Transcranial Doppler ultrasonography (TCD) is a technique that allows measurement of blood flow from the basal intracerebral vessels. It is relatively inexpensive, non-invasive, can be performed at the bedside, and allows monitoring in acute emergency settings and for prolonged periods with a high temporal resolution, making it ideal for studying the haemodynamics within the intracranial arteries in neuro-Behcet's disease (NBD) and neuro-psychiatric lupus (NPSLE). Our aim was to assess the cerebral haemodynamic patterns in patients with NBD and NPSLE using TCD, while brain lesions were examined using magnetic resonance imaging (MRI).
Material and methodsCase–control prospective study of 30 neuro-Behcet's disease patients, 25 neuro-psychiatric lupus patients and 26 healthy age-matched volunteers. All patients and healthy controls were examined by TCD. Only the groups of patients underwent cranial magnetic resonance imaging (MRI).
ResultsTranscranial Doppler (TCD) values for middle cerebral artery (MCA), anterior cerebral artery (ACA), posterior cerebral artery (PCA), vertebral artery (VA) and basilar artery (BA) in NBD, NPSLE and control groups were measured. The results showed that there was a significant decrease in mean blood flow velocities in all the arteries examined in NBD and NPSLE patients. There was also a significant increase in the pulsatile index of PCA, VA and BA between NBD and NPSLE patients. The same results were obtained when comparing NBD versus controls. However, there was no significant difference between the NPSLE patients and the control group. The MRI lesions described were parenchymal lesions in 14 patients (46.7%), and vascular lesions in 4 patients (13.3%). Vascular lesions co-existed with parenchymal lesions (mixed lesion). Parenchymal lesions were in white matter (40%), thalamus (26.7%), brain stem (26.7%) and cerebellum (20%). While, in NPSLE, 23 patients were normal (92%) and only two patients had a vascular lesion (8%).
ConclusionThere was a significant decrease in mean blood flow and a significant increase in the pulsatile index among both NBD and NPSLE patients, according to the TCD values.
La ecografía Doppler transcraneal (TCD) es una técnica que permite evaluar el flujo sanguíneo de los vasos intracerebrales basales. Es relativamente económico, no invasivo, se puede realizar al lado de la cama y permite la monitorización en situaciones de emergencia aguda y durante períodos prolongados con una alta resolución temporal, lo que lo hace ideal para estudiar la hemodinámica dentro de las arterias intracraneales en la enfermedad de neuro-Behcet (NBD) y neurolupus psiquiátrico (NPSLE). Nuestro objetivo fue evaluar los patrones hemodinámicos cerebrales en pacientes con NBD y NPSLE por TCD y lesiones cerebrales por resonancia magnética (RM).
Material y métodosEstudio prospectivo de casos y controles de 30 pacientes con enfermedad de neuro-Behcet, 25 pacientes con lupus neuropsiquiátrico y 26 voluntarios sanos de la misma edad. Todos los pacientes y controles sanos fueron examinados por TCD. Se realizó un examen de RM craneal a los grupos de pacientes.
ResultadosSe evaluaron los valores de Trance Cranial Doppler (TCD) para la arteria cerebral media, la arteria cerebral anterior, la arteria cerebral posterior (PCA), la arteria vertebral (VA) y la arteria basilar (BA) en los grupos NBD, NPSLE y control. Los resultados mostraron que hubo una disminución significativa en las velocidades medias del flujo sanguíneo en todas las arterias examinadas entre los pacientes de NBD y NPSLE. Además, hubo un aumento significativo en el índice pulsátil de PCA, VA y BA entre los pacientes con NBD y NPSLE. Se obtuvieron los mismos resultados al comparar NBD y controles. Por otro lado, no hubo diferencias significativas entre los pacientes con NPSLE y los controles. Las lesiones de resonancia magnética descritas fueron lesiones parenquimatosas en 14 pacientes (46,7%) y lesiones vasculares en 4 pacientes (13,3%). Existían lesiones vasculares junto con lesiones de parénquima (lesión mixta). Las lesiones de parénquima se localizaron en sustancia blanca (40%), tálamo (26,7%), tronco encefálico (26,7%) y cerebelo (20%), mientras que en NPSLE, 23 pacientes eran normales (92%) y solo 2 pacientes tenían lesión vascular (8%).
