The increasing prevalence of obesity or overweight at all ages, their associated morbidity and mortality associated, and the increased perception of the problem by the society have generated several hypotheses in response to the scientific and the international community.
ObjectiveInvestigate the preventive interventions in childhood obesity so far.
MethodsIntegrative review during the study period from April 2013 to November 2014. The MEDLINE international database was used, including PubMed, the Cochrane Library (Issue 4 2002), the national database Isooc (CSIC) national database, as well as the Internet. The review included health articles published in Spanish and English between 1990 and 2014 that focused on or included education, prevention, diagnostic, and treatment of obesity interventions.
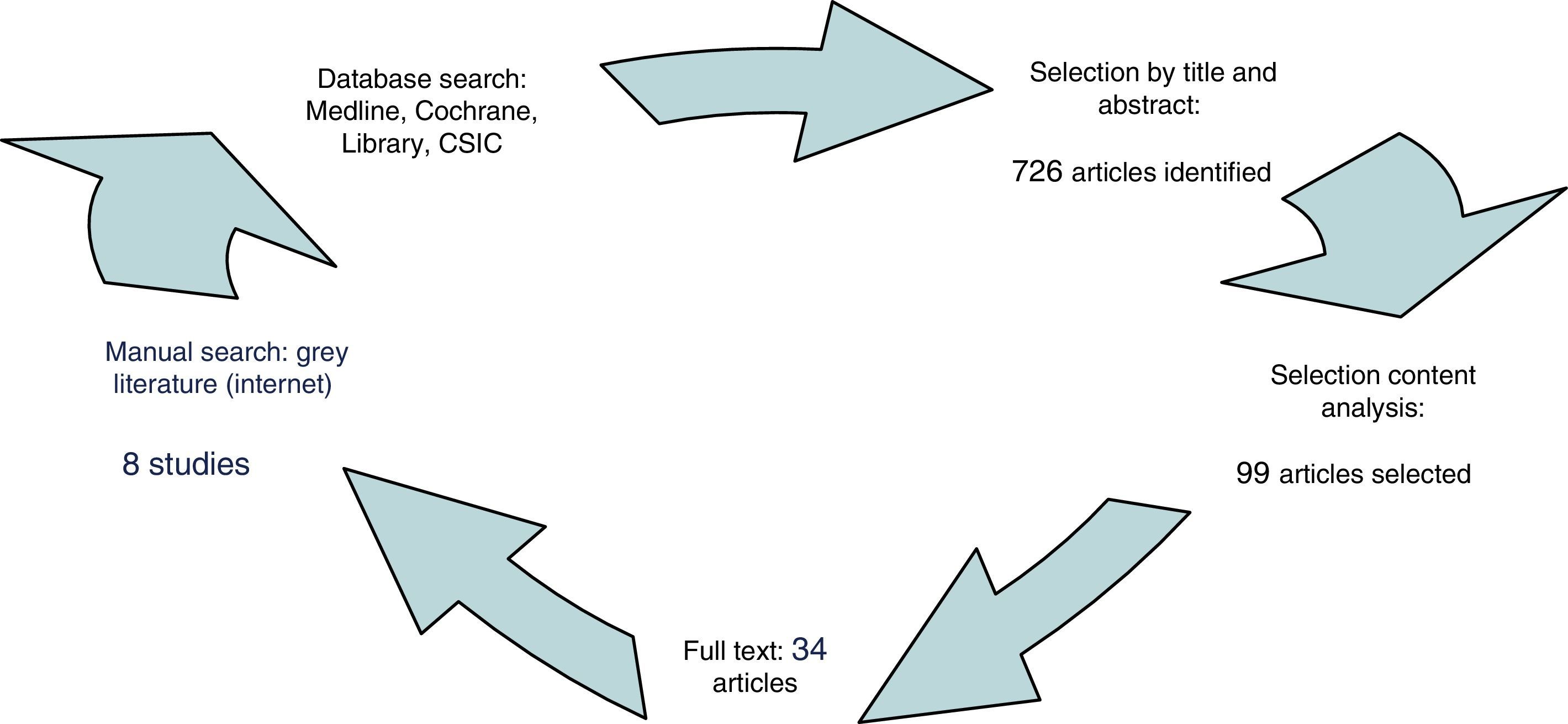
ResultsOf the 726 articles identified, 34 of most relevant (peer reviewed) were selected. It was noted that there is limited generalisable evidence on interventions that could be implemented in Primary Care or referral services available, although numerous studies suggest that improvements in the overweight are possible.
