Whereas most studies have focused on how the religious beliefs positively interfere with the presence or execution of suicidal behaviors, few have identified differences among religious beliefs and how these can not only be consider as a protective factor for suicide, but also as a variable that influences the expression of the suicidal related behaviors.
ObjectiveTo provide evidence about the effect of religious practices and beliefs on suicidal behavior in cancer patients in Colombia.
MethodsThis is a hospital-based cross-sectional study with a sample of 132 patients with cancer. Socio-demographic data were measured, in which the religious affiliation was included. The instruments used include the Scale of Suicidal Ideation (SSI), the item 9 of Beck Depression Scale (BDI-IA) and the Beck Hopelessness Inventory (BHS).
ResultsIn our study, 93% of the patients had advanced stages of cancer, where 51.52% of them were in stage IV. Cancer patients who reported non-Catholic Christians were 3 and 4 times more likely to have some manifestation of suicidal behavior.
ConclusionsIt is recognized in non-Catholic Christians patients a greater chance to express suicidal ideation, which could be related to their level of suicide acceptability. It is considered that religion and their perception of death affects the expression and acceptance of suicidal ideation, reason why it is necessary more research on the effect of different religions on suicidal behavior, in order to include these aspects in the patient intervention.
Mientras que la mayoría de los estudios se han centrado en cómo las creencias religiosas interfieren positivamente con la presencia o la ejecución de conductas suicidas, pocos han identificado diferencias entre creencias religiosas y cómo estas no solo se pueden considerar un factor protector contra el suicidio, sino también una variable que influye en la expresión de los comportamientos suicidas.
ObjetivoProporcionar evidencia sobre el efecto de las prácticas y creencias religiosas en la conducta suicida de los pacientes con cáncer en Colombia.
MétodosEs un estudio transversal con una muestra de 132 pacientes con cáncer. Se aplicó la Escala de Ideación Suicida (SSI), el ítem 9 del Inventario de Depresión de Beck (BDI-IA) y el Inventario de Desesperanza de Beck (BHS); además, en la entrevista se recogieron datos sociodemográficos entre los que se incluye la afiliación religiosa.
ResultadosEl 93% de los pacientes presentaban estadios de cáncer avanzados, de los que el 51,52% estaba en estadio IV. Los pacientes con cáncer que informaron ser cristianos no católicos tienen 3 y 4 veces más probabilidades de alguna conducta suicida.
ConclusionesSe distingue en los pacientes cristianos no católicos una mayor expresión de la ideación suicida, lo que podría estar relacionado con el grado de aceptabilidad del suicidio. Se considera que la religión y su percepción de la muerte afecta a la expresión y la aceptación de las ideas suicidas, por lo que se requiere más investigación sobre el efecto de las diversas religiones en las conductas suicidas, con el objetivo de incluir estos aspectos en la intervención de los pacientes.
The suicide, as defined by the World Health Organization (WHO), is considered as an impulsive act aimed to deliberately end the life of the individual and can occur in the middle of moments of crisis, when the subject does not have proper coping strategies to deal with troubles mostly related to economic difficulties, chronic diseases, discrimination, abuse and violence, etc.1 The act of suicide, formerly addressed as suicidality, includes a range of suicide-related behaviors such as ideations or thoughts, communications and behaviors and is mainly characterized by self-initiation, potentially injurious behaviors and, in some degree, intent to die.2
According to the WHO, only a small portion of the population who have recognize thinking about suicide (suicidal ideation) will go on to attempt, and even less individuals will die by suicide;1 it has been found that suicidal ideation and nonlethal attempts (frustrated suicide behavior) are more common than lethal attempts.2 Epidemiologically, it has been recognized worldwide that the suicidal behavior has a sex pattern, where the male suicides outnumber the female suicides on a ratio of 4:1;2 however, the female nonlethal attempts outnumber the male attempts on a ratio of 3:1.1,2 Also it was found that the suicidal behavior is more common among older adults, people with major depression or other mental illness and people with chronic diseases recently diagnosed or in terminal phases.3 Indeed, in cancer patients the rate of suicidal behaviors has been found to be twice as high as in the general population.3–7 Commonly the general population has been related to risk factors that include previous mental illness like depression, previous suicidal attempts, poor social support, hopelessness and the presence of any chronic disease, in particular cancer.8 The cancer types that have more suicide risk are the gastrointestinal, breast, head and neck cancer, pancreatic cancer and also the hematologic malignances.3,4,6,8
In Colombia, during the period 2006-2015, 18 618 suicides were reported, with a gradual increase that has led to consider this as a public health problem. The age groups showing the highest rates of suicide were people between 15 and 34 years old (48.74%) and adults over 80 years old with a suicide rate 61% higher than the general population. While figures of suicide in people with cancer are still nonexistent in Colombia, in 2015 there were reported 259 suicide cases (27.6%) related to physical or mental illness.9 The role of some other social and psychological variables have been also discussed, in particular, related to religious perspectives and the way that moral and religious beliefs influence a person to communicate or act on the desire to die, as is discussed in this article.