ConclusiónHubo una disminución significativa en el flujo sanguíneo medio y un aumento significativo en el índice pulsátil entre pacientes con NBD y NPSLE en los valores de TCD.
Behcet's Disease (BD) is classified among vasculitis. Central nervous system involvement in BD is due to chronic, recurrent vasculitis of the small blood vessels. Arterial thrombosis is a rare complication in BD with central nervous system involvement, while venous thrombosis is a major complication.1
Neurological manifestations in systemic lupus erythematosus (SLE) have been commonly presented and well-studied. On the other hand neurological manifestations are less prevalent in other systemic inflammatory and autoimmune disorders like Behcet's disease.2
In SLE, one of the most serious complaints is the nervous system involvement which includes a wide variety of neurologic and psychiatric manifestations. The central neurologic features of NPSLE usually have diffuse symptoms that closely resemble bipolar disorder.3 It may be difficult to differentiate between SLE and atherosclerotic disease (lipohyalinosis) as a cause of stroke in SLE patients with diabetes or hypertension, who are at risk for conventional small-vessel cerebrovascular disease.4
TCD allows insight into cerebrovascular function in many central nervous system disorders.5,6 Sharma et al. reported that TCD enables a reliable assessment of blood flow from the basal intracerebral vessels.7 Our aim was to assess cerebral hemodynamic patterns in patients with NBD and NPSLE by TCD and brain lesions by MRI.
Material and methodsThis study included thirty patients with neuro-Behcet's disease (28 males and 2 females) who fulfilled the criteria of the International Study Group for Behcet's disease (ISGBD, 1990)8; 25 patients with NPSLE diagnosed according to The American College of Rheumatology Nomenclature and Case Definitions for Neuropsychiatric Lupus Syndromes9; 26 healthy age-matched volunteers were enrolled as a control group. Patients were selected from the outpatient clinics and inpatient departments of the Physical Medicine, Rheumatology and Rehabilitation departments at Assiut University and Al-Azhar (Assiut) Hospitals..
Exclusion criteria included: (1) patients less than 18 years old, or more than 40 years; (2) pre-existing clinical evidence of cardiovascular disease, such as cardiac, hypertensive, or cerebrovascular events (angina, myocardial infarction, transient ischemic attack, stroke or vertebrobasilar insufficiency); (3) history of psychosis or other neurological diseases involving the central nervous system which hindered patient cooperation; (4) history of brain ischemia due to cardiorespiratory arrest; (5) other systemic diseases including renal impairment or failure, history of drug abuse leading to central nervous system involvement (such as liver and renal diseases, AIDS, and endocrine conditions); (6) a history of cancer identified over the past five years; and (7) patients with primary vasculitis.
A qualified rheumatologist took a complete history of the patient and conducted a comprehensive clinical examination, and a neurological examination was also conducted in all patients with the help of a qualified neurologist.
Both, patients and controls, underwent a Transcranial Doppler (TCD), while MRI was only done in patients. The Transcranial Doppler was performed with a Nicolet Bravo model 460 SNF0000001544 with a 2MHz probe (Neurocare, Madison, WI). TCD provides direct and non-invasive assessment of vascular changes. Transcranial Doppler examinations were performed at the department of Neurology and Psychiatry, Clinical Neurophysiology Unit, Assiut Neurology, Psychiatry and Neuroscience University Hospital. The right anterior cerebral artery (ACA) was recorded via a trans-temporal window and the depth of insinuation recorded between 60 and 90mm. The subject's head was in neutral position. The right middle cerebral artery (MCA) measured via trans-temporal window and the depth of insonation was between 30 and 60mm. The subject's head was placed in neutral position. The right posterior cerebral artery (PCA) was accessed via a trans-temporal window and the depth of insonation was between 60 and 80mm. The subject's head was placed in a neutral position. The right vertebral artery (VA) was recorded via a sub-occipital window and the depth of insonation was between 60 and 90mm. The subject's head was placed in a neutral position. The right basilar artery (BA) was measured via a sub occipital window. The depth of its insonation was between 80 and 120mm. The subject's head was placed in a neutral position. The systolic mean velocity (MV) and pulsatile index (PI) were recorded. PI is equal to the peak velocity minus the end-diastolic velocity, divided by the mean velocity.10 PI normally ranges between 0.5 and 1.1.11
Only the group of patients underwent a cranial MRI (FLAIR, T1 and T2 sequences) using a Philips, Achieva, 1.5T MRI device. The images were performed by the same radiologist. The MRI assessed the evidence of organic focal lesions and identified the site involved.
