The objective was to evaluate the association between sleep quality and mental health in students at a jungle university in Peru.
Materials and methodsAn analytical cross-sectional study was conducted on university students ≥18 years old during September and November 2020. Mental health status was measured with General Health Questionnaire (GHQ-12), and sleep quality with the Pittsburgh Sleep Quality Index (PSQI). The association was assessed using linear regression models, and crude (βc) and adjusted (βa) beta regression coefficients with their respective 95% confidence intervals (95%CI) were estimated.
ResultsTwo hundred and seventy-nine students were evaluated, 35.1% were 20–21 years old and 56.6% were male. The mean PSQI was 7.9±3.2, and 75.3% presented sleep problems. The mean GHQ-12 was 14.0±6.6, and 57.7% showed suspected psychopathology. The total sleep quality score (βa=0.36; 95% CI: 0.11–0.61; p=0.005), as well as, higher component scores, subjective sleep quality (βa=1.57; 95% CI: 0.28–2.87; p=0.018), sleep duration (βa=1.25; 95% CI: 0.35–2.16; p=0.007), hypnotic medication use (βa=1.79; 95% CI: 0.43–3.15; p=0.010), and daytime dysfunction (βa=1.15; 95% CI: 0.10–2.19; p=0.032), were associated with worse mental health status score.
ConclusionAfter 6 months of initiation of COVID-19 confinement, the frequency of sleep disturbance and mental health were elevated. Sleep quality disturbance was associated with worse mental health status.
Evaluar la asociación entre la calidad del sueño y la salud mental en estudiantes de una universidad de la selva de Perú.
Materiales y métodosSe realizó un estudio transversal analítico en universitarios ≥18 años durante septiembre y noviembre de 2020. El estado de la salud mental fue medido con General Health Questionnaire(GHQ-12) y la calidad del sueño con el Pittsburgh Sleep Quality Index (PSQI). Se evaluó la asociación mediante modelos de regresión lineal y se estimaron los coeficientes de regresión beta crudo (βc) y ajustado (βa) con sus respectivos intervalos de confianza (IC) a 95%.
ResultadosSe evaluaron 279 estudiantes, 35,1% tenían 20-21 años y 56,6% eran varones. La media del PSQI fue de 7,9±3,2, y 75,3% presentaron problemas de sueño. La media del GHQ-12 fue de 14,0±6,6, y 57,7% mostraron sospecha de psicopatología. El puntaje total de la calidad de sueño (βa=0,36; IC 95%: 0,11-0,61; p=0,005), así como, un mayor puntaje de los componentes. la calidad subjetiva del sueño (βa=1,57; IC 95%: 0,28-2,87; p=0,018), duración del sueño (βa=1,25; IC 95%: 0,35-2,16; p=0,007), uso de medicación hipnótica (βa=1,79; IC 95%: 0,43-3,15; p=0,010), y disfunción diurna (βa=1,15; IC 95%: 0,10-2,19; p=0,032), se asociaron a un peor puntaje del estado de salud mental.
ConclusiónTras seis meses de iniciado el confinamiento por COVID-19, la frecuencia de trastornos del sueño y salud mental fueron elevados. La alteración de la calidad del sueño se asoció a un peor estado de salud mental.
Problems related to sleep quality are considered a worldwide public health epidemic.1 These disorders have been linked to seven of the 15 leading causes of death in the United States,1 and have been shown to increase the incidence of stroke, dyslipidemia, obesity, and diabetes, as well as increased all-cause, coronary heart disease and stroke mortality.2,3 In addition, poor sleep quality has been linked to the development of mental disorders such as depression and anxiety.4,5
During 2020, the governments of the world, to control the COVID-19 pandemic and based on the recommendations given by the World Health Organization (WHO),6 imposed strategies that limited physical distancing. Thus, they imposed mandatory confinement that lasted for months, with the impossibility of attending classes, working, or socializing in person.7,8 Consequently, lifestyles such as negative eating patterns, sleep disorders, and increased use of screens have been favored.9,10 In addition, a higher incidence of mental disorders such as symptoms of depression, anxiety, and stress has been recorded during the pandemic.11–13
On the other hand, an increased incidence of sleep quality disorders during the pandemic has been reported, with an estimated prevalence globally of 31% among healthcare professionals, 18% among the general population, and 57% among patients with COVID-19.14 However, in university students, poor sleep quality and mental disorders (mainly anxiety) have been common problems since long before the pandemic, due to circadian rhythms altered by study hours and academic responsibilities.15 Therefore, due to the effects of confinement, the university population could have developed a higher frequency of such problems.16
In Peru, mandatory confinement was established starting in March and remained mandatory until the end of October 2020, with about 6 months of strict measures.16 Previous studies in Peru have evaluated an increase in the incidence of mental disorders and sleep quality, but have not assessed the association between these conditions in university students. Therefore, the present study evaluated the relationship between sleep quality and mental health status in a representative sample of students from a university in the Peruvian jungle, 6 months after the start of the outbreak and during the first peak of COVID-19 deaths.
