Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in the paediatric age. It is estimated that between 30–60% of adults patients persist with active disease, which leads to sequelae and complications as well as a decrease functional capacity and reduced quality of life.
ObjectivesTo evaluate the health-related quality of life in adult patients diagnosed with juvenile idiopathic arthritis.
MethodologyA cross-sectional study was performed, using a search for adult patients diagnosed with JIA between 1996 and 2018. Clinical records were reviewed during the paediatric age, and clinical parameters were evaluated for activity (JADASc-71), and joint (JADI-A) and extra-articular (JADI-E) damage, functional capacity (HAQ), and quality of life (SF-36). Relationships were determined by non-conditional logistic regression.
ResultsA total of 69 patients were included. The most frequent subtype of JIA was enthesitis-related arthritis (ERA) (33%). Active disease was observed in 33%. Polyarticular JIA RF (+) was associated with active disease (P = .007), high values of JADASc-71 (P = .003), and HAQ (P = .001). Age of onset after 5 years reduced risk of joint damage (OR = 0.16) and extra-articular damage (OR = 0.03). Poor therapeutic adherence was associated with joint damage (P = .00) and JADASc-71 (P = .004). A high score of JADI-E was associated with functional disability (OR = 5.75). Joint damage (P = .003) and extra-articular damage (P = .024), and functional disability (OR = 7.05) were associated with low values in the SF-36.
ConclusionsJIA is not a disease limited to the paediatric age. Persistence of active disease, joint, and extra-articular damage are associated with functional disability and a decrease in H-RQoL.
La artritis idiopática juvenil (AIJ) permanece activa en el 30–60% de pacientes adultos, conduciendo a complicaciones articulares, extra-articulares, disminución en la capacidad funcional y reducción en la calidad de vida.
ObjetivosEvaluar la calidad de vida relacionada con la salud en pacientes adultos con diagnóstico de artritis idiopática juvenil.
MetodologíaEstudio corte transversal, se realizó una búsqueda de pacientes adultos con diagnóstico de AIJ entre 1996–2018. Se revisaron historias clínicas durante la edad pediátrica y se evaluaron parámetros clínicos para actividad (JADASc-71), daño articular (JADI-A) y extra-articular (JADI-E), capacidad funcional (HAQ) y calidad de vida (SF-36). Asociaciones determinadas por regresión logística no condicional.
ResultadosSe incluyeron 69 pacientes. El subtipo de AIJ más frecuente fue la artritis relacionada con la entesitis (ARE) (33%). 33% de los pacientes tenían enfermedad activa. AIJ poliarticular FR + se asoció con enfermedad persistentemente activa p = 0,007, altos valores del JADASc-71 p = 0,003 y HAQ p = 0,001. Edad de inicio posterior a 5 años redujo el riesgo de daño articular OR = 0,16 y extra-articular OR = 0,03. Mala adherencia terapéutica se asoció a daño articular p = 0,00 y JADASc-71 p = 0,004. Alta puntuación del JADI-E se asoció con discapacidad funcional OR = 5,75. El daño articular p = 0,003 y extra-articular p = 0,024 y discapacidad funcional OR = 7,05 se asociaron con bajos valores en SF-36.
ConclusionesLa AIJ no es una enfermedad limitada a edad pediátrica. Persistencia de enfermedad activa, daño articular y extra-articular se asocian con discapacidad funcional y disminución en la calidad de vida relacionada con la salud (CVRS).
