discomfort (it could indicate anxiety) |
| Limit exposure to information focused on negative aspects |
| Coping strategies can be used to reduce anxiety |
| Deep breathing |
| Muscular relaxation |
| Imagery |
| Mindfulness |
| Specific strategies for improving dysfunctional thinking patterns for young people with a developmental age of at least 8 years: |
| • Identify anxious thoughts and put them to the test |
| • Demonstrate how certain thoughts can lead to overestimating the possibilities of fears materialising |
| • Channel them towards more realistic thoughts |
| • Ask the children to write down their concerns |
| • Help them to think about the evidence in favour and against these concerns |
| • Propose more balanced and optimistic views of the situation |
| • Remind them that, by respecting social distancing and prevention measures, people are doing a lot to protect themselves |
| • Explain to them that there are resources for people who get sick to help them overcome the infection |
| Specific tips for parents of young people with OCD in the context of the COVID-10 pandemic22 |
| For young people obsessed with infection or health-related issues or with cleaning or hygiene compulsions: |
| • It may help to explain how the general public health guidelines (e.g. hand washing) can be compatible with their treatment plan |
| • Therapists can be asked for help on how to do it |
| For young people who ask questions about COVID-19: |
| • Parents should be ready to answer them |
| • Not all questions imply a search for reassurance |
| • They are likely to be seeking reassurance if they ask the same question repeatedly or press for an answer or need one immediately |
| • If they are seeking reassurance, tell them that it may heighten their anxiety |
| • If there are doubts as to how to proceed, ask the therapist for help |
| If the young person begins to seek reassurance about future uncertainty: |
| • Try activities that connect them to the present (e.g. cooking, puzzles, etc.) |
| • Limit exposure to the media that talk about COVID-19 |
| • Caregivers should be responsible for providing information |
People with anxiety disorders may encounter great difficulties in adapting to current changes. Particularly those with a fear of disease may have a worsening anxiety about becoming infected and engage in excessive hand washing. This concern may continue even after the quarantine period is over. Some children with separation anxiety may become overly attached to their caregivers during the pandemic and may find it difficult to return to school. Anticipating changes and transitioning can be part of the plan for resuming activities.23 Moreover, factors such as intrafamily violence may trigger anxiety crises in these patients.35
When they return to their activities at school, patients with social phobia may have a new outbreak on account of having spent so much time avoiding exposure due to confinement or having their face partially covered (with a mask).
Obsessive-compulsive disorder (OCD)Symptoms such as adaptive reaction may increase in patients with obsessive-compulsive disorder, although with support they can revert to their previous status. The virtual support group of the International Obsessive-Compulsive Disorder Foundation designed some specific tips for the parents of young people with OCD in the context of this pandemic22 (Table 3).
Post-traumatic stress disorder (PTSD)Sprang and Silman compared PTSD symptoms in quarantined parents and children versus non-quarantined controls. They found that post-traumatic stress scores are four times greater in quarantined than non-quarantined children. There were more symptoms in the quarantined group (28% versus 17%).36
During lockdown, some children will be exposed to family discord, child or sexual abuse12,15,16, stressful adverse events that could trigger an acute stress disorder or PTSD.
Other disorders and COVID-19Although no specific literature was found about other mental disorders, it is believed that subjects with some type of severe mental disease, such as schizophrenia, psychotic disorders or bipolar affective disorder, will be exposed to factors that can trigger crises that will require hospitalisation, with all the risks that this implies during the pandemic.
Moreover, in other mental disorders, symptoms could increase during the pandemic, which is why they are mentioned below.
The expression of symptoms in patients with oppositional defiant disorder (ODD) and conduct disorder (CD) may change depending on the family and social setting. Parental management skills are put to the test during confinement. Homes presenting a higher adversity index will witness an increase in ODD behaviour. Genetic and environmental factors behave as protectors or as factors in the onset of ODD in childhood.37 Families with a child with ODD will have to cope with the child's reactions to the limits imposed.
It should be considered that while certain antisocial behaviours in adolescents during the pandemic (such as stealing) may be regarded by their parents as adaptive, they are still part of the path towards a conduct disorder.38 In confinement prompted by previous epidemics, adolescents were seen to present difficulties in observing the measures proposed during isolation. They “break quarantine”, which makes them a group at risk of antisocial behaviours and consumption of alcohol and substances.39
Sleep disorders such as insomnia may increase on account of several factors: changes in sleep hygiene habits, reduced physical activity, increased exposure to the light (screens) and exposure to video games and television programmes.