Materials and methodsStudy design and populationAn analytical cross-sectional study was carried out. The population consisted of undergraduate university students enrolled at the National University of the Peruvian Amazon, Iquitos, Peru. We excluded those who did not wish to participate in the survey, minors, those who did not have a means of communication by which to contact them during the study period, and those surveys with inconsistent responses. Finally, records with incomplete data were eliminated.
Sample and samplingSimple random probability sampling was used based on the list of university students enrolled in the first semester of 2020. The sample calculation was considered for hypothesis testing studies using the correlation coefficient. The value of Pearson's correlation coefficient was obtained from the study of Tao et al.17 The correlation coefficient between mental health status and sleep quality was 0.259. In addition, we considered a confidence level of 99% and a power of 90% to ensure that the correlation was not due to systematic error. The data were entered into the Epidat statistical software, considering, in addition, a non-response or incomplete response rate of 30%, thus obtaining a final sample of 279 university students.
ProceduresThe university provided the telephone numbers and names of the students enrolled in the study period after the ethical approval of the project. From this, the survey was distributed to the selected students, through the “WhatsApp” application with a standardized message that was reiterated up to two times and contained the link to fill out the virtual survey (using Google Forms). The survey was available from September 1 to November 29, 2020.
QuestionnaireThe survey began with the presentation of the research, the request for informed consent, and the instructions for completion. Subsequently, after approval of the informed consent, the self-administered questionnaire was presented, which was designed taking into account previous studies.18,19
The questionnaire consisted of three sections (see Supplementary Material 1). The first section was composed of sociodemographic and personal variables. The second section assessed sleep quality. The third section assessed the presence of minor mental disorders.
The substantive and content validity was confirmed by a panel of physicians specialized in epidemiology and psychiatry. In addition, Cronbach's Alpha was calculated after the application of the questionnaire. The result was a good Alpha for the global survey (alpha=0.70).
Dependent variableThe dependent variable was the presence of minor mental disorders, estimated employing the General Health Questionnaire (GHQ-12),18 which has been validated in Spanish for use in students, with a Cronbach's alpha of 0.78.19 The questionnaire consists of 12 items, 6 positive and 6 negative. The items are answered on a four-point Likert-type scale (0-1-2-3). The total score was calculated by adding the scores obtained in all the statements of the scale. The rating ranges were from 0 to 36 and that categorically a score ≤12 was categorized as “with suspected psychopathology” or “with psychological well-being” and >12 as “With suspected psychopathology”, such as depression or anxiety.
Independent variableThe independent variable was sleep quality, which was measured using the Pittsburgh Sleep Quality Index adapted to Spanish from the “Pittsburgh Sleep Quality Index” (PSQI).20 This version was validated in Colombia and has a Cronbach's alpha of 0.78.21 The instrument consisted of 24 questions that provide an overall score of sleep quality and partial scores (from 0 to 3) distributed in seven components: (A) subjective sleep quality, (B) subjective sleep latency, (C) sleep duration, (D) subjective habitual sleep efficiency, (E) sleep disturbances, (F) The use of medication for sleep, and (G) Daytime dysfunction.
Finally, the PSQI total score could assume scores between 0 and 21. Categorically a score of less than five is considered as “no sleep problems”, a score between five and seven as “deserves medical attention” and if it was higher than eight as “deserves medical attention and medical treatment”. The specific questions of the PSQI, for each component, the methodology used, and the interpretation of the scores for each component can be found in Supplementary Material 2, according to the original PSQI questionnaire.21
Other variablesFor the present research, we included sociodemographic and personal characteristics, such as gender (male, female), age terciles (18–19, 20–21, and over 21 years), year of study (first year, second year, third year, fourth year and last year [fifth, sixth and seventh year for Human Medicine; fifth and sixth for Law and Dentistry; and the fifth year for the rest of the careers]), professional school (engineering, health sciences, social sciences, and economics-business), marital status (with a partner or without a partner), history of COVID-19 (no, yes), history of a family member in the household with COVID-19 (no, yes), weight alterations during quarantine (none, weight loss and weight gain).
Statistical analysisStata® v.17.0 software (Stata Corporation, College Station, TX, USA) was used. The quantiles plot and the Shapiro–Wilk test were used to evaluate the normality of the numerical variables of interest. Thus, means were presented with their respective standard deviations (SD) or medians plus interquartile range (IQR). For categorical variables, absolute and relative frequencies were used. To evaluate the differences between the variables of interest with the categorical variables, the Student test for equal variances (evaluated by the test of equality of SD), the ANOVA test, or the Kruskall–Walis test according to normality was used.