Juvenile Idiopathic Arthritis (JIA) is the most prevalent rheumatic disease in pediatric patients. There are different presentations of chronic arthritis in patients under 16 years old. In addition to the joint involvement, the disease may affect various organs and present systemic manifestations, depending on the subtype; this heterogeneity is also reflected in the evolution, prognosis and treatment.1–3 JIA is a significant cause of disability in children and adolescents; several studies have identified between 30 and 60% of adult patients with persistent active disease, depending on the subtype of arthritis. JIA conditions the articular and extra-articular complications, hence affecting quality of life.2,3
Quality of life is defined as “an individual's perception of their position in life in the context of the culture and value system in which they live and in relation to their goals, expectations and standards and concerns.” A number of instruments have been developed to assess health-related quality of life (HRQL), designed to determine the impact of the disease on quality of life.4 Among the pediatric population patients are reported to have a lower HRQL score with regards to self-esteem, and adolescents in all the areas assessed, with a more severe compromise of their physical wellbeing. Approximately 1/5 of the patients with JIA exhibit behavioral disorders, usually anxiety or depression. In general, the most affected area in children with JIA is physical function – which is influenced by the magnitude of the functional impairment and pain intensity.5
The impact of the disease on HRQL has also been described in adults. As a whole, all the areas assessed in HRQL in patients with JIA were compromised according to the report, as compared against the general population, with pain being the most significantly affected area, followed by psychiatric disorders (anxiety and depression), limitation of daily activities and impaired mobility and severe disability, all showing a statistically significant difference as compared to the control group. There were other additional predictors of low HRQL scores including female gender, older age, level of education, disability, and good compliance with pharmacological therapy.4
Over the years, and as a result of increased awareness of the disease, improved diagnosis and early onset of treatment, severe physical complications have decreased and functional capacity has improved. However, the challenge is not just to reduce physical decline and functional impairment, but to approach the social, emotional and family aspects leading to an improved quality of life in the short and long term, and ensure adult autonomy.6 Consequently, the purpose of this study was to assess the impact of JIA on HRQL of adult patients, and related clinical, demographic and social factors.
Materials and methodsA cross-sectional study was conducted to learn about the HRQL of adult patients diagnosed with JIA. The study population comprised adult patients with a final diagnosis of JIA, that were included in the registry of the pediatric rheumatology clinic between 1996 and 2018, and with a duration of the disease equal or greater than 5 years. The patients were relocated and invited to participate; they accepted to join the trial and signed the informed consent. Patients with a follow-up by rheumatology of less than 2 years were excluded. This study was assessed by the ethics committee of the Universidad El Bosque, that considered that this was a “minimum risk” trial and gave its approval.
For the selection and size of the sample, the sample size was estimated using the proportion P = .41, keeping in mind that we don’t have an actual prevalence of the disease studied, with a population of 200 patients with JIA. Considering a 95% confidence level, an alpha of 5, and an error of 10%, the number of participants required would be n = 64. This analysis was conducted using the Openepi statistical software (www.OpenEpi.com).
During the procedure to collect the information, the first step was patient identification from the database of the clinic. Then each medical record was reviewed and the initial information was entered into data collection form. These patients were invited to undergo an assessment which included: update of demographic and socio-economic data, clinical assessment and the administration of quality of life surveys. During the active search of patients, 69 adult patients were identified. To assess the disease activity, the clinical Juvenile Arthritis Activity Index of 71 joints (JADASc-71) was used, which provides an overall assessment of the disease by the physician, an overall assessment of the disease by the patient or caregivers, and identifies the number of joints with active arthritis. The sum total of the results of the 3 parameters represents the final JADAS score, which ranges between 0 and 91, classifying the disease as inactive with a score of less than or equal to 1; if there is oligoarticular involvement: low activity with a score of 1.1–2; moderate activity between 2.1 and 4.2, and high activity >4.2 and in patients with polyarticular involvement: low activity with a score between 1.1 and 3.8; moderate activity between 3.9 and 10.5; and high activity >10.5.7