Subjects with a history of major depressive disorder (MDD) are at risk of having a new episode due to possible losses, not just because of the economic crisis, but also the possible death of family members. Due to the treatment protocols applied to patients with COVID-19, the isolation of the corpse and barriers to performing a funeral ritual are risk factors for a relapse of MDD or a complicated bereavement.40
The neurological diseases were addressed in the review, since some of them may constitute differential diagnoses of behavioural disorders, whereas others may involve comorbidity with other psychiatric disorders. According to the European Academy of Neurology, as yet there is no evidence of affection of the nervous system by SARS-CoV-2 in children. However, the infection's characteristics constitute a risk to children affected by chronic neurological diseases.41 Evidence is beginning to appear that SARS-CoV-2 may cause neurological complications such as cerebral inflammation, encephalitis, delirium and cerebrovascular complications, among others.42,43 Finally, there is a risk of infection and of serious respiratory diseases for children with neuromuscular disorders, immunosuppressive therapies, rare diseases, and inborn errors of metabolism and neurodevelopment disabilities.41
Telepsychiatry with children and adolescentsAn alternative during the pandemicThe barriers to specialised care in paediatric psychiatry have increased exponentially during this coronavirus crisis. Travel difficulties, the risk of contagion at health facilities, the suspension of numerous consultation services and the already difficult task of obtaining an appointment all make it more difficult to see a child and adolescent psychiatrist. In this scenario, the resource of telemedicine comes into play, and more precisely, psychiatry in the form of interactive consultation.44
Telepsychiatry with children and adolescents consists of using telecommunications and information technology to provide access to psychiatry services targeting the paediatric population. This modality must include at least audio and video.45 For some specialists this is a novelty, although the field is not new and has been in development for several years. The use of telemedicine results in lower costs, ease of access, correct diagnoses and effective treatments. Not only has it been used in general medicine, it has also been applied in emergency rooms, paediatric critical care units and in community psychiatry.45–47
Although acceptance of the service is favourable and has been documented in surveys about telepsychiatry with patients, relatives and healthcare personnel,48 it presents certain limitations compared to in-person consultations, such as the lack of face-to-face contact, partially-absent body language, absence of physical contact and change in emotional expressions.45
Besides the aforementioned considerations, it must be noted that of all the different telepsychiatry models, the most accepted and effective one is that which involves local mental health personnel who can facilitate the communication process and also monitor the patient, either via this modality or in person in the future.49
The experience of telepsychiatry in the worldSeveral new experiences have been reported with this modality in the current pandemic. A greater move towards telepsychiatry services has taken place in different parts of the world. From the beginning of the lockdown in China, both the government and academic organisations implemented support, supervision, training and psychoeducation services for the general population through digital channels. In Australia, specialised consultations in mental health are provided virtually to vulnerable groups and the system is currently being expanded to the general population. Similarly, in Europe, mental health services are moving towards telepsychiatry-based care.50–53 In the Latin American setting, in Colombia, the telepsychiatry programme of the University of Antioquia, developed jointly with the Living Lab, which had already successfully been providing mental healthcare, has implemented a care strategy for the general public and health personnel, providing psychological first aid, and psychological and psychiatric consultations for adults and the paediatric population.54
Recommendations for implementing telepsychiatryTelepsychiatry consultations will probably be effective, adequate and accepted by parents and children, and will serve as an input to continue the follow-up with the same modality, considering the duration of the pandemic.