The association between general mental health status and sleep quality (as well as its components) was evaluated by simple and multiple linear regression models, obtaining the crude (βc) and adjusted (βa) beta regression coefficient with their respective 95% confidence intervals (CI 95%), after evaluation and compliance with assumptions of normal distribution, independence, and homoscedasticity, For the adjusted regression, an epidemiological approach was considered, entering the following confounding variables into the model: sex, age, semester of study, professional school, marital status, whether she had been diagnosed with COVID-19, whether her family had had COVID-19 and whether she had suffered weight alterations during quarantine. No collinearity was found among the variables in this model (variance inflation factor less than 10).
Ethical issuesAll procedures in the present study followed international ethical standards, maintaining anonymity and confidentiality. The research protocol was approved by the ethics committee of the Universidad San Martín de Porres (Oficio N°: 332-2020-CIEI-FMH-USMP), and registered in the Health Research Project Registration Platform of Peru (ID: F4D28160-2EC0-4309-8AE5-3E140407070E06).
ResultsThe survey was distributed among 369 students from the different professional schools of the study university. Of these, 20 minors were excluded, as well as 24 individuals who recorded incomplete information and 46 who presented incongruent information in the sleep quality questions. This left us with a final sample size of 279 university students.
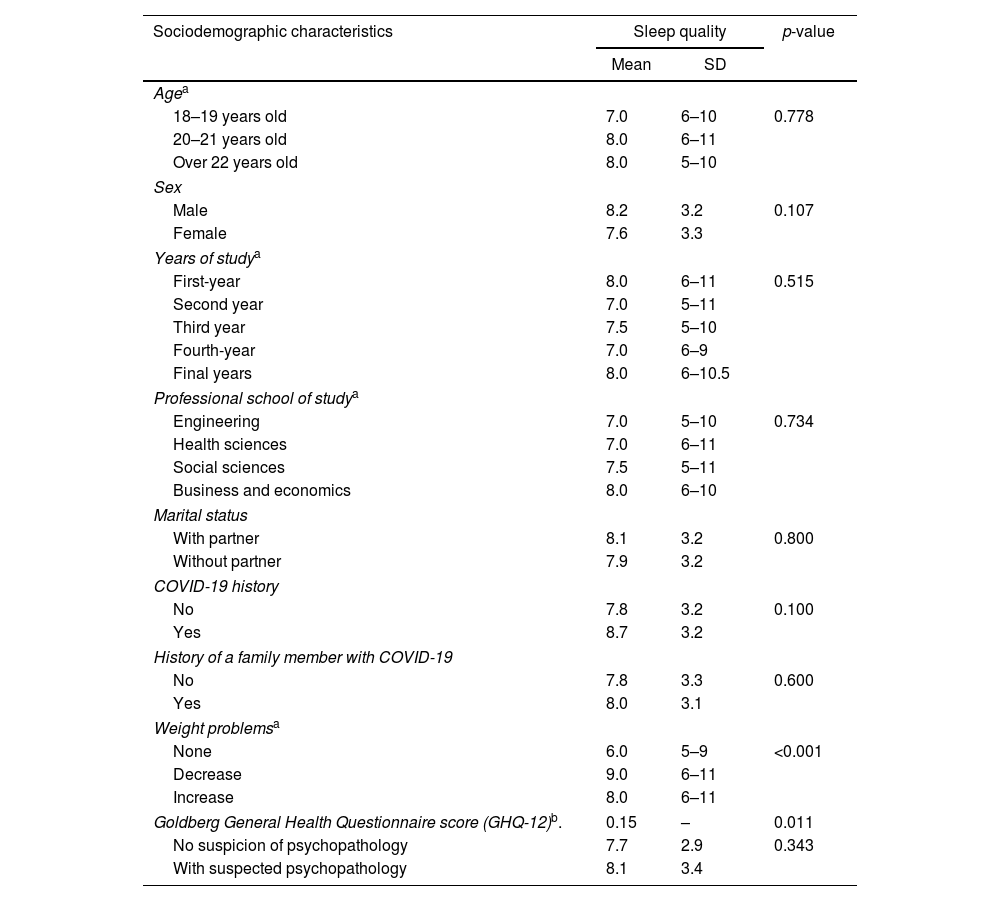
Most of the respondents were male (56.6%), in the 20–21 years age group (35.1%), those in the last years of their degree (28.7%), and engineering professionals (30.8%). Regarding the evaluation of sleep quality, the mean of the respondents was 7.9±3.2, categorizing 75.3% of the respondents as having sleep problems (PSQI score>5). While the mean mental health questionnaire score was 14.0±6.6, with 57.7% having suspicion of psychopathology (GHQ-12 score>12) (Table 1).