It has been noticed how the suicidal ideation and its expression is influenced by religion in cancer patients, Ohnsorge et al.,10 in a study with 30 terminally ill cancer patients, noticed that some patients expressed a strong desire to die, but for moral or religious reasons rejected the idea of acting accordingly by keeping those thoughts for themselves.10 Also Spencer et al.4 identified in patients with advanced cancer that positive religious coping (the belief in a benevolent God) resulted in greater quality of life in advanced cancer patients, whereas negative religious coping (the belief in a punishing God or demonic appraisals) or no religious affiliation produced worse psychological outcomes and increases the risk of suicide-related behavior.4
Similar studies, such as the one of Yun et al.11 performed in 17 hospitals with a total of 3840 individuals among patients, family and oncologists, show that not having a religious affiliation is related with individuals who accepted assisted suicide, in fact 576 patients (48,8%) who reported not having a religious affiliation show to be more accepting of the idea of assisted suicide (odds ratio [OR]=1.55; CI, 1.30-1.72).11
In the same order, in Switzerland, Panczack et al.12 conclude that individuals without a religious affiliation have higher suicide rates compared with Catholics and accordingly the religion is consider as a protective factor for suicide in cancer patients. Specifically, these authors found that Protestants (41.9%) had a suicide rate of 27.5 (CI, 26.5-28.4), while Catholics (46%) had a rate of 18.6 (CI, 17.8-19.3) and finally people with no religious affiliation (12.2%) had a suicide rate of 39.0 (CI, 37.0-41.1).12 Furthermore, Shim et al.13 made a research study with 400 Korean cancer patients where they found that there is an association between religion and suicide, where not having a religious affiliation is related with a higher risk of suicide. It is noted in the univariate analysis, 126 people with no religious affiliation and suicide risk (P=.48; OR=1.66; CI, 1.01-2.77) and in the multivariate analysis, 99 people with no religious affiliation and suicide risk (P=.010; OR=2.25; CI, 1.21-4.16).13
With this in mind it can be considered that knowing the type of religious affiliation is important in the evaluation of the cancer patients among other factors in order to identify and prevent the suicidal behaviors.
From this point of view, individuals who reside in nations with a relatively high level of religiosity, like Colombia, have a lower level of suicide acceptability than the ones who reside in other countries,14 these is confirmed by Leal-Hernandez et al.15 when they suggest that in Colombia most of the people has denied having suicidal ideation due to their religious beliefs and its opinion on the respect for the human life. Likewise the Pan American Health Organization (PAHO) has talked about the importance of considering the cultural and religious factors involved in the report of suicides since these factors influenced by the stigma of suicide may generate that the recorded information is incomplete.16
Nonetheless, there is sparse evidence about the effect of religious practices and beliefs on suicidal behavior in cancer patients and about the mechanisms underlying. Based on above, this study examines the relationship between the suicidal related behaviors and the religious beliefs among cancer patients in Colombia.
MethodsType of study and populationThis is a hospital-based cross-sectional study. All participants included are cancer patients, over 18 years old who during the study received treatment in private oncology units in Bogotá, Colombia. The sample was drawn using a non-probabilistic scheme to complete 132 volunteer participants. Patients suffering from deafness or muteness, intubated or sedated, with cognitive disabilities or using antidepressants, or people with vomiting and/or diarrhea, or those who had just finished chemotherapy session at the time of the study were excluded.
ProceduresInitially, all patients were invited to participate, the objectives of the study and the confidential use of the information were explained, after that all the concerns and questions were resolved and it was requested the informed consent. Subsequently, several assessment instruments were applied to measure suicidal ideation and other biopsychosocial factors associated. After the interview, patients were fed back on the results of the evaluation and when there were patients who had suicidal ideation or suicide risk, they were referred to the Department of Psychology of the institution and finally, were given an information booklet about mental health care.