ConclusionsDespite the abundant literature and that many institutions place childhood obesity as one of the priorities of Public Health, we face the paradox that the evidence on cost-effectiveness of prevention interventions is sparse. Knowing these gaps in knowledge should lead to filling them with rigorous and well-designed studies.
El incremento en la prevalencia de obesidad y/o sobrepeso en todas las edades, la morbimortalidad asociada a dichas situaciones y la mayor percepción del problema en la sociedad han generado distintas hipótesis de respuesta científica y de la comunidad internacional.
ObjetivoInvestigar las intervenciones preventivas realizadas en obesidad infantil hasta el momento.
MétodosRevisión integradora de la literatura durante el periodo de estudio: abril de 2013 a noviembre dfe 2014. Se utilizó la base de datos internacional MEDLINE, a través de PubMed, The Cochrane Library (número 4 de 2002) y la base de datos nacional Isooc (CSIC) e internet. Se incluyeron en la revisión los trabajos de salud desarrollados entre 1990 y 2014, que se centraban o incluían intervenciones de educación, prevención, diagnóstico y tratamiento de la obesidad (en idiomas inglés y español).
ResultadosSe seleccionaron los 34 registros más relevantes (peer review) de 726 artículos identificados. Se constata que hay poca evidencia generalisable sobre intervención que pueda llevarse a cabo en atención primaria o en los servicios de referencia disponibles, aunque numerosos estudios indican que las mejoras en el sobrepeso son posibles.
ConclusionesA pesar de la abundante literatura y de que numerosas instituciones sitúan la obesidad infantil como una de las prioridades de salud pública, nos enfrentamos a la paradoja de que el coste-efectividad de las intervenciones preventivas es escaso. Constatar estas lagunas en el conocimiento debe llevar a completarlas con estudios rigurosos y bien diseñados.
Obesity is considered to be the disease of the 21st century due to the growing size of the problem over the past 20 to 30 years and the impact on morbidity and mortality rates, quality of life and healthcare expenditure.1,2 There is also concern for the medical, psychological and social problems it causes in Spain. According to the World Health Organisation (WHO), obesity is defined as a body mass index (BMI) ≥30; calculated by body mass (kg) divided by the square of the body height (metres).1,3–5 Obesity is characterised by an excessive accumulation of body fat or general hypertrophy of adipose tissue. The causes of obesity are multifactorial and include dysmorphic syndromes with genetic abnormalities, such as Bardet-Biedl, Laurence-Moon or Prader-Willi, and psychobiological, behavioural and cultural factors.6–8 However, the most common cause is exogenous. The psychological repercussions of social discrimination against obese children need to be highlighted, with many having serious self-esteem problems.1–3,6,9
The excessive and growing availability of high-calorie foods, the increase in saturated fats and refined sugars in the diet and the decrease in physical activity have all contributed to the dramatic rise in this problem.5,6 There is a tendency nowadays to consume high-calorie precooked dishes and/or eat unbalanced diets due to lack of time for cooking, and this has led to a shift from the Mediterranean diet to a fast-food one.3,10 There has also been an increase in sedentary behaviour among children, with preference for playing video games, surfing the Internet or watching television for over 3h a day and neglecting daily exercise.6,11–13
In industrialised countries, childhood obesity has increased alarmingly in recent years5,14,15 and has become a serious public health problem; it is a chronic disease of multifactorial origin that begins during childhood and adolescence. The prevalence among children in Spain is estimated to be around 12.7%. The increase in the prevalence of obesity and overweight, the associated morbidity and mortality, and the greater perception of the problem by society have led scientists and the international community to respond with different hypotheses.1,3,10
First of all, the publication of articles on the subject has increased notably in the past ten years. Second, many health science institutes have drawn up documents in recent years which, as part of public health plans and policies, are aimed at the general population and seek an integrative approach for different initiatives.10,11,16 Lastly, scientific interventions to evaluate their effectiveness have recently been published in a number of different journals.17 An analysis of these shows shortcomings, such as the fact that there are few quality studies, they are very heterogeneous in terms of design, target population and outcome, making it impossible to combine results with statistical methods,10,18,19 and they have other limitations such as poor power, small sample size, being limited to a certain socioeconomic level, lacking in cost analysis, etc.18,19
With this situation in mind, we decided it was imperative to carry out a review of the scientific literature on preventive interventions in childhood obesity.