A written informed consent was obtained from all the participants (NPSLE, NBD and control) before entering the study. This study was reviewed and approved by the ethics committee of Faculty of Medicine, Assiut University and Al- Al-Azhar (Assiut) university, Egypt.
StatisticsUpon completion of the data collection process, all the data were entered in a Microsoft Excel program. Then the data were transferred to SPSS software version 20 package (IBM Corporation, Armonk, NY) for data analysis. Standard descriptive statistics were used, including mean and standard deviation for normally distributed continuous variables, and median and interquartile range (Q1; Q3) for non-normally distributed continuous variables; absolute numbers and percentages for categorial variables. The results analyzed by using One-way analysis of variance (ANOVA) followed by a post hoc test (LSD) and Chi-squared test Fisher's exact probability test. The distribution characteristics were assessed with the Kolmogorov–Smirnov test. Kruskal–Wallis test and Man–Whitney U test were used for comparison after testing all the variables in the transcranial doppler findings for normal distribution; all of the variables showed a skewed distribution of nonparametric data. The significance level was set at p<0.05.
ResultsThis study included 30 patients with NBD with a mean age of 30.27±8.29 years and a male predominance (28 males and 2 females); the mean disease duration was 4.67±3.19 years. The study also included 25 patients with NPSLE with a mean age of 27±7.69 with female predominance and mean disease duration of 4.76±2.65. These two groups were compared against a control group of 26 subjects with mean age of 28.4±8.97.
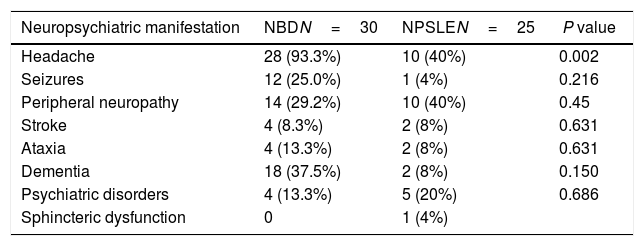
Table 1 shows that the most salient neuropsychiatric symptom was headache with 93.3% in NBD and 40% in NPSLE. The neuropsychiatric manifestations recorded in NBD were headache (93.3%), dementia (37.5%), peripheral neuropathy (29.2%), and seizures (25%). In NPSLE the most common symptoms were peripheral neuropathy and headache (40%); the psychiatric symptoms included depression, anxiety, psychosis (20%), while dementia, ataxia and stroke were present in 8% of the cases.
Neuropsychiatric manifestations in neuroBehcet's disease (NBD) and neuropsychiatric SLE (NPSLE).
| Neuropsychiatric manifestation | NBDN=30 | NPSLEN=25 | P value |
|---|---|---|---|
| Headache | 28 (93.3%) | 10 (40%) | 0.002 |
| Seizures | 12 (25.0%) | 1 (4%) | 0.216 |
| Peripheral neuropathy | 14 (29.2%) | 10 (40%) | 0.45 |
| Stroke | 4 (8.3%) | 2 (8%) | 0.631 |
| Ataxia | 4 (13.3%) | 2 (8%) | 0.631 |
| Dementia | 18 (37.5%) | 2 (8%) | 0.150 |
| Psychiatric disorders | 4 (13.3%) | 5 (20%) | 0.686 |
| Sphincteric dysfunction | 0 | 1 (4%) |
Data described as number and percentage.