Pittsburgh Sleep Quality Index score (PSQI) according to general characteristics of participants (n=279).
| Sociodemographic characteristics | Sleep quality | p-value | |
|---|---|---|---|
| Mean | SD | ||
| Agea | |||
| 18–19 years old | 7.0 | 6–10 | 0.778 |
| 20–21 years old | 8.0 | 6–11 | |
| Over 22 years old | 8.0 | 5–10 | |
| Sex | |||
| Male | 8.2 | 3.2 | 0.107 |
| Female | 7.6 | 3.3 | |
| Years of studya | |||
| First-year | 8.0 | 6–11 | 0.515 |
| Second year | 7.0 | 5–11 | |
| Third year | 7.5 | 5–10 | |
| Fourth-year | 7.0 | 6–9 | |
| Final years | 8.0 | 6–10.5 | |
| Professional school of studya | |||
| Engineering | 7.0 | 5–10 | 0.734 |
| Health sciences | 7.0 | 6–11 | |
| Social sciences | 7.5 | 5–11 | |
| Business and economics | 8.0 | 6–10 | |
| Marital status | |||
| With partner | 8.1 | 3.2 | 0.800 |
| Without partner | 7.9 | 3.2 | |
| COVID-19 history | |||
| No | 7.8 | 3.2 | 0.100 |
| Yes | 8.7 | 3.2 | |
| History of a family member with COVID-19 | |||
| No | 7.8 | 3.3 | 0.600 |
| Yes | 8.0 | 3.1 | |
| Weight problemsa | |||
| None | 6.0 | 5–9 | <0.001 |
| Decrease | 9.0 | 6–11 | |
| Increase | 8.0 | 6–11 | |
| Goldberg General Health Questionnaire score (GHQ-12)b. | 0.15 | – | 0.011 |
| No suspicion of psychopathology | 7.7 | 2.9 | 0.343 |
| With suspected psychopathology | 8.1 | 3.4 | |
SD: standard deviation.
Among the respondents, higher Pittsburgh Sleep Quality Index scores were presented by respondents aged 20–21 years (8, RIQ=6–11), those older than 22 years (8, RIQ=5–10), those of male gender (8.2±3.2), those in their first (8, RIQ=6–11) and last year (8, RIQ=6–10.5), those studying economics and business (8, RIQ=6–10), those with a personal history of COVID-19 (8.7±3.2), family history of COVID-19 (8.0±3.1), those with weight loss during confinement (9, RIQ=6–11) and those with suspected psychopathology (8.1±3.4) (Table 2).
Goldberg General Health Questionnaire scores (GHQ-12) according to the general characteristics of the participants (n=279).
| Sociodemographic characteristics | General mental health status | ||
|---|---|---|---|
| Mean | SD | p-value | |
| Agea | |||
| 18–19 years old | 13.0 | 10–18 | 0.638 |
| 20–21 years old | 13.0 | 10–18 | |
| Over 22 years old | 15.0 | 9–20 | |
| Sex | |||
| Male | 14.8 | 6.7 | 0.027 |
| Female | 13.0 | 6.3 | |
| Years of studya | |||
| First-year | 13.0 | 10–18 | 0.806 |
| Second year | 13.0 | 10–18 | |
| Third year | 13.0 | 9–17.5 | |
| Fourth-year | 15.0 | 10–20 | |
| Final years | 13.5 | 11–17 | |
| Professional school of studya | |||
| Engineering | 13.0 | 10–18 | 0.387 |
| Health sciences | 14.0 | 11–18 | |
| Social sciences | 13.0 | 8–18 | |
| Business and economics | 13.0 | 10–17 | |
| Marital status | |||
| With partner | 13.9 | 5.7 | 0.937 |
| Without partner | 14.0 | 6.7 | |
| COVID-19 history | |||
| No | 14.2 | 6.8 | 0.244 |
| Yes | 12.9 | 5.5 | |
| History of the family member with COVID-19 | |||
| No | 14.2 | 6.9 | 0.473 |
| Yes | 13.7 | 6.0 | |
| Weight problemsa | |||
| None | 15.0 | 10–18 | 0.644 |
| Decrease | 13.0 | 9–19 | |
| Increase | 13.0 | 10–17 | |
| Pittsburgh Sleep Quality Index (PSQI)b | 0.15 | – | 0.011 |
| No problems | 13.7 | 6.4 | 0.031 |
| With sleep problems warranting medical attention | 12.5 | 4.8 | |
| With sleep problems warranting medical attention and treatment | 15.0 | 7.3 | |
SD: standard deviation.