The assessment of damage secondary to the disease, whether at the articular or extra-articular level, was assessed using the Juvenile Arthritis Damage Index (JADI), a tool that comprises the assessment of the articular and extra-articular damage (JADI-A and JADI-E), respectively.8 The JADI-A includes the assessment of 36 joints or groups of joints and its maximum score is 72. It assessed 3 main forms of joint damage: persistent involvement (at least 6 months duration and not due to active arthritis), the range of movement is limited and is associated to the presence of deformity, and a history of prior surgical interventions such as joint replacement, arthrodesis and arthroplasty. Partial damage is a score of greater than or equal to 1, and severe damage is a score or greater than or equal to 2, or the presence of anchyloses or need for prostheses. JADI-E is defined as the presence of persistent changes in the anatomy, the physiology, the disease or the function, which may occur from the very onset of the disease, as a consequence of activity or therapy, and which last for at least 6 months. The range of measurement is from 0 to 17, and is considered damage when the score is greater than or equal to 1. The assessment includes the following complications: 1) ophthalmological such as cataracts, uveitis, need for eye surgery and blindness; 2) non-articular musculoskeletal damage including fractures secondary to osteoporosis, muscle atrophy, vertebral misalignment, avascular necrosis and localized growth disorders in a particular segment; 3) cutaneous findings such as red streaks, subcutaneous atrophy secondary to the intra-articular injection of steroids; 4) endocrinological abnormalities such as growth failure, diabetes mellitus and pubertal delay, and 5) amyloidosis.8
The functional status was assessed via the Health Assessment Questionnaire (HAQ), which consider 4 parameters: disability, pain, drug-related adverse events and costs. A score of 0 indicates absence of disability, from 0.1 to 0.5 = moderate disability and a score of more than 1.5 = severe disability. Finally, to assess HRQL, the health-related quality of life questionnaire SF-36 was used, which has been validated in Colombia. This includes 36 parameters grouped into 8 areas: physical function, physical performance, discomfort, emotional performance, mental health, vitality, general health status, and social functioning. The first four assess the physical component and the rest correspond to the mental component. Furthermore, there is one element not included in these 8 categories, which explores the changes experienced in the health status over the last year. The scores in each of the 8 areas range from 0 (worst condition for that area) to 100 (the best health status for that area) and a reference factor for the components established in the healthy population of 50 ± 10.9
In the statistical analysis, all the data were analyzed using SPSS Statistics 23.0.0. and Stata 12. A descriptive analysis was conducted for all the variables, through a frequency analysis, central tendency and dispersion measurements. A bivariate analysis for quantitative variables was conducted and the distribution of the data was analyzed using the Shapiro–Wilk test. Then, the Kruskal–Wallis and Mann–Whitney tests were used to compare the quality of life scores in accordance with the activity of the disease, the presence of joint damage, extra-articular damage, and the subtypes of the disease. The comparison of frequencies between the categorical variables according to age, subtypes, rheumatology parameters, and markers, was performed using chi square/Fisher’s exact test. Some multivariate, logistical regression models were implemented to adjust variables in terms of the activity of the disease, articular and extra-articular damage, and the physical and mental quality of life. The odds ratio (OR) was estimated to determine the magnitude of the association among the variables. The results were considered significant when P < .05.
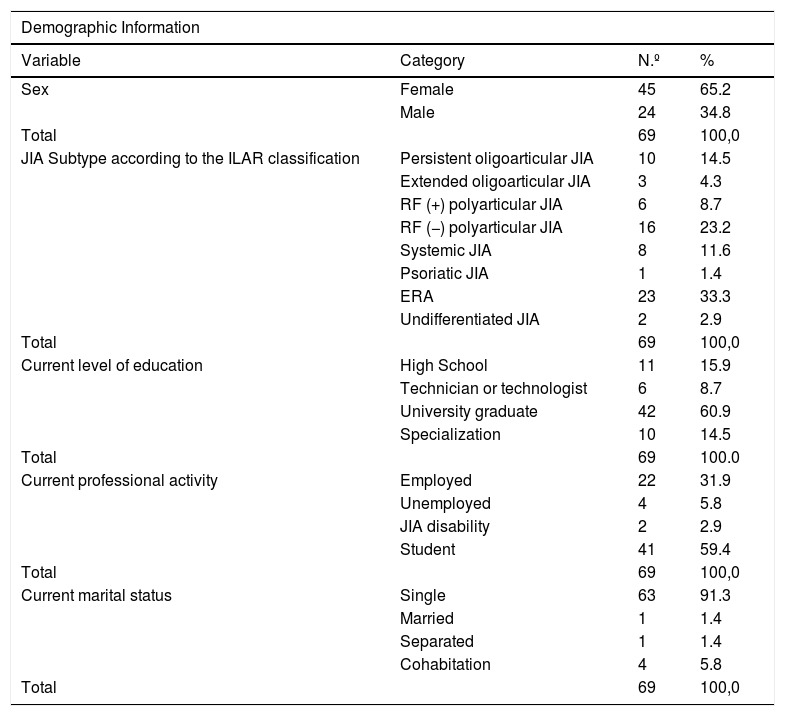
Results69 patients were identified and admitted into the trial. Of the 69 patients assessed, 65% (45) were females, with a gender distribution of F 1.9: M 1 for the JIA subtypes, except for the ERA subtype where the distribution was M 2: F 1 (Table 1).
