Primary angiitis of the central nervous system is an uncommon disease that may affect adults and the pediatric population. It can involve both the medium-large and small sized cerebral blood vessels, and can be associated with inflammatory, infectious, tumor processes, or of idiopathic origin. The case is presented of an adolescent with focal neurological impairment due to right hemiplegia, in whom other more frequent causes of cerebral ischemia were ruled out. The final diagnosis was Epstein Barr virus associated with primary angiitis of the central nervous system.
La vasculitis primaria del sistema nervioso central es una enfermedad infrecuente que puede afectar a adultos y población pediátrica. Puede comprometer los vasos sanguíneos cerebrales tanto de mediano o gran calibre como los de pequeño calibre y estar asociada a procesos inflamatorios, infecciosos, tumorales o ser de origen idiopático. Describimos el caso de un adolescente con deterioro neurológico focal dado por hemiplejía derecha en quien se descartaron otras causas más frecuentes de isquemia cerebral, con diagnóstico final de vasculitis primaria del sistema nervioso central asociada a infección por virus de Epstein Barr.
Vasculitis with involvement of the central nervous system (CNS) is a cerebral inflammatory disease that, although rare, has begun to be recognized more frequently in children as a cause of cerebrovascular accident (CVA).1 It is characterized by an angiocentric inflammation of the vascular wall or the perivascular space of the cerebral blood vessel2 that does not occur in the context of a systemic inflammatory disease, since in that case, it would be classified as secondary CNS vasculitis.3 In 1988 Calabrese et al. proposed some diagnostic criteria for primary angiitis of the CNS (PACNS) in adults4 that included: (1) new neurological deficit, (2) angiographic or histological characteristics of CNS vasculitis and (3) no evidence of systemic disease associated with the findings; to date, these criteria are used also in pediatric population with minimum modifications.3,5
3 types of PACNS have been described in children6: (1) large vessel disease or visible by angiography in progressive variant, (2) non progressive, and (3) small vessel disease or not visible by angiography but detected in biopsy.7
The PACNS in children has a varied clinical presentation, including neurological (focal or diffuse) or psychiatric symptoms, as well as headache, nuchal rigidity, seizures and even constitutional symptoms such as fever, nausea and fatigue.8
The diagnosis of large or medium blood vessel disease is based on findings suggestive of vasculitis in nuclear magnetic resonance angiography (MRA) or in conventional angiography,9 while the small vessel disease requires a biopsy for its diagnosis.7
We will describe the case of a 14-year-old adolescent with seizures and subsequent right hemiplegia, in whom systemic inflammatory disease was ruled out and who underwent MR angiography with characteristic findings of PACNS.
Case presentationA 14-year-old adolescent boy, previously healthy, who consulted due to a clinical picture that occurred 2 days before admission, consisting of a tonic position of the left hemibody that alternated with clonus therein, supraversion of the gaze (upward gaze), urethral sphincter relaxation of unknown duration, subsequent disorientation and dysarthria. With an initial cranial CT scan without lesions and a cranial CT scan taken 24h later showing a hypodense lesion in the left temporo-occipital region with involvement of basal nuclei.