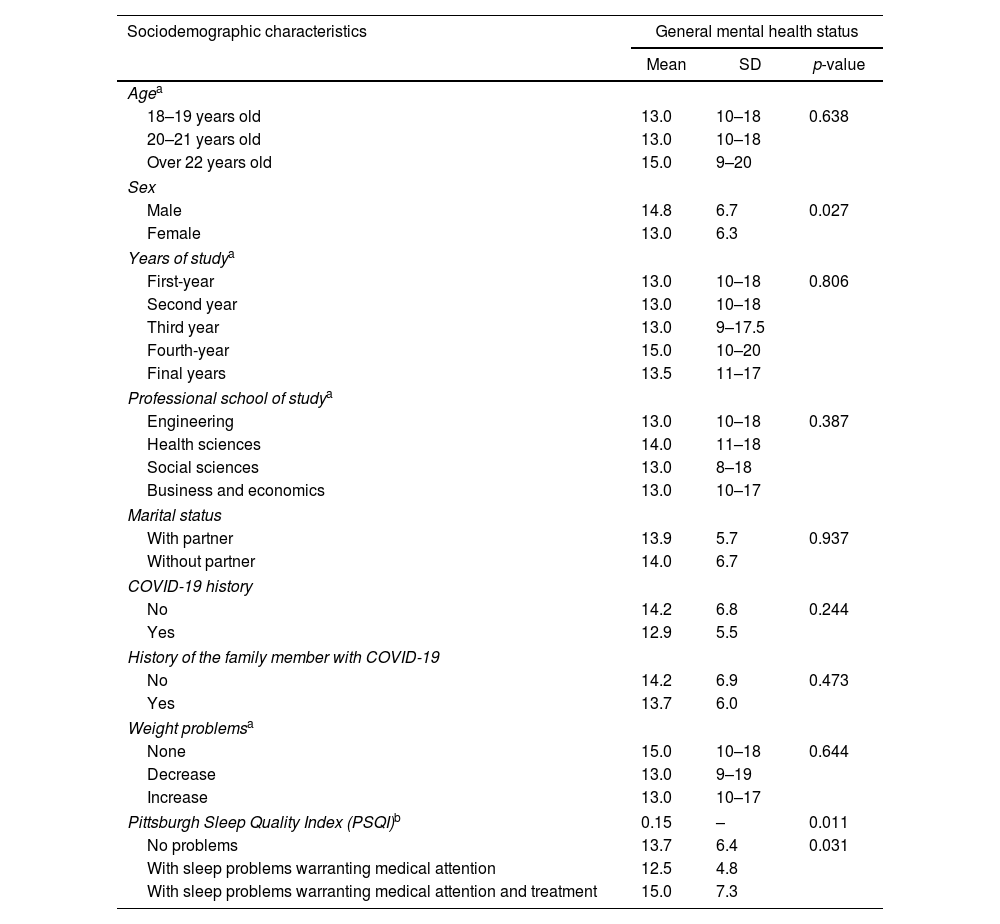
On the other hand, those who were older than 22 years (15, RIQ=9–20), males (14.8±6.7), those who were in their fourth year of study (15, RIQ=10–20), those who were studying health sciences (14, RIQ=11–18), those who were without a partner (14.0±6.7), those with no personal history (14.2±6.8), no family history of COVID-19 (14.2±6.9), those with no weight problems during COVID-19 confinement (15, RIQ=10–18), and those with sleep problems warranting medical attention and treatment (PSQI>8; 15.0±7.3) (Table 3).
Linear regression model to assess the association between general mental health status and sleep quality.
| Sleep quality | General mental health status | |||||
|---|---|---|---|---|---|---|
| Simple regression | Multiple regression* | |||||
| βc | 95% CI | p-value | βa | 95% CI | p-value | |
| Component 1: subjective sleep quality | 1.37 | 0.12–2.62 | 0.032 | 1.57 | 0.28–2.87 | 0.018 |
| Component 2: sleep latency | −0.42 | −1.32 to 0.49 | 0.367 | −0.38 | −1.32 to 0.55 | 0.419 |
| Component 3: sleep duration | 1.07 | 0.19–1.95 | 0.018 | 1.25 | 0.35–2.16 | 0.007 |
| Component 4: habitual sleep efficiency | 0.53 | −0.13 to 1.18 | 0.112 | 0.52 | −0.16 to 1.20 | 0.134 |
| Component 5: sleep disturbances | 0.78 | −0.41 to 1.97 | 0.198 | 0.75 | −0.48 to 1.97 | 0.230 |
| Component 6: use of sleep medication | 1.7 | 0.38–3.01 | 0.011 | 1.79 | 0.43–3.15 | 0.010 |
| Component 7: daytime dysfunction | 0.86 | −0.13 to 1.84 | 0.088 | 1.15 | 0.10–2.19 | 0.032 |
| Pittsburgh Sleep Quality Index Global Score (PSQI) | 0.31 | 0.07–0.55 | 0.011 | 0.36 | 0.11–0.61 | 0.005 |
βc: crude beta regression coefficient; βa: adjusted beta regression coefficient; 95% CI: 95% confidence interval. p values less than 0.05 are in bold.
The multiple linear regression model was calculated considering an epidemiological model. Each component and the total PSQI score were adjusted for sex, age, semester of study, professional school, marital status, whether she had been diagnosed with COVID-19, whether her family had had COVID-19 and whether she had suffered weight alterations during quarantine.