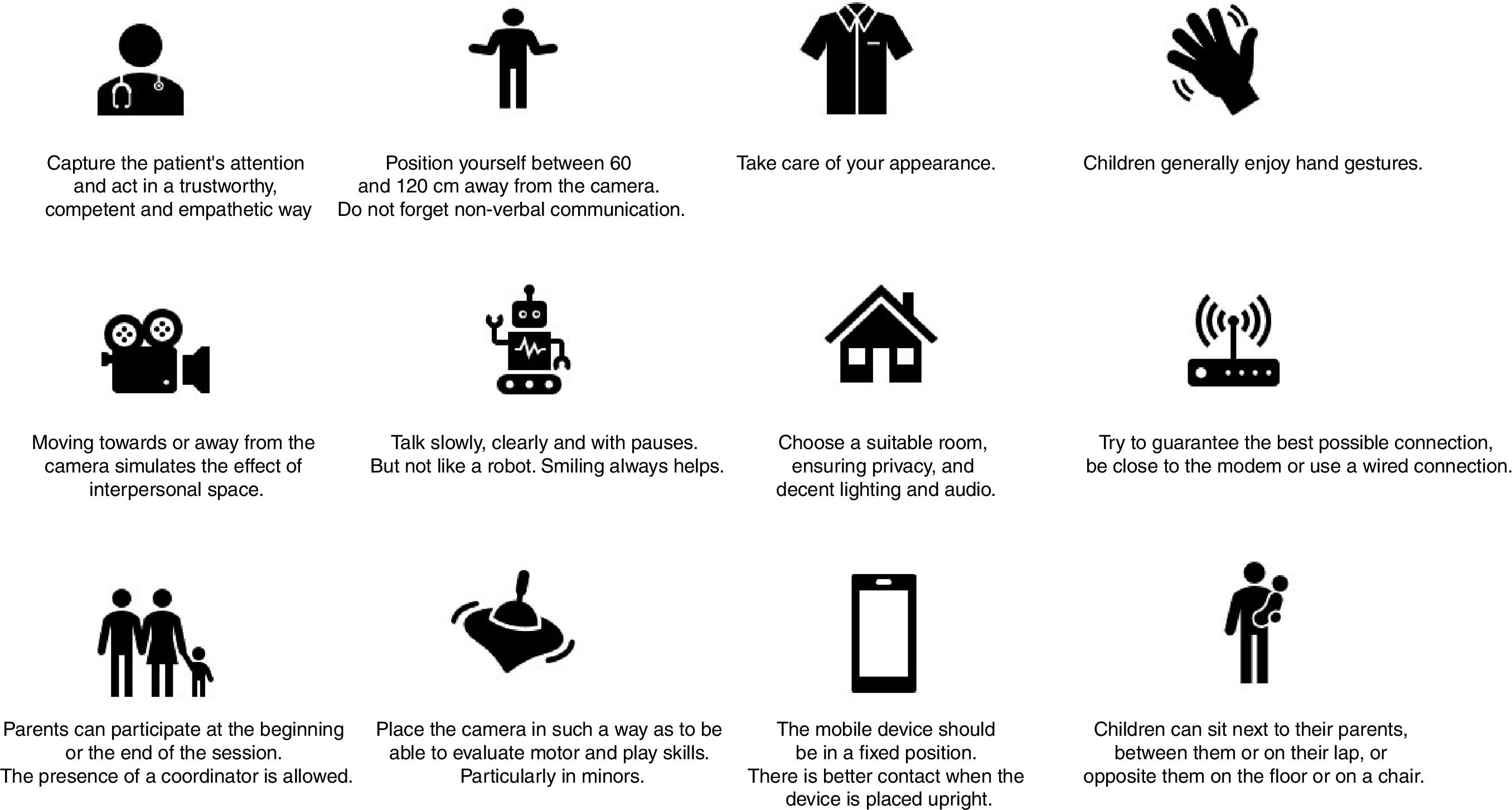
The pandemic is forcing us to implement alternatives to face-to-face consultation, and it is the right time to apply telepsychiatry, but certain considerations should be taken into account in order to successfully adapt to this new consultation context. Fig. 2 describes some tips conducting a telepsychiatry consultation.
Practical tips for telepsychiatry care of children and adolescents.
Readers are recommended to consult the current telepsychiatry guidelines for children and adolescents to expand on the topic.55,56
ConclusionsThe current COVID-19 pandemic and lockdown threaten to exacerbate symptoms in children and young people with a prior psychiatric disorder. This occurs within a family dynamic affected by an economic and social crisis. Although there is no exact evidence about the effects of the current pandemic, children and adolescents with psychiatric disorders are a vulnerable population that requires monitoring and interventions by specialised personnel. The current barriers and risks lead to care during the pandemic ideally being provided through telepsychiatry.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Palacio-Ortiz JD, Londoño-Herrera JP, Nanclares-Márquez A, Robledo-Rengifo P, Quintero-Cadavid CP. Trastornos psiquiátricos en los niños y adolescentes en tiempo de la pandemia por COVID-19. Rev Colomb Psiquiatr. 2020;49:279–288.