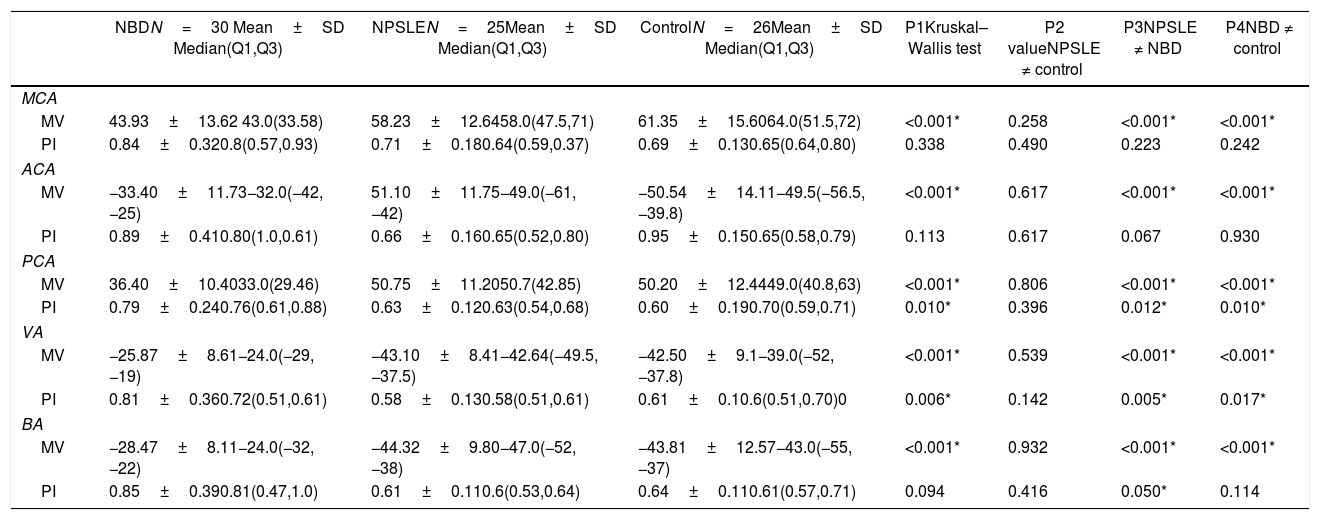
Table 2 shows the TCD values for MCA, ACA, PCA, VA and BA in NBD, NPSLE and the control groups. The results showed a significant decrease in mean blood flow velocities in all the arteries examined between NBD and NPSLE patients. Additionally, there was a significant increase in the pulsatile index of PCA, VA and BA between NBD and NPSLE patients. The same results were obtained when comparing NBD and controls. On the other hand, there was no significant difference between NPSLE patients and controls.
Comparison of transcranial Doppler between neuroBehcet's disease (NBD), neuropsychiatric SLE (NPSLE) and control.
| NBDN=30 Mean±SD Median(Q1,Q3) | NPSLEN=25Mean±SD Median(Q1,Q3) | ControlN=26Mean±SD Median(Q1,Q3) | P1Kruskal–Wallis test | P2 valueNPSLE ≠ control | P3NPSLE ≠ NBD | P4NBD ≠ control | |
|---|---|---|---|---|---|---|---|
| MCA | |||||||
| MV | 43.93±13.62 43.0(33.58) | 58.23±12.6458.0(47.5,71) | 61.35±15.6064.0(51.5,72) | <0.001* | 0.258 | <0.001* | <0.001* |
| PI | 0.84±0.320.8(0.57,0.93) | 0.71±0.180.64(0.59,0.37) | 0.69±0.130.65(0.64,0.80) | 0.338 | 0.490 | 0.223 | 0.242 |
| ACA | |||||||
| MV | −33.40±11.73−32.0(−42,−25) | 51.10±11.75−49.0(−61,−42) | −50.54±14.11−49.5(−56.5,−39.8) | <0.001* | 0.617 | <0.001* | <0.001* |
| PI | 0.89±0.410.80(1.0,0.61) | 0.66±0.160.65(0.52,0.80) | 0.95±0.150.65(0.58,0.79) | 0.113 | 0.617 | 0.067 | 0.930 |
| PCA | |||||||
| MV | 36.40±10.4033.0(29.46) | 50.75±11.2050.7(42.85) | 50.20±12.4449.0(40.8,63) | <0.001* | 0.806 | <0.001* | <0.001* |
| PI | 0.79±0.240.76(0.61,0.88) | 0.63±0.120.63(0.54,0.68) | 0.60±0.190.70(0.59,0.71) | 0.010* | 0.396 | 0.012* | 0.010* |
| VA | |||||||
| MV | −25.87±8.61−24.0(−29,−19) | −43.10±8.41−42.64(−49.5,−37.5) | −42.50±9.1−39.0(−52,−37.8) | <0.001* | 0.539 | <0.001* | <0.001* |
| PI | 0.81±0.360.72(0.51,0.61) | 0.58±0.130.58(0.51,0.61) | 0.61±0.10.6(0.51,0.70)0 | 0.006* | 0.142 | 0.005* | 0.017* |
| BA | |||||||
| MV | −28.47±8.11−24.0(−32,−22) | −44.32±9.80−47.0(−52,−38) | −43.81±12.57−43.0(−55,−37) | <0.001* | 0.932 | <0.001* | <0.001* |
| PI | 0.85±0.390.81(0.47,1.0) | 0.61±0.110.6(0.53,0.64) | 0.64±0.110.61(0.57,0.71) | 0.094 | 0.416 | 0.050* | 0.114 |
MCA: middle cerebral artery; ACA: anterior cerebral artery; PCA: posterior cerebral artery; VA: vertebral artery; BA: basilar artery; MV: mean velocity; PI: pulsatility index; Mann Whitney test was used in P2, P3 and P4.