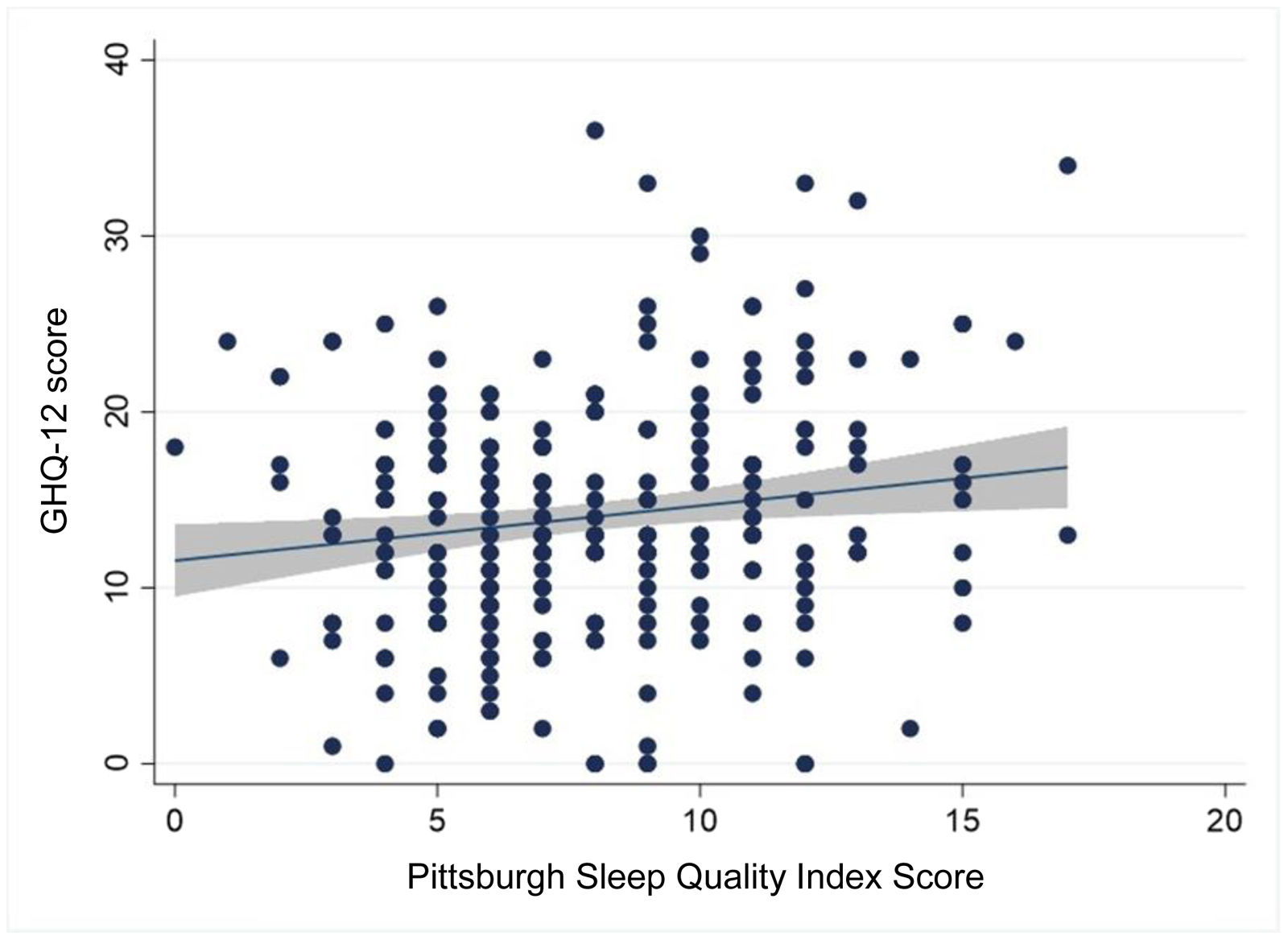
Pearson's correlation between the Pittsburgh sleep quality index and the Goldberg general health questionnaire score showed a positive association (Pearson's correlation coefficient=0.15; p=0.011) (Fig. 1, Tables 2 and 3).