Opening question: Is there enough evidence available on preventive interventions in childhood obesity? Objective: to investigate the preventive interventions in childhood obesity carried out to date worldwide.
MethodsThis is a narrative review, with a qualitative and descriptive approach, of national and international preventive interventions in childhood obesity. It is accepted that the general purpose of a literature review is to gather knowledge on a topic, helping to form the basis of an important study for nursing.20 Moreover, the integration mode is a method by which the researcher adds and abstracts conclusions by means of research to a particular subject for possible incorporation into practice. The PICO process was adopted following the successive steps taken to build the study: selection and definition of the population, literature search, categorisation of studies, evaluation of interventions included in the results, interpretation and comparison of these and presentation of the integrative review.21
During the study period (April 2013–November 2014) we used the National Library of Medicine (MEDLINE) databases, through PubMed, The Cochrane Library (Issue 4 of 2002), the Spanish Ciencias Sociales y Humanidades (ISOC – Social Sciences and Humanities) database (CSIC) and the Internet (Fig. 1). Aiming to minimise the lack of relevant documents retrieved, the search terms were: “obesity and childhood”; “preventive interventions and obesity and evidence”; “interventions and health care and childhood obesity”; “competences and nursing and childhood obesity”; “risk for overweight”; “psychosocial obesity”; “diet”; “physical activity”; “adverse life events”; “psychoeducation”; “prevention & public policy”. In order to choose these terms, we used the thesaurus of each of the consulted databases or the lists of controlled vocabulary if there was no thesaurus.
In order to perform an in-depth analysis, the process was organised into two stages:
- 1.
To broadly define the available work on child obesity through a detailed reading of the titles and abstracts of all the publications identified (peer reviewed). As an aid in this stage, we used an instrument composed of the data: title, authors, year and country of publication, journal and language. Of the 726 studies, we selected 99 articles according to these inclusion criteria.
- 2.
Analysis of content of a smaller number of publications, a total of 34, which constituted the body of the analysis.
We included in the review scientific health-related articles published between 1990 and 2014 focusing on or including interventions in education, prevention, diagnosis and treatment of obesity (in English and Spanish) for which the abstract and the full text were available with free online access (Fig. 1). We excluded studies that did not meet the above criteria: projects or interventions carried out outside the scope of health and theoretical studies. Also excluded were scientific journal editorials and duplicate articles.
In the end 34 records were imported into ProCite Personal Bibliographic Software and contact was made with Mental Health and Endocrinology specialists at the Reina Sofía University Hospital and with the Latin American and Brazilian Cochrane Center by post and e-mail.