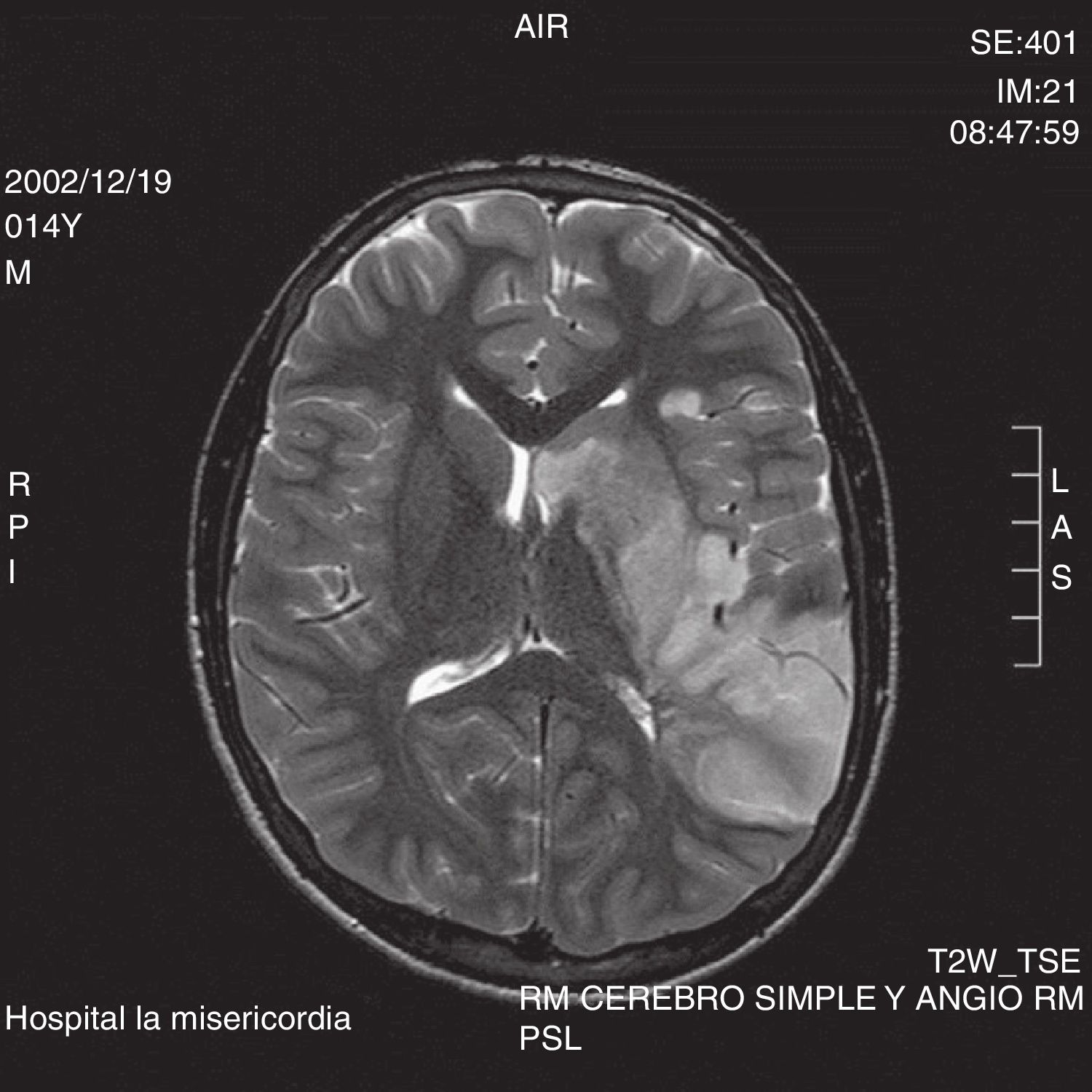
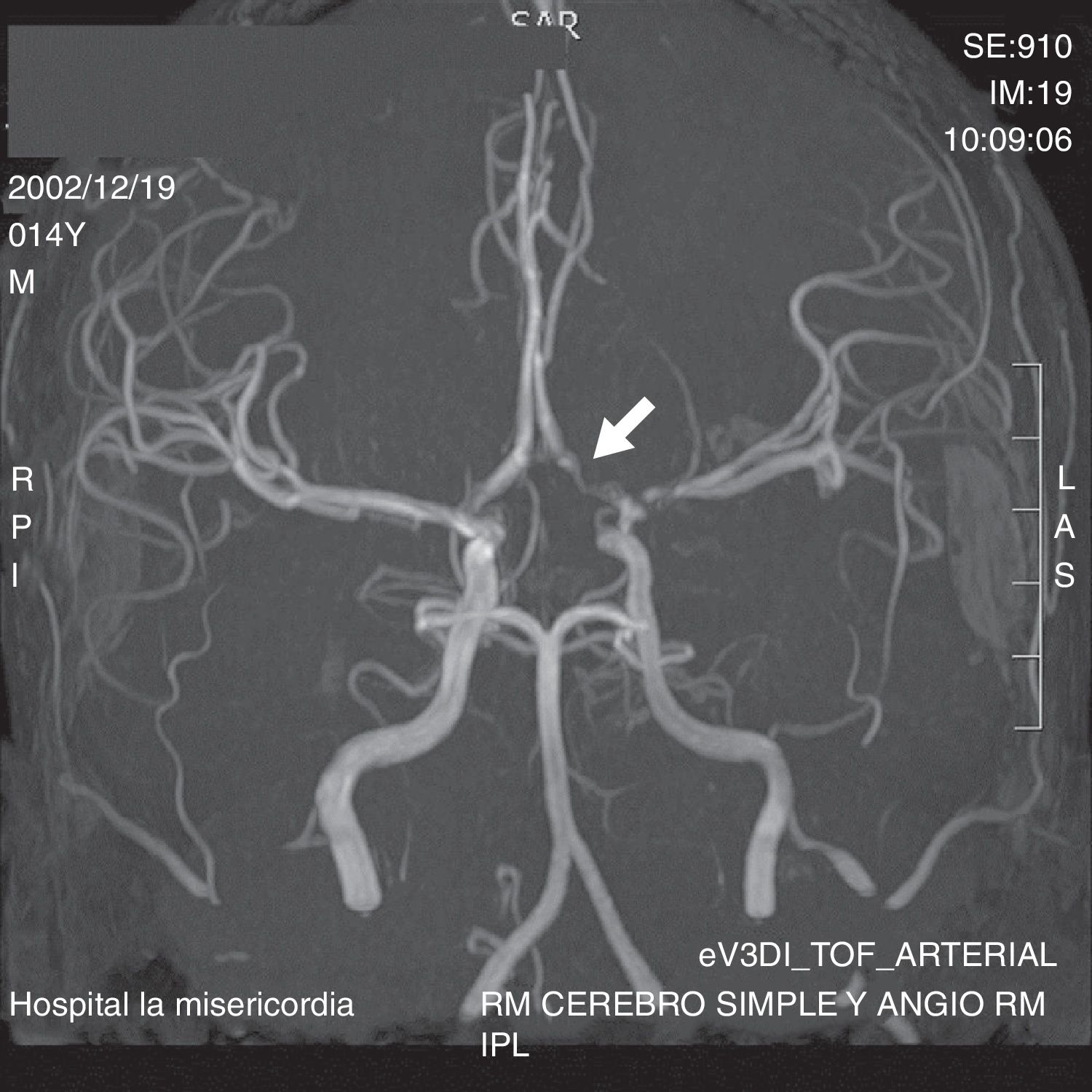
On admission, the patient had stable vital signs, without control of sphincters, somnolent, with right central facial paralysis and right hemiplegia, motor aphasia, without other alterations to the physical examination or alterations in initial paraclinical tests (blood count, C-reactive protein, electrolytes, glycaemia, clotting times). The studies were extended with simple and contrasted MRI of the brain, which showed a lesion described as hyperintense in T2 and hypointense in T1 with restricted DWI and ADC that involved the left temporal anterior pole, the insula and the temporal lip of the ipsilateral operculum, compromised by edema, with irregularity of the M1 lumen, stenosis of the carotid artery in the supraclinoid portion and of the anterior cerebral siphon in the proximal portion but with competent communicating and middle cerebral arteries in the M1 portion with early bifurcation. (Fig. 1) There was no significant mass effect due to edema, changes of hemorrhagic transformation, or anatomical lesions susceptible to management by neurosurgery.