The scales and other measures presented below have been used for clinical care of patients in these cancer units so it has been found that patients understand the language, allowing the evaluation in the form of an interview facilitating the approach to the patient. As these instruments were presented in the form of an interview, special emphasis was made in reference to the cancer experience.
Among the instruments used include the Scale of Suicidal Ideation (SSI)17 to identify aspects of history of suicidal ideation and behavior. Based on the reported previously, it was considered that a score equal to or greater than 1 is indicative of risk of suicide. In addition, item 9 of the Beck Depression Scale (BDI-IA)18, which measures suicidal ideation and behavior, and the Beck Hopelessness Inventory (BHS) in the Spanish version of Bobes et al.19 Socio-demographic data were also measured, in which the religious affiliation and the status of being non-practicing was asked.
Statistical analysisDescriptive statistics and frequencies were calculated to characterize the study population. Crude association analyses were performed on socio-demographic and clinical variables, to determine their relationship with some suicidal demonstration. Comparisons were developed by means of cross-product odds ratios. A logistic regression model was finally adjusted in order to obtain measure of adjusted effects. To do that, a stepwise process of elimination of variables was carried out.20 All analyses were performed through STATA package version 14,21 and an alpha level of .05 was set for statistical significance.
Ethical issuesThis research project was assessed and approved by two ethics committees according to the Oncology Unit in which it was developing the evaluation of patients. All participants gave written informed consent. Patients did not receive financial remuneration for their participation but all received feedback from the evaluation, psychological support in case of need and an information booklet about mental health care.
ResultsA total of 132 patients were included in this study. The outcome variable was built binary by considering a positive result with every person who has at least one episode of the following: suicidal ideation, current death wishes, suicidal intentions, previous suicidal attempts or self-damaging thoughts. In the sample, it was found that 18 patients (13.64%) answered positively for ideation, meanwhile 13 people declared to have death wishes (9.92%). Also 5 individuals (3.79%) and 6 (4.55%) had intentions or frustrated suicidal attempts, respectively. Finally, 3 (2.27%) had harmful thoughts. The prevalence of suicidal demonstration was 21% (n=28). Respect to the stage of cancer, 31.06% of the patients were found in early cancer stages, 17.42% were in middle-advanced stage and most of the sample, the 51.52%, were in advanced stages. Only 6 people (4.54%) declared to suffer from another serious illness. As continuous variables, SSI and BHS had a mean of 0.7±2.55 and 2.89±2.89 respectively. Its maximum and minimum values were 0-18 and 0-14 in each case.
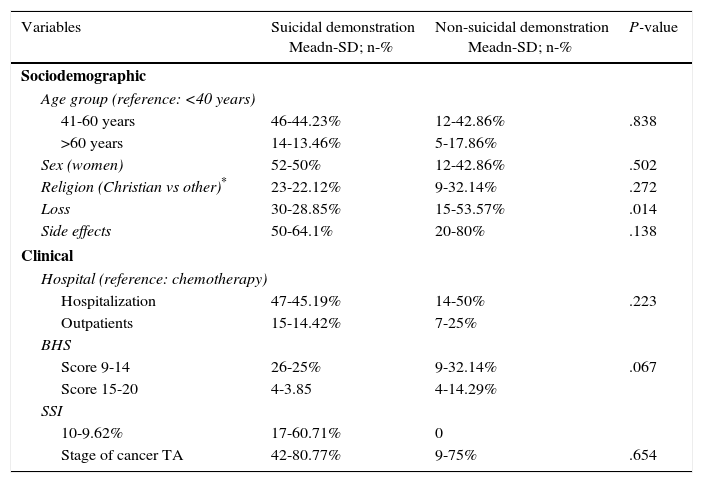
As is shown in Table 1, the patients with ages between 40 and 60 years, and also women have a higher percentage of suicide demonstrations. Moreover, even though the 80% of patients had no suicidal demonstrations associated with the side effects of cancer treatment, a significant percentage 64% had suicidal demonstrations.