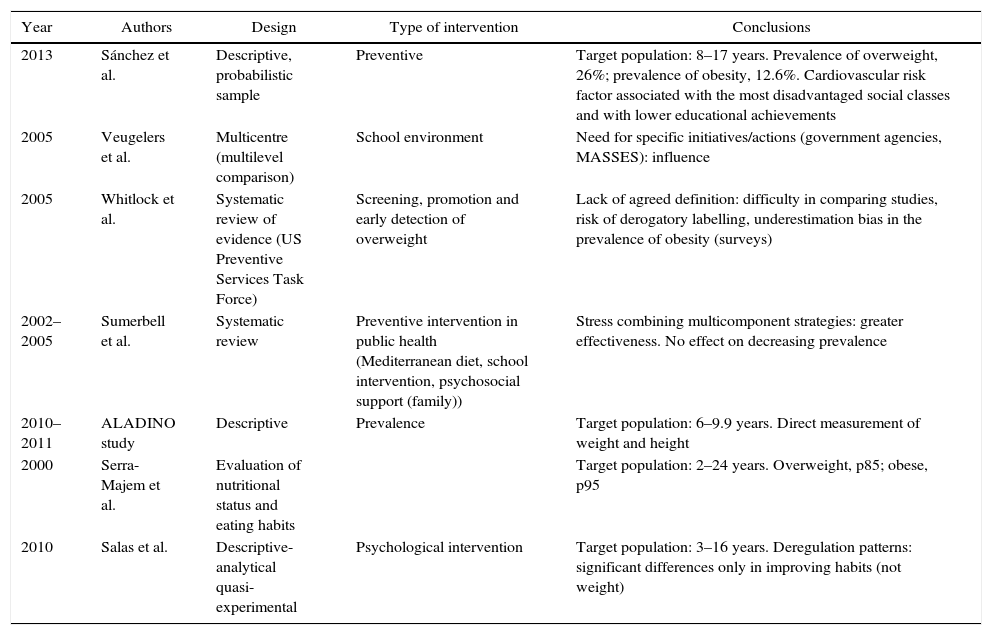
In order to ensure methodological rigour, the publications were summarised in a summary table with authors, year, purpose and focus and the most relevant conclusions (Table 1). For the analysis, the analysis of content, observation of the preanalytical stages, the design, findings, conclusions and interpretation of the data obtained were used as reference.
Most relevant results of the review.
| Year | Authors | Design | Type of intervention | Conclusions |
|---|---|---|---|---|
| 2013 | Sánchez et al. | Descriptive, probabilistic sample | Preventive | Target population: 8–17 years. Prevalence of overweight, 26%; prevalence of obesity, 12.6%. Cardiovascular risk factor associated with the most disadvantaged social classes and with lower educational achievements |
| 2005 | Veugelers et al. | Multicentre (multilevel comparison) | School environment | Need for specific initiatives/actions (government agencies, MASSES): influence |
| 2005 | Whitlock et al. | Systematic review of evidence (US Preventive Services Task Force) | Screening, promotion and early detection of overweight | Lack of agreed definition: difficulty in comparing studies, risk of derogatory labelling, underestimation bias in the prevalence of obesity (surveys) |
| 2002–2005 | Sumerbell et al. | Systematic review | Preventive intervention in public health (Mediterranean diet, school intervention, psychosocial support (family)) | Stress combining multicomponent strategies: greater effectiveness. No effect on decreasing prevalence |
| 2010–2011 | ALADINO study | Descriptive | Prevalence | Target population: 6–9.9 years. Direct measurement of weight and height |
| 2000 | Serra-Majem et al. | Evaluation of nutritional status and eating habits | Target population: 2–24 years. Overweight, p85; obese, p95 | |
| 2010 | Salas et al. | Descriptive-analytical quasi-experimental | Psychological intervention | Target population: 3–16 years. Deregulation patterns: significant differences only in improving habits (not weight) |
The 34 full texts were read in detail. Two thematic categories emerged: “existing preventive intervention in childhood obesity”; and “scientific evidence in preventive intervention”.
ResultsCharacterisationA total of 726 studies were published on the subject between 1990 and 2014. The year with the most publications was 2005 and the country with the most publications was the United States. Most of the studies were published in English. Only 15 publications were of Spanish or Latin-American origin, with the following journals standing out: Gaceta Sanitaria, Revista Chilena Scielo (2 articles), RevistaColombianadePsiquiatría and Atención Primaria (nursing); Medicina Clínica, Nutrición and Sanidad e Higiene Pública.