Studies were expanded for coagulation disorders (fibrinogen, D-dimer, protein C, protein S, antithrombin III, activated protein C resistance, factor V Leiden, prothrombin mutation) and for systemic inflammatory disease (antinuclear antibodies, anti- DNA, complement, extractable nuclear antibodies, anti-β2 glycoprotein antibodies, anticardiolipins and lupus anticoagulant), all of them reported as negative. Likewise, nitrogen compounds, lipid profile, Doppler of the neck vessels, angio-CT and electrocardiogram were performed, all reported as normal. It was found only an elevation of uric acid, which was corrected after one week of management with allopurinol, and the presence of patent foramen ovale in the echocardiogram, with intermittent left-to-right shunt, which is not considered to be the cause of CVA due to paradoxical embolism because of the pathophysiological mechanism. It was decided to initiate anticoagulation of the patient with low molecular weight heparin (dalteparin 5000IU every 12h applied subcutaneously) adjusted by anti-factor XA.
The patient was taken to MRA, which showed acute infarction in the left middle area of the cerebral territory, without signs of hemorrhagic transformation, with irregularity of the wall and loss of signal in the territory of the left internal carotid artery in its cavernous and supraclinoid portions and with extension to the emergence or the anterior and middle cerebral arteries of the left side, related to the inflammatory-vasculitic process (Fig. 2). For this reason, isolated vasculitis of the CNS (type transient focal arteriopathy) was considered as the first possibility, and therefore, boluses of 1g of methylprednisolone every day for 3 days were started, followed by 1mg/kg of prednisone daily. Given the impossibility to perform a biopsy due to the location of the lesion, it was decided to initiate cyclophosphamide (15mg/kg). A viral profile was taken prior to the start of immunosuppressive therapy, with negative reports for HIV, toxoplasma, cytomegalovirus, herpes I and herpes II, but with positive IgG and IgM for Epstein Barr.
During the hospitalization he presented isolated episodes of headache that subsided with conventional analgesia. After the management established, he presented progressive improvement of the neurological deficit; at discharge, he presented the use of coherent but poor language to answer questions, persistence of nominal aphasia, right hemiparesis with improvement in strength with respect to admission and persistence of the right central facial palsy, which was only noticeable when he was asked to smile, with adequate seating; and was able to walk, but with support. For this reason, the patient was discharged with the indication to continue corticosteroid, cyclophosphamide, and a panangiography was requested on an outpatient basis.
DiscussionThe PACNS is defined in the pediatric population as a psychiatric or neurological deficit, focal or diffuse, recently acquired in a patient ≤18 years, associated with characteristic histopathological, angiographic or MRA findings, in the absence of an underlying disease that explains or mimics the clinical picture.1,3 It is a condition that must be taken into account within the pediatric differential diagnoses of a CVA: cerebral arteriopathies are the cause of up to 80% of cerebral ischemic events in children.10 Its current incidence is approximately 2–4 cases per million patients/year,11 however, these data may be biased due to the heterogeneity of the multiple denominations of the disease as well as to the complexity of its diagnosis, for which there are no criteria validated in pediatrics.12 Interestingly, there is a slight predominance of PACNS of large vessels in children, which coincides with a higher prevalence of ischemic events in this population.13
The PACNS can be classified according to the angiographic findings in those with involvement of medium and large-sized vessels (angiography+), and with involvement of small vessels (angiography−). The first type is more common in men than in women and is classified, in turn, into progressive and non-progressive variants, which are distinguished by the appearance or not of new segments of stenosis, respectively, in an angiographic control performed 3 months after the first image. The second type is, on the contrary, more common in women than in men, and since the angiography or the MRA are normal here, a biopsy with demonstration of intramural and perivascular lymphocytic infiltrates should be performed for the diagnosis.3,7 The terms transient cerebral arteriopathy or transient focal arteriopathy correspond to synonyms of PACNS of median and large-sized vessels: all of them are referred to as unilateral focal brain arteriopathies in the primary classification of CVA in children.14