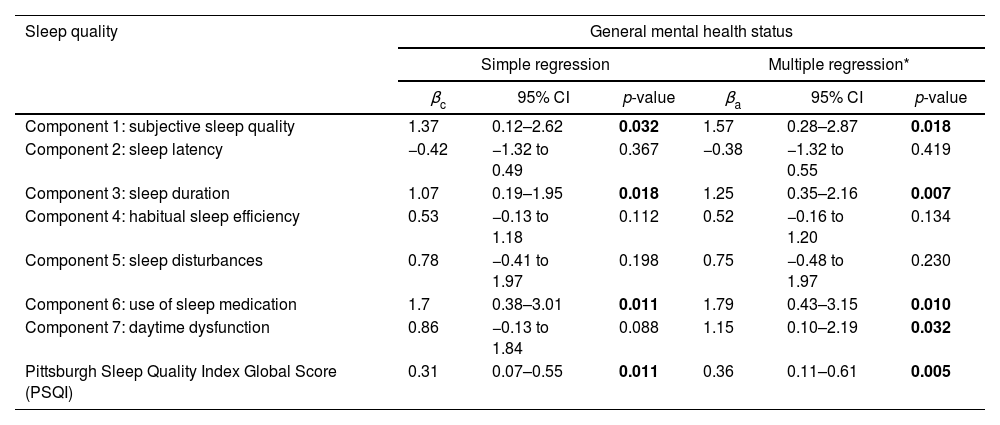
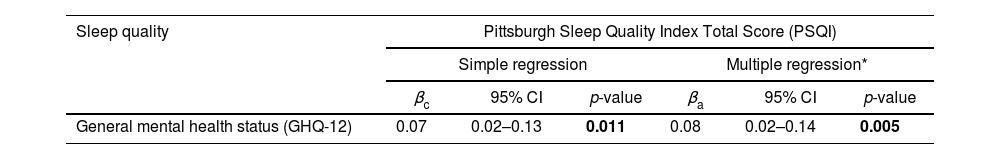
Likewise, in the simple (βc=0.31; 95% CI: 0.07–0.55; p=0.011) and multiple linear regression analysis (βa=0.36; 95% CI: 0.11–0.61; p=0.005), the association between the scores of both variables continued with a positive association. Finally, within the PSQI domains, higher scores on subjective sleep quality (βa=1.57; 95% CI: 0.28–2.87; p=0.018), sleep duration (βa=1.25; 95% CI: 0.35–2.16; p=0. 007), hypnotic medication use (βa=1.79; 95% CI: 0.43–3.15; p=0.010), and daytime dysfunction (βa=1.15; 95% CI: 0.10–2.19; p=0.032), were associated with worse mental health status (Table 4).
Linear regression model to assess the association between sleep quality and general mental health status.
| Sleep quality | Pittsburgh Sleep Quality Index Total Score (PSQI) | |||||
|---|---|---|---|---|---|---|
| Simple regression | Multiple regression* | |||||
| βc | 95% CI | p-value | βa | 95% CI | p-value | |
| General mental health status (GHQ-12) | 0.07 | 0.02–0.13 | 0.011 | 0.08 | 0.02–0.14 | 0.005 |
βc: crude beta regression coefficient; βa: adjusted beta regression coefficient; 95% CI: 95% confidence interval. p values less than 0.05 are in bold.
The multiple linear regression model was calculated considering an epidemiological model. Each component and the total PSQI score were adjusted for sex, age, semester of study, professional school, marital status, whether she had been diagnosed with COVID-19, whether her family had had COVID-19 and whether she had suffered weight alterations during quarantine.
It was found that about 75.3% of the respondents presented some sleep problems and 57.7% presented suspected psychopathology. In addition, poor sleep quality was significantly correlated with mental health. Also, within the PSQI domains, subjective sleep quality, sleep duration, use of hypnotic medication, and daytime dysfunction were associated with poorer mental health. These findings provide evidence of the impact of the COVID-19 pandemic on these disorders in university students in the Peruvian jungle.
Frequency of suspected psychopathologyApproximately half of the students presented suspicion of psychopathology. Similar frequencies (between 62.3% and 71.5%) have been reported in university students in India, Turkey, the United Kingdom, and the United States.22–25 It should be recognized that the pandemic has had a greater impact on the mental health of university students than on the general population.25 Consequently, a higher frequency of university students with suicidal thoughts has been reported.25 Because of this, the implementation of virtual mental health surveillance centers in universities could be important to reduce negative impacts, especially during health emergencies.
Frequency of sleeping problemsAbout three-quarters of the respondents had sleep disorders, with figures similar to those reported in 79.3% of university students in Egypt and three-quarters of university students in Italy during confinement,26,27 but higher than those reported in university students in Macao-China (45.1%).17 This could be due to the effects that the pandemic had on people, such as mandatory quarantine, fear and worry about becoming infected and developing a fatal case, as well as the higher incidence of mental disorders, mainly anxiety and depression.28 In addition, being university students and facing the difficulties of the academic load, they could face problems of fewer hours of sleep.29 It is noteworthy that in Peru, a lower frequency of insomnia–hypersomnia (39.5%) has been described before the pandemic,30 which would highlight the role that the pandemic had on the quality of sleep of university students.