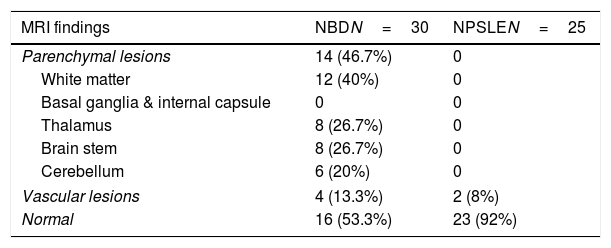
With regards to NBD, the MRI was normal in 16 patients and abnormal in 14 patients. The MRI lesions described were parenchymal lesions in 14 patients (46.7%), and vascular lesions in 4 patients (13.3%). The vascular lesions co-existed with parenchymal lesions (mixed lesion). The parenchymal lesions were located in white matter (40%), thalamus (26.7%), brain stem (26.7%) and cerebellum (20%). While in NPSLE, 23 patients were normal (92%) and only two patients had vascular lesion (8%). The vascular lesions identified were dural venous thrombosis and transverse venous thrombosis (Table 3).
Localization of MRI finding in neuroBehcet's disease (NBD) and neuropsychiatric SLE (NPSLE).
| MRI findings | NBDN=30 | NPSLEN=25 |
|---|---|---|
| Parenchymal lesions | 14 (46.7%) | 0 |
| White matter | 12 (40%) | 0 |
| Basal ganglia & internal capsule | 0 | 0 |
| Thalamus | 8 (26.7%) | 0 |
| Brain stem | 8 (26.7%) | 0 |
| Cerebellum | 6 (20%) | 0 |
| Vascular lesions | 4 (13.3%) | 2 (8%) |
| Normal | 16 (53.3%) | 23 (92%) |
Data described as number and percentage. NBD: Neuro Behcet’ Disease; NPSLE: neuropsychiatric SLE.
Systemic autoimmune diseases such as Behcet's disease and SLE affect multiple systems, and the nervous system is one of them.12 According to our knowledge, no trial has been conducted to compare the two diseases, even though both conditions have been associated with immune-mediated mechanisms, which according to the pathology exhibit small vessel vasculopathy in the parenchyma of the nervous system. So, as far as we know, this study could be considered first one to be conducted in the Middle East comparing the two illnesses. However, the current study showed a female predominance in NPSLE patients (22/3) as compared with NBD (2/28), and the NPSLE patients were generally younger than the NBD group (25.0±7.69, 30.27±8.29 respectively). Moreover, NPSLE patients had a greater tendency towards diffuse manifestations than NBD, though the possibility of a referral bias cannot be completely ruled out. In Behcet's disease headache is the most frequent neurological symptom.13 However, peripheral neuropathy and headache tend to be higher in the NPSLE patients. This is the cause of the different patterns of neuropsychiatric presentations between the NPSLE and NBD patients, which may be suggestive of a different immunologic process in NPSLE as compared with NBD.