Existing preventive interventions in childhood obesityThe results of the latest Cochrane review available on preventive interventions in childhood obesity (importance of knowing the children's anthropometric data in order to have reference data and for comparison with other studies, and the psycho-environmental factors that promote excess weight in order to be able to act on them),9,14,19–22 indicate that the interventions evaluated to date have not succeeded in reducing the prevalence of obesity in clinical practice. They do, however, show improvements in society's knowledge of the problem.19,23 Some authors point out that the best results are obtained when several preventive strategies are combined and integrated, mainly those aimed at eliminating sedentary behaviour (e.g. stress reduction or reduction in time spent watching television and/or connected to the Internet) and increasing physical activity by various means.5,6
The predominant tendency in preventive strategies is to carry out multicomponent interventions taking school as the starting point and including the promotion of physical activity and nutritional education (they also tend to be complemented by actions directed at the families and the local environment), changes in the types of food offered by school canteens, and perhaps the involvement of other local resources (dietitians, medical professionals, psychologists), which often improves the results, although it increases the cost of the intervention.14,22,23
There are, however, many specific initiatives promoted by different agencies and institutions (sugary drinks, school lunches, walking routes to school), many of which have been evaluated in research studies.6,9,24
There seems to be wide debate about which psychological models should be used to inspire the interventions and about whether to give more emphasis to interventions with a psychosocial focus and/or the individual's own behaviour. In such cases, we have to remember that a lack of evidence does not mean there is “evidence of lack of effect of the intervention”.
The International Obesity Task Force (IOTF), in collaboration with the WHO, summarises this reflection well and adopts a health-promoting perspective when it considers that, in order to halt the obesity epidemic, interventions directed at the family or school must be accompanied by professional changes in the psychosocial and cultural context, so that any benefits which are achieved can be maintained and improved over time.1,15,25
With that in mind, the Cochrane Collaboration analysis recommends that the following aspects be given priority in the design of new public health interventions19:
- •
Environments that support and facilitate behavioural changes (psychotherapy).