General characteristics of the patients included.
| Variables | Suicidal demonstration Meadn-SD; n-% | Non-suicidal demonstration Meadn-SD; n-% | P-value |
|---|---|---|---|
| Sociodemographic | |||
| Age group (reference: <40 years) | |||
| 41-60 years | 46-44.23% | 12-42.86% | .838 |
| >60 years | 14-13.46% | 5-17.86% | |
| Sex (women) | 52-50% | 12-42.86% | .502 |
| Religion (Christian vs other)* | 23-22.12% | 9-32.14% | .272 |
| Loss | 30-28.85% | 15-53.57% | .014 |
| Side effects | 50-64.1% | 20-80% | .138 |
| Clinical | |||
| Hospital (reference: chemotherapy) | |||
| Hospitalization | 47-45.19% | 14-50% | .223 |
| Outpatients | 15-14.42% | 7-25% | |
| BHS | |||
| Score 9-14 | 26-25% | 9-32.14% | .067 |
| Score 15-20 | 4-3.85 | 4-14.29% | |
| SSI | |||
| 10-9.62% | 17-60.71% | 0 | |
| Stage of cancer TA | 42-80.77% | 9-75% | .654 |
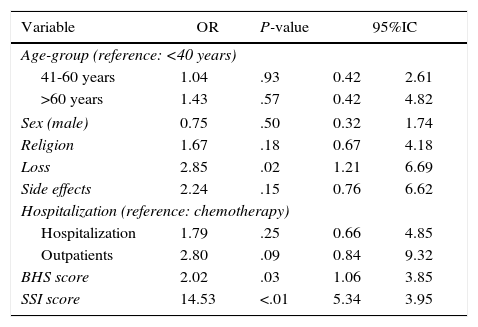
In the Table 1, despite there was a significant difference between the proportions of loss among patients with or without suicidal demonstrations (P=.014), that effect was not relevant in the adjusted model. The same happened with the crude comparisons of Table 2, where there was a significant difference between the proportions of loss, outpatients, BHS score and SSI score related to any suicidal demonstration.
Crude comparisons related to any suicidal demonstration.
| Variable | OR | P-value | 95%IC | |
|---|---|---|---|---|
| Age-group (reference: <40 years) | ||||
| 41-60 years | 1.04 | .93 | 0.42 | 2.61 |
| >60 years | 1.43 | .57 | 0.42 | 4.82 |
| Sex (male) | 0.75 | .50 | 0.32 | 1.74 |
| Religion | 1.67 | .18 | 0.67 | 4.18 |
| Loss | 2.85 | .02 | 1.21 | 6.69 |
| Side effects | 2.24 | .15 | 0.76 | 6.62 |
| Hospitalization (reference: chemotherapy) | ||||
| Hospitalization | 1.79 | .25 | 0.66 | 4.85 |
| Outpatients | 2.80 | .09 | 0.84 | 9.32 |
| BHS score | 2.02 | .03 | 1.06 | 3.85 |
| SSI score | 14.53 | <.01 | 5.34 | 3.95 |
Crude comparisons only show significant association between any demonstrations of suicidal behaviors except for loss, the binary version of BHS and SSI, with a positive OR associated in every case. The associated OR with the mourning was approximately three.
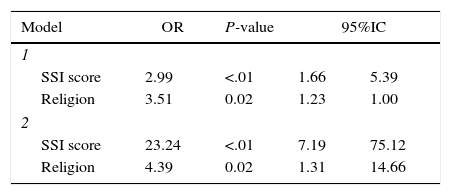
The logistic regression analysis showed too that patients with scores between 9-14 in BHS had a risk of suicide more than 8 times higher than patients with scores between 0-4 on this scale (OR=8.22; CI, 1.77-38.16; P=.007).
The adjusted model only kept significant effects for the variables of religion and the SSI scale. For religion, in our sample the findings show that being Christian represents an increasing of around four times in the odds of an occurrence of at least one suicidal demonstration. Meanwhile, the individual score on the SSI scale is related to an increase in the odds of approximately three (P<.001), however, the distribution of the variable is very biased to the left with 105 observations taking the zero value; due this, the model was re-built using a binary version of the score considering two groups: the zero values and any scoring as 1. This model produced an estimated OR=23. Details are presented in Table 3.
Despite the small number of predictors, this led to an overall model characterized by a correct classification power of 83.86% of the sample with a specificity of 98.8%, it means that with a high probability, over 80%, the predictors are capable to identify the individuals with an exceeded risk of coming of a group with any suicidal demonstration; complementary to this, the model also classified well to these individuals coming from group without demonstrations, roundly 100%. A test of the model against the constant-only model was significant, χ2 (df=2)=30.4.3 (P<.001), Nagelkerke R2=.32, indicating that the model statistically distinguished between the persons who had suicidal behaviors.