In terms of the cerebrovascular changes assessed by transcranial doppler, there was a significant reduction in the mean velocity and an increase in the pulsatile index in the groups of patients studied (NBD and NPSLE), as compared with the control group, in most of the vessels studied.
Transcranial Doppler ultrasonography has been used in many central nervous system disorders to allow insight into cerebrovascular function. However, TCD does not measure actual blood flow, but flow velocity through the basal cranial arteries. However, few studies have been performed using TCD in neuro-BD.14 Gosling PI was originally designed to measure vascular resistance. The increased PI observed in our study presumably represents enhanced cerebrovascular bed resistance in the cerebral circulation due to cerebral vasculitis in NBD or NPSLE.
This is consistent with previous literature showing TCD abnormalities in the form of micro embolic signals which were more significant in patients with neurological involvement due to BD, than in patients with no neurological involvement.15 The study by Gad et al. showed similar findings (decreased velocity and increased pulsatile index), mainly in MCA.16 Two additional studies showed significant changes in the flow parameters of the vertebral artery in patients with BD. These changes are probably secondary to vasculitis of the vertebral artery in BD.14,17 A previous study using color-coded duplex zoography in patients with BD, also found ocular and cerebral hemodynamic changes, including increased acceleration in the MCA.18 The TCD results in our study are consistent with our previous study by Shehata et al, which reported significant increases in the mean velocities and decreases in the pulsatile index of most of the intracranial vessels studied in SLE patients, as compared with the controls.19 These increases and decreases can be explained by narrowing, constriction, stenosis or occlusion of the vessel in most pathologic conditions affecting the large intracranial arteries, which results in increased mean flow velocity and decreased pulsatile index.20 In our study, the cerebrovascular changes in NPSLE were more significant as compared with NBD.
Vascular changes in NBD and NPSLE patients may be due to multiple causes, but ischemia is widely accepted to play a major role in causing CNS disorders in SLE patients, and reperfusion of an ischemic area carries the risk of edema.21 The probable explanation is the wide range of SLE antibodies in contrast to Behcet's disease. These auto-antibodies are believed to play two different, but not mutually exclusive roles in mediating neurological injury; direct injury to the neural target cells and antibody-induced rheological disruptions leading to infarction.21 Of these two mechanisms, antibody-induced rheological disruptions are widely accepted to be the major event resulting in CVD; however, diffuse neural damage caused by antibody-mediated mechanism may be the reason why NPSLE patients tend to exhibit diffuse manifestations. Vascular changes and subsequent microinfarcts determined by histopathological studies of the nervous system in SLE patients were also observed, although true vasculitis was rare.22 In our study, the parenchymal involvement was more prominent among NBD patients, and absent in NPSLE, while vascular changes were present in both. In NBD, vasculitis was the main pathological process of Behcet's disease, and the pattern of the parenchymal lesions seen on cranial MRI was consistent with small vessel vasculitis and inflammation of the veins. However, there are contradictory reports on the observed pathology, and the observed histopathological changes span a broad spectrum, including vasculitis, low grade inflammation, demyelization and degenerative changes. Definite vasculitis has not been observed in all cases.12
Our results showed that parenchymal lesions are mainly in white matter (40%) followed by the thalamus and the brain stem (26.7%) and lastly the cerebellum (20%). There is however another study which found that brain stem is the most affected structure, followed by white matter and lastly the basal ganglia.14
The limitations of this study are the relatively small number of patients and a small control group, in addition to the fact that the study was conducted only in two hospitals. Therefore, our recommendation is to pursue further multicenter studies with a larger number of patients.
Although our study was on small population, we think that TCD can provide a sensitive and accurate bed-side non-invasive imaging tool for the detection of flow pattern abnormalities in patients with NBD and NPSLE. MRI remains the gold standard for diagnosis.
In conclusion, according to TDC values, there was a significant decrease in the mean blood flow and a significant increase in the pulsatile index among NBD and NPSLE patients. Further large scale, multicenter studies should be pursued.
FundingNo funding was received for this study.
Conflict of interestsThe authors have no conflict of interests to disclose.