The cause of the PACNS is unknown. Genetic factors have not been studied systematically. However, it has recently been proposed that patients with mutations in the DOCK8 gene, which encodes a protein of T and B lymphocytes and is associated with immunodeficiency, may have a higher risk of developing PACNS.15 There are common viral infections that can be triggers, associated with the non-progressive variant of PACNS of large or medium-sized vessels,16 mainly the varicella zoster virus, but herpes simplex virus, cytomegalovirus, human immunodeficiency virus and Epstein Barr virus are also reported, the latter found in our patient.17 However, the relationship between the presence of antibodies against these viruses and the presence of a clinical picture of PACNS has not been clarified so far. The infection, whether viral, bacterial, fungal or parasitic, could be both a differential diagnosis (direct infection of the arterial wall) and a trigger of the inflammatory cerebral arteriopathy that these patients present (postinfectious arteriopathy).18 Increased levels of certain cytokines such as IL-1 and IL-6 have also been found in children with the same variant of PACNS.18,19 A lymphocytic infiltrate with predominance of CD8+ was observed in the pathology study of biopsies performed in patients with PACNS of small vessels.20
Children with PACNS may have diverse neurological or psychiatric manifestations.21 In general, the PACNS that affects large and medium-sized vessels manifests itself with acute symptoms such as a CVA, a subarachnoid hemorrhage, a transient ischemic attack or minor prodromal symptoms.22–24 On the other hand, the PACNS that compromises the small-caliber vessels exhibits a symptomatology of more gradual onset such as persistent headaches, progressive focal neurological deficits, cognitive deterioration, character disorders, changes in behavior or focal seizures, which constitutes a true diagnostic challenge for the pediatrician.25 In the case of the patient, the symptoms were from the beginning focal neurological of sudden onset, which is consistent with the type of PACNS diagnosed.
Currently, there are no specific laboratory tests that allow the diagnosis of PACNS, which is a diagnosis of exclusión.26 The erythrocyte sedimentation rate, C-reactive protein, leukocytes and immunoglobulins may be elevated; however, their normality, as well as of other inflammatory markers do not exclude PACNS.25 On the other hand, antinuclear antibodies, antineutrophil cytoplasmic antibodies, anticardiolipins, extractable nuclear antibodies, rheumatoid factor and angiotensin-converting enzyme are also usually negative.9 Prothrombotic diseases should be studied, especially in patients who present an ischemic stroke. Such is the case of our patient, in whom all the studies to rule out an underlying systemic disease or cardiac embolism were negative. The cerebrospinal fluid analysis can show leukocytosis in less than 50% of the cases of PACNS, which is more frequent in the PACNS of small vessels, followed by the progressive form of PACNS of medium and large-sized vessels.3,27
The imaging studies needed for the diagnosis of PACNS are angiography and MRA.28 The MRI studies often reveal unilateral ischemic lesions in the territory of large vessels in the PACNS of medium and large-sized vessels.29 In the non-progressive form of the PACNS, the MRA reveals a thickening of the vessel wall and enhancement with the gadolinium contrast due to the inflammation of the blood vessel. The anterior cerebral territory, especially, is often affected, and much less frequently, the posterior.30 The sensitivity and specificity of these findings is controversial and the different studies have not demonstrated superiority of conventional angiography over MRA in the diagnosis of PACNS of vessels of large and medium caliber.29 A selective involvement of the distal segment of the internal carotid artery, the proximal segment of the anterior cerebral artery, the middle cerebral artery, or a combination of these can be observed in the anterior circulation.31 The compromised arterial territory seems to be typical in patients with non-progressive PACNS of large and medium-sized vessels, and explains the higher frequency of involvement of the basal ganglia due to their exclusive irrigation by the leukostriate artery, branch of the proximal segment of the middle cerebral artery.32 In the case of the patient, there was an area of ischemia in the territory of the left middle cerebral artery, compromising the basal ganglia.