DiscussionThis study constitutes one of the first reported efforts in the literature to deepen in the recognition of suicide as a fundamental part in the emotional and social process of the patients with cancer. The findings of this study show that most of these patients (21%) consider at least one suicidal expression through the disease process and that they have a greater degree of hopelessness, score 9-14 points 0-4 points versus BHS, has a much higher probability (more than 8 times) suicidal risk. Therefore, we consider that it is necessary to evaluate the presence of hopelessness in cancer patients. While this data is not available to the general Colombian population, our findings are consistent with the official figures from the National Institute of Legal Medicine and Forensic Sciences (INMLCF)22 of this country, who exposed that, by 2013, 22.74% of the population who committed suicide had a physical or mental illness23 and also that this behavior was mostly prevalent in men.2
Regarding the diagnosis, as it has been previously reported, there is a clear relationship between the severity of the disease, the stage of the cancer and the frequency of the suicide manifestations.6,24 In our study, 93% of the patients had advanced stages of cancer, where 51.52% of them were in stage IV. This situation is potentially related to the diagnostic and therapeutic opportunities of the patients, observed as in the context of this research, which is often delayed and can be related to the experience of an emotional process affected by the same situation. Accordingly, the scope of this findings should be understood not only in the light of the effect of the disease but also taking into account the process of care and its shortcomings, in addition to the proposed in other researches.6,25
Structurally, the factor that in our study showed to be related to suicidal behavior was the practice of a religious belief. This situation is, however, mediated by the inability to determine whether if the behavior associated with the belief discourages or promotes the expression of a suicide manifestation;10 despite this, in the light of these findings, it is possible to establish a precedent to consider during the process of psychological assistance to people who claim to have a religious affinity. Taking into account that from what was found is not possible to consider such religious affinity as a factor associated with the decrease of expressions of suicide in people with cancer, since patients who reported to be non-Catholic Christians had between 3 and 4 times chance of occurrence. Indeed, in contrast with other findings,12 no relationship between being Catholic and a lower frequency of suicidal behavior was found.
In this regard, Stack26 findings indicate that religiosity serves as a protective factor for suicide acceptability, which would, indicated that according to our findings the patients recognized as non-Catholic Christians have high suicide acceptability and therefore express their suicidal behaviors. Accordingly, depending the religion the suicide acceptance varies affecting the expression of suicidal behaviors; nonetheless a question rises whether the religion actually stops the people from having death wishes or only prevents them from expressing their present thoughts due to the fear of being judged.
Other aspects to consider regarding the scope of our findings imply the recognition of some methodological limitations. First, the fact that this study was developed from a set of validated scales for Hispanic general population but not particularly for the Colombian population. This situation encourages the deepening of the approach given in this research as much as the effort to develop and adapt instruments to the specific characteristics of the population. Furthermore, the limited sample size prevents the generalization of the results. Finally, it should be noted that distributionally the sample is not homogenous in regard to the religious beliefs reported by the patients so the accuracy of the estimate could be compromised.
In view of the above, this study motivates the need to continue the investigation in terms of the specificity, adequacy and suitability of the interventions for the protection of the oncogenic patient, in particular with the concern of the effect on their psychological performance from the perspective of the role of a religious belief and their arising needs of assistance and care.
ConclusionsIn Colombia we have a high level of religiosity and a low level of suicide acceptability and frequently in the country the subject of suicide is avoided and disowned. This impact the clinical assessment of the patients and their care, in the way that the suicide risk many times is not evaluated in the patients and also because for fear of being judged the patients do not talk about their death wishes.
It is known that cancer patients experienced high levels of pain and suffering, many times accompanied by psychological and psychiatric issues that affect their quality of life and their will to live. Hereby it is important to inquire the presence of suicidal ideation on the patients in order to provide a proper intervention and improve the mental health of the patient.
The role of the mental health staff in the oncology units such as the psychiatrist and psychologist in the prevention, evaluation and treatment of these patients27 is extremely important taking into account the need for new interventions and assessment instruments that include for instance the evaluation of the suicide risk and the role that variables such as religion plays in the patient's life.
Because of that, is highlighted the importance of the investigations for the improvement of the mental health of the patients not only with cancer but also suffering with chronic diseases.28
This study also encourages the importance of inquiring about the role of the religion in the suicide assessment and the value of these findings in the development of an integrated intervention in these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestsThe authors declare no conflict of interest in this research.