Demographic characteristics of adult patients with a diagnosis of JIA.
| Demographic Information | |||
|---|---|---|---|
| Variable | Category | N.º | % |
| Sex | Female | 45 | 65.2 |
| Male | 24 | 34.8 | |
| Total | 69 | 100,0 | |
| JIA Subtype according to the ILAR classification | Persistent oligoarticular JIA | 10 | 14.5 |
| Extended oligoarticular JIA | 3 | 4.3 | |
| RF (+) polyarticular JIA | 6 | 8.7 | |
| RF (−) polyarticular JIA | 16 | 23.2 | |
| Systemic JIA | 8 | 11.6 | |
| Psoriatic JIA | 1 | 1.4 | |
| ERA | 23 | 33.3 | |
| Undifferentiated JIA | 2 | 2.9 | |
| Total | 69 | 100,0 | |
| Current level of education | High School | 11 | 15.9 |
| Technician or technologist | 6 | 8.7 | |
| University graduate | 42 | 60.9 | |
| Specialization | 10 | 14.5 | |
| Total | 69 | 100.0 | |
| Current professional activity | Employed | 22 | 31.9 |
| Unemployed | 4 | 5.8 | |
| JIA disability | 2 | 2.9 | |
| Student | 41 | 59.4 | |
| Total | 69 | 100,0 | |
| Current marital status | Single | 63 | 91.3 |
| Married | 1 | 1.4 | |
| Separated | 1 | 1.4 | |
| Cohabitation | 4 | 5.8 | |
| Total | 69 | 100,0 | |
IJA: idiopathic juvenile arthritis; ERA: enthesitis-related arthritis; RF: Rheumatoid Factor; ILAr: International League of Associations of Rheumatology.
The mean age during the adult assessment was 22 years, with a standard deviation (SD) of 4 years. The average age at the time of diagnosis of the disease was 9 years (SD 4 years). The mean duration of the disease was 12 years, with an interquartile range between 8 and 16 years. In order to carry out the bivariate analysis, the age of the patients was categorized at the beginning of the disease in quinquennials. In 47.8% of the patients (33) the onset of the disease was between 11 and 15 years, followed by the patients between 5 and 10 years old representing 28.9% (20) and in a smaller proportion – 23.2% (16) – the group of patients with an onset of the disease before 5 years of age. The bivariate analysis of the age of onset according to the subtype of JIA, showed no statistically significant differences, except for the FR positive polyarticular JIA subtype, where the onset of the disease occurred between 11 and 15 years old (P = .028) and an interesting trend was observed in the persistent oligoarticular JIA groups with onset of the disease before 5 years old (P = .063) and in ERA between 11 and 15 years (P = .060).
The most frequent subtype identified was ERA with 33.3% of the patients, followed by: polyarticular RF negative JIA 23.2%, Polyarticular JIA 18.8% (with a distribution of 10 patients with persistent oligoarticular compromise and 3 with extended oligoarticular JIA), systemic JIA 11.6%, polyarticular RF positive JIA AIJ 8.7% and to a lesser extent subtypes undifferentiated JIA 2.9%, and just one patient with psoriatic JIA.
In terms of the level of education of the patients at admission to the trial, 75.3% (52) of the patients had completed higher education (60.9% university education and 14.5% master’s degree or specialization); 15.9% (11) of the patients completed high school and 8.7% (6) completed technical or technological education. There were no patients with less than high school education. With regards to occupational activity, 91.3% (63) of the patients were actively working or in the academic environment. 59.4% (41) of the patients were university students, 31.9% (22) were formally employed, 5.8% (4) were unemployed and 2.9% (2) were disabled as a consequence of the disease (one patient with subtype RF negative polyarticular JIA, and una patient with ERA). With regards to marital status, 91.3% (63) were single, 5.8% cohabitation, and 1.4 and 1.5% were married and divorced, respectively.
During the clinical assessment conducted to join the trial, the number of compromised joints was recorded as active, painful or limited. There was a mean of 1 active joint with a minimum of 0 and a maximum of 19 active joints; the mean for painful joints was 2, with a minimum of 0 and a maximum of 21 joints, and an average of 3 limited joints, with a minimum of 0 and a maximum of 45 joints. Using a visual analogue scale, patient pain perception was assessed with a mean of 1.55, with a SD of 2.4 and a range between 0 and 8; similar findings were reported in the assessment conducted by the doctors, with a mean of 1.33 and SD of 2.34.
During the evaluation of the disease activity, the mean JADASc-71 was 4.1, with a range between 0 and 29, and a SD of 7.2. A minimum activity was found in 3% (2) of the patients, moderate activity in 6% and severe activity in 25%. The JADASc-71 led to the conclusion that patients with RF positive polyarticular JIA exhibited a severe activity of the disease during adulthood (P = .003), with a statistically significant difference and no statistical significance was observed with the other subtypes of JIA.