The differential diagnosis of PACNS in children includes secondary vasculitis of the CNS, non-vasculitic inflammatory brain diseases, non-inflammatory vasculopathies and cerebral vasospasm.16 Due to the clinical difference between the 2 variants of PACNS of large and medium-sized vessels (progressive and non-progressive) in children, the differential diagnosis is different for each type. In the case of the PACNS of medium and large vessels, the differential diagnosis includes non-inflammatory vasculopathies and cerebral vasospasm.16 Fibromuscular dysplasia can cause similar symptoms, however, it is diagnosed more frequently in middle-aged women with arterial hypertension. In children, this disease can cause fatal cerebral arterial ischemia.33 The studies contrasted with gadolinium might be the best way to differentiate the PACNS from fibromuscular dysplasia34: in the latter, an intraluminal dissection is observed. Moyamoya disease can also cause similar symptoms. However, it occurs in the context of type I neurofibromatosis and is angiographically characterized by the presence of multiple collateral blood vessels (Moyamoya vessels) that are formed at the site of stenosis in the major vessels.35 There are also genetic alterations that can manifest themselves with cerebral vasculopathy,36,37 such as Fabry's disease, metabolic myopathies or homocystinuria. Certain channelopathies or drugs can be associated with vasospasm and produce a similar clinical picture, in particular certain recreational drugs, such as cocaine or amphetamines, can cause a prolonged vasoconstriction that produces a secondary vasculitis.38 The complete clinical history is very important to clarify the etiology, given the wide range of differential diagnoses that include inflammatory brain disease and its non-inflammatory simulators.39
The objectives of the treatment of the PACNS are the control of the active intramural inflammation, the prevention of secondary ischemic events, the improvement in the remodeling of the blood vessel, the control of the associated symptoms (neurological or psychiatric) and the prevention of complications derived of the disease itself and its treatments.16 In children, each subtype of PACNS requires a different therapeutic strategy. In children with the non-progressive variant of PACNS of large or medium-sized vessels, boluses of methylprednisolone are usually administered for 3–5 days, followed by high doses of prednisolone with de-escalation of the dose during 3 months until a dose of 1mg/kg/day. This regime is associated with antithrombotic treatment and substitution with calcium and vitamin D.8,16 The effectiveness of the treatment is usually assessed by performing a neuroimaging study at 3 months; in the case of stabilization of the lesion (not new areas of stenosis) and absence of new neurological symptoms, immunosuppressive treatment is discontinued. On the other hand, children who present new lesions or neurological symptoms are reclassified to the progressive variant and should receive treatment for this entity.16
Children with PACNS of large and medium caliber vessels, progressive variant, or PACNS of small vessels, have a severe inflammatory brain disease and require another type of immunosuppression in addition to corticosteroids. The drug that has been used with relative success is cyclophosphamide, although there are no prospective studies that confirm the findings in the case reports.3,40,41 The current treatment for this type of PACNS consists of 6 months of high immunosuppression with monthly pulses of cyclophosphamide, associated with prophylactic treatment against Pneumocystis jirovecci, high doses of prednisolone (2mg/kg/day) for one month (followed by progressive dose de-escalation) associated with an antithrombotic treatment, calcium and vitamin D supplementation, in addition to symptomatic control (for example, use of anticonvulsants).21 It is continued with a maintenance treatment that can be done with mycophenolate or azathioprine; the duration, in general, is 18 months both in the progressive variant of large or medium-sized vessels and in the PACNS of small vessels.21,42,43
ConclusionPACNS is a disease that, although rare, should be considered within the differential diagnoses in pediatric patients presenting with focal or generalized involvement of the CNS. Its diagnosis is of exclusion, after an adequate clinical history and subsequent paraclinical approach that rules out other entities to which the symptoms of the patient can be attributed. When suspecting the diagnosis, the study should be extended with angiography or MRA, remembering that only patients in whom these images are reported normal should go to histopathological study. The timely initiation of immunosuppressive therapy ensures the favorable impact on the recurrence of new episodes and on the improvement of the symptomatology presented by the child, as is the case of our patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingOwn resources of each co-author were used for the implementation of this article.
Conflict of interestThe authors declare they do not have any conflict of interest
Thanks to the Radiology Service of the Hospital la Misericordia for its valuable contribution and help in the evaluation of the images of this patient.
Please cite this article as: Romero FV, Rincón AD, Maldonado AS. Vasculitis primaria del snc en poblacion pediátrica: reporte de caso y revisión de la literatura. Rev Colomb Reumatol. 2018;25:301–306.