- •
Improvement in the types of food offered in schools (safe play areas to increase physical activity).
- •
Provision of psychosocial support to families (modify their current life and working circumstances).
- •
The need to conduct long-term follow-up studies that include relevant results and cost-effectiveness assessments.
In 2005 the US Task Force on Preventive Services published a systematic review on intervention for the early detection of overweight in children in clinical practice. The report chooses to use the term overweight instead of obese, as BMI is a relative measure of body weight (with limitations for specifying obesity in childhood) and may lead to children being unfairly labelled.18,33
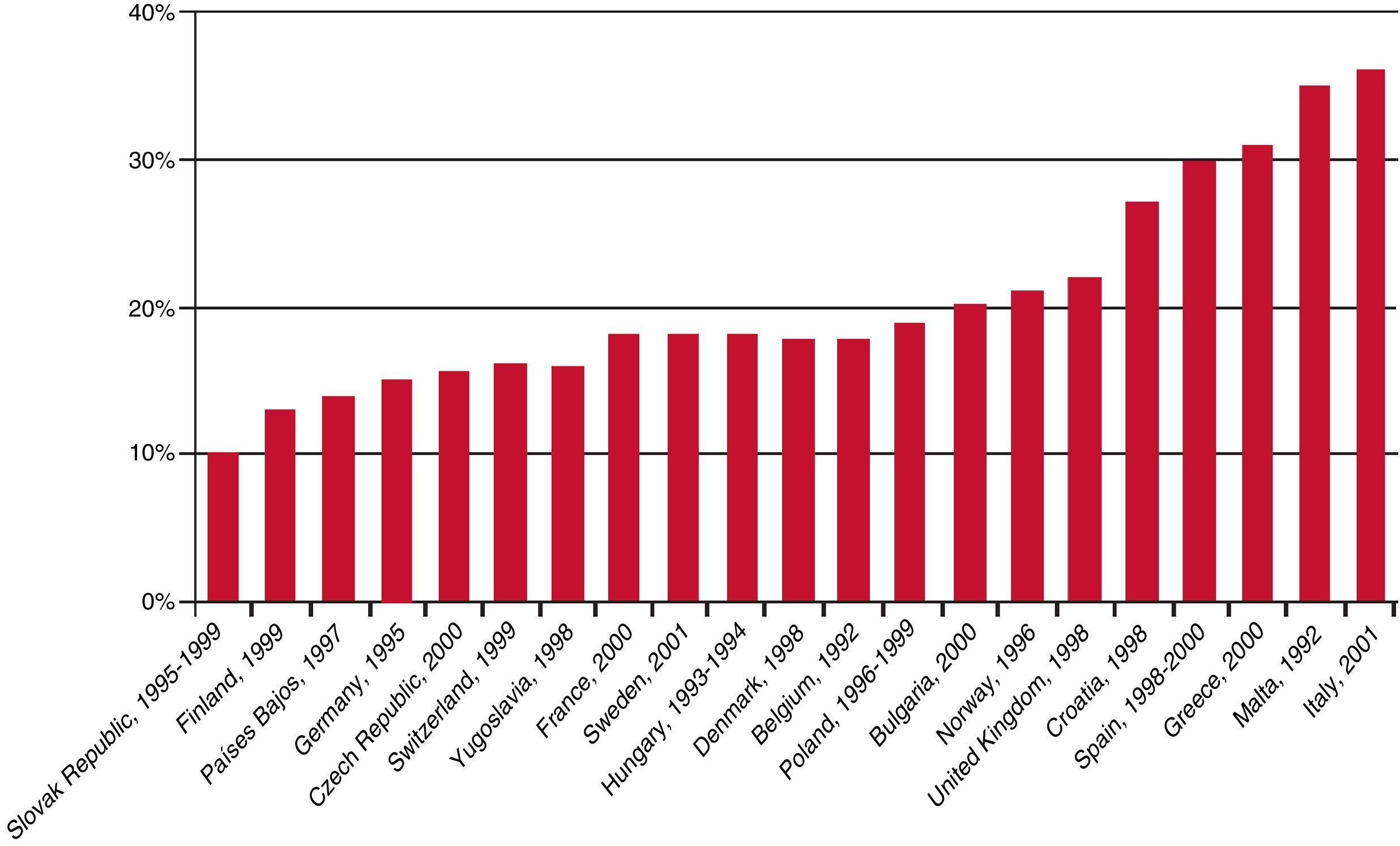
The result is that in the definition of childhood obesity, there are no consensus criteria for determining overweight or obesity based on BMI. The two most widely accepted sets of criteria are those proposed by the WHO28 (overweight: gender- and age-specific BMI values >1 standard deviation in the reference population set out in the cited article; obesity: gender- and age-specific BMI values and >2 standard deviations) and those proposed by the IOTF29 (with specific cut-off points for establishing childhood overweight or obesity for each value and gender according to the reference population detailed in the cited article). In Spain, there is also widespread use of the tables published by the F. Orbegozo Foundation,31 used in the “enKid” study, a study conducted across Spain on childhood obesity, dietary habits, and lifestyles of children and adolescents which evaluates their eating habits and nutritional status and, as cut-off points, considers values of the 85th percentile for overweight and the 95th percentile for obesity, in both cases specific for age and gender (Fig. 2).
Apart from the lack of an agreed definition of obesity that makes it difficult to compare studies, there is also the fact that the available data often come from studies, mainly health surveys, in which weight and height are not measured directly, but rather are based on estimates reported by participants or their guardians, with the consequent bias that tends to underestimate the prevalence of obesity.34 In Spain, the last two studies conducted on a national level which used a direct measurement of weight and height were the “enKid” study, carried out from 1998 to 2000 with a population aged from 2 to 24 years, and the more recent ALADINO study (study monitoring growth, diet, physical activity, child development and obesity),12 the fieldwork for which took place from October 2010 to May 2011 and was limited to the population of male and female children from the age of 6–9.9 years.