Sleep quality and mental disordersSleep quality plays an important role in college students due to its neuroprotective effects.31 This study showed that poor sleep quality was associated with suspected psychopathology in college students. This fact supports previous studies where it was reported that university students with symptoms of anxiety or depression had poorer sleep quality.27,32 This would highlight the fact that sleep health and mental health are correlated and that, in stressful situations such as the pandemic, it is necessary to identify these disorders for timely intervention, having as the first agent of surveillance the family nucleus in the students’ homes.5
Regarding the associated components, we found that shorter sleep duration has been associated with poor mental health. In this regard, it has been reported that fewer hours of sleep influences mood, and increases anxiety symptoms, as well as the risk of suffering mental, physical and cognitive health problems.33,34 This shorter sleep duration could be due to the existence of stressors that delay sleep reconciliation in this population, such as thoughts related to the strenuous academic load, exposure to blue lights from electronic devices, and social, and emotional factors, as well as mental health problems.35–37 Educational interventions on the importance of sleep and how to sleep, as well as raising awareness of the negative effects of electronic device use before bedtime, could be low-cost strategies to decrease sleep disorders.
Also, it was found that the use of hypnotic medication was associated with poor mental health, in addition, it was previously found that the use of sedatives and tranquilizers led to high rates of depression and post-traumatic stress syndrome.38 Another study showed that those who used sedatives without medical prescription had poor sleep quality and had some mental health disorders.39 On the other hand, daytime dysfunction, which is defined as the inability to perform different tasks during the day, in this study was also associated with poor mental health, which coincides with a study conducted before the pandemic in Spanish workers.40 Daytime dysfunction causes a lower level of vigilance during the day, memory loss, fatigue, and lethargy.41 This would hinder academic performance and generate social problems, which would lead to a higher frequency of mental disorders in university students. Given these findings, it should be noted that evaluating the components of sleep quality is very important to assess possible risks of developing mental disorders.
Public health relevance and general recommendationIn Peru, the prioritization of patients infected with COVID-19 has meant that mental health assessment and intervention have been neglected. The present study showed a positive relationship between poor sleep quality and the suspicion of mental disorders; therefore, university and health authorities should implement measures to improve the quality of sleep in the university population, such as training for the development of sleep hygiene measures, for example, not taking virtual classes late at night, among others.42 Strategies should also be implemented to detect and intervene promptly for different mental disorders, such as providing virtual channels for psychological care43 and making the population aware of the importance of the use of health services so that they are properly used. In addition, families should be made aware so that they can be the first agents of vigilance in the detection of psychosocial and emotional problems of family members who are university students.
To mitigate the long-term negative effects, interventions applied in other countries are recommended, such as the creation of protocols for counseling, family accompaniment, avoiding academic overload, and flexible communication with the teacher.44 In addition, the activation of a telephone line for psychological counseling to deal with emergencies would contribute to better academic and social performance in the future.45
Limitations and strengthsAlthough the results of the present study are consistent with those reported in previous studies,46 the following limitations should be kept in mind. First, the sample only corresponds to students contacted by smartphone with Internet access at the time of the survey. Second, other variables of interest such as respondents’ medical conditions, whether they had a diagnosis of mental disorder or a pre-existing chronic disease, were not taken into account. Third, the students contacted through the survey only correspond to one university, so these results may not be generalizable to other contexts. Fourth, because the responses were self-reported, we may fall into respondent-related biases, such as recall bias. Fifth, we recognize that due to the lack of temporality we cannot assert causality, and there is the possibility that reverse causality contributes to this association.
In addition, psychiatric symptoms were analyzed in the present study through the PHQ-9 and GHQ-12, which evaluate the degree of psychological or emotional distress; however, no serious psychiatric disorders were identified, such as post-traumatic stress disorder,47,48 eating disorders,49 psychoactive substance use,50 social isolation and loneliness, suicidal ideation,51 nor how these could have affected the quality of sleep of the students during that period. Finally, this is the first study conducted on a random sample of students from a Peruvian jungle university that evaluated sleep quality and mental disorders after several months of confinement.
ConclusionsWe found that about three-quarters of the university students at the University of the Peruvian Amazon presented sleep problems, and 6 out of 10 presented suspected psychopathology, after being in mandatory confinement for more than 6 months. In addition, sleep disturbances were associated with mental health status. Therefore, it would be necessary to monitor sleep quality problems and mental health disorders to detect and intervene promptly, specially during public health emergencies such as the COVID-19 pandemic.
Authors’ contributionVMR, ASG conceived the study idea. VMR, MERG, ADLRP, JSRG, RMBV participated in data acquisition. VMR, ASG, BCC and DFG participated in the methodology, formal analysis, and interpretation of data. All authors drafted the manuscript; likewise, all authors participated in the critical revision and final approval.
FundingThis work was supported by the Universidad San Martín de Porres and self-funded by the authors for data collection, analysis, and preparation of the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
To Junior Panduro and Piero Pasache, for their support in data collection.