However, in the Task Force analysis, BMI is the preferred measurement for assessing overweight and correlates well with other measures of adiposity in childhood and adolescence. Based on these criteria, it is estimated that 10% of children aged 2–5 years and 16% of children over 6 years of age are overweight, with a significantly high prevalence in racial and ethnic minorities in the age subgroups over the age of 6 years.10
Most of the studies address intensive behavioural interventions performed by specialists in children aged 8–12 years, and in many cases using family-based treatments.10
We did not identify any trials designed to evaluate early detection and treatment programmes and, in general, research on the effectiveness of interventions appears to be lacking. There is low-quality evidence on the use of drugs as adjuncts to behavioural therapy in adolescence and evidence of even worse quality on bariatric surgery.5,11,18,24
DiscussionThe results of this review and its recommendations coincide with another review conducted by the US Task Force on Community Preventive Services,11,17 which addresses public health strategies for obesity prevention in schools. This review also concludes that the evidence is insufficient to determine the effectiveness of interventions that combine nutrition, psychotherapy and physical activity, to prevent or reduce obesity in the school setting. This is mainly due to the small number of studies carried out with scientific rigour and the choice of non-comparable results.34,35
It is considered important to monitor child growth and development by periodically determining BMI in clinics, although care should be taken not to label children as overweight unnecessarily until we obtain a better understanding of the long-term risk and consequences. An interesting point is that most studies do not report the adverse effects and harm caused by these interventions and the effects of derogatory labelling (social discrimination, bingeing, low self-esteem, eating disorders, domestic violence).24,33,35
With regard to BMI, the use of waist circumference measurements as indicator of abdominal fat distribution is now being evaluated, due to its greater reliability when attributing health risks (mainly cardiovascular) in adulthood. This, however, has not been sufficiently demonstrated in the paediatric age groups.4,10,27,36
There is limited generalisable evidence on interventions that could be implemented in primary care or the available referral services, although numerous studies suggest that improvements in the overweight problem are possible. Examples are the clinical guidelines and recommendations on lifestyle changes that can be applied to all children and adolescents regardless of risk.31,37
Similarly, in spite of the large amount of literature and the fact that many institutes class childhood obesity as a major priority in public health, the paradox is that evidence of the cost-effectiveness of these interventions is lacking in Spain. The prevalence of childhood obesity in Spain is among the highest in Europe, along with Malta, Italy, the United Kingdom and Greece. The 2010 Sociedad Española de Salud Pública y Administración Sanitaria (SESPAS – Spanish Society of Public Health and Health Administration) report stated that 35% of children were affected by excess weight (20% overweight and 15% obese). We are therefore faced with a major and ever-increasing risk factor, and must recognise the need for systematic and rigorous monitoring of this trend. There are frequent methodological weaknesses in the definition and measurement of obesity, and in sample selection. In the current literature, in contrast to the many that can be found dealing with adults, there are few studies that measure the economic impact of childhood obesity.35 This is an important issue, especially when we consider other indirect costs such as school/work absenteeism, or intangible costs, such as those related to the psychological and social repercussions of the problem and the implications obesity has on the quality of life of the people affected, all of which need to be evaluated.38
However, the lack of sufficiently powerful evidence should not prevent us from dedicating time and energy to clinical interventions on healthy habits and the screening and detection of childhood obesity while further research continues, especially in the development of new tools to facilitate work in clinic practice (risk-detection algorithms, psychotherapy for relatives and patients to facilitate behavioural changes, etc.).24,34,35,38
To conclude, the psychological perspective should always be taken into account, but whether the primary care physician or specialist does so will depend, in the majority of cases, on the effectiveness of the intervention.
LimitationsWe have to acknowledge the inherent publication bias, which we have tried to minimise by expanding with reference and intuitive searching in Google Scholar (grey literature) and limiting the studies analysed to those written in English and Spanish.
ConclusionsSome promising studies are being published on behavioural interventions in these age groups (although no clear benefits have yet been demonstrated). The prevention of childhood obesity requires the collaboration and commitment of many different social sectors, with the development of innovative methodologies being necessary, both in the design of interventions and their evaluation.
Traditionally, the treatment of obesity is based on diet and physical exercise. However, this approach is far too reductionist, as the psychological and social/family aspects, which play a decisive role in the generation and maintenance of obesity, are not usually taken into consideration in the treatment.
For the moment, periodic determination of BMI seems to be the best instrument for detecting obesity and overweight, but in childhood and adolescence, we must avoid labelling the patients. Since the results of various preventive approaches in childhood obesity are rather limited, greater efforts and resources should be applied to the task of preventing obesity from very early ages.
A final thought: recognising these gaps in knowledge should encourage us to fill them through rigorous, well-designed studies.
Conflict of interestNone.
To all the members of the team who collaborated on this project and, in particular, the team of professionals that makes advances in our nursing profession possible by disseminating our knowledge. Our heartfelt thanks go out to you.
Please cite this article as: Alba-Martín R. Evidencia científica sobre intervenciones preventivas en obesidad infantil. Rev Colomb Psiquiat. 2017;46:36–43.