The assessment of damage secondary to the disease was based on whether there was joint involvement with a mean JADI-A index of 2, a SD of 7. In the case of associated extra-articular damage, the result of the JADI-E index was a mean of 0 with a SD of 2. 74% (51) of the patients had no joint sequalae, 9% (6) were categorized as partial damage, and 17% (12) presented with clinical signs or a history of surgery to classify them as severe damage. There was a higher proportion of small joint involvement of the hands (carpal, metacarpophalangeal and interphalangeal), metatarsophalangeal joints and the temporomandibular joint, followed by compromised large joints – elbows, knees, hips, ankles, and cervical spine. There was a relationship between the RF negative polyarticular JIA subtype and high JADI-A values (P = .001), which means that these patients developed significantly more severe joint damage. Although there was no statistical significance, the patients with RF positive polyarticular subtype showed a marked tendency towards more relevant joint damage (P = .078).
The assessment of the extraarticular damage showed that there was a larger percentage of musculoskeletal involvement (10%). 9% (6) of the patients presented with severe muscle atrophy, followed by disrupted growth of the segments (associated with a significant mismatch in the length of the lower extremities) in 6% (4) of the cases; bone necrosis of the femoral heads was present in 4% (3) and osteoporosis and vertical vertebral misalignment were identified in one patient. Eye involvement was observed as the second most important presentation, evidenced by the presence of cataracts, blindness, and the need to undergo surgical procedures in 3% of the patients. Only in one patient (1%) was the final height affected as a result of the disease. There were no skin damage or a history of amyloidosis among the patients assessed, and there was no statistically significant difference between the JIA subtype and extraarticular damage (JADI-E).
The outcomes of the HAQ questionnaire showed a mean of 0.29, SD of 0.52, mean of 0 and a range between 0 and 2.9. In 25% of the patients the score was 0 and in 75% was 0.50. There was some degree of functional disability in 46.4% (32) of the patients, and the severity was classified as follows: mild disability 23%, moderate disability 20% and severe 3%. It was established that patients with seropositive JIA experienced mild to moderate functional disability more frequently (P = .001). This association was not evidenced in the other subtypes of JIA.
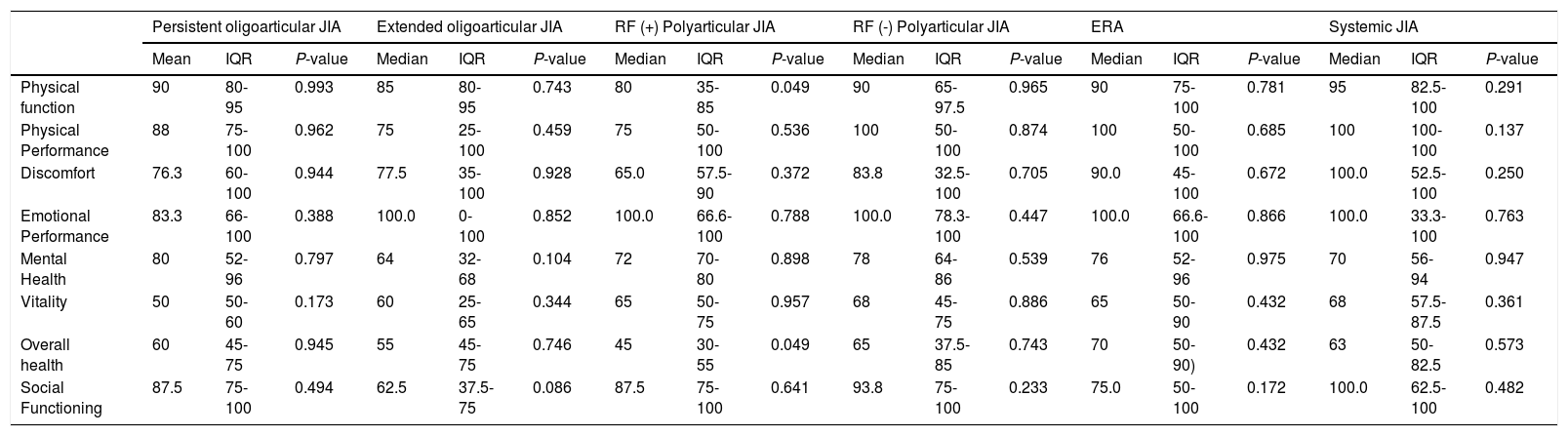
The HRQL assessment, taking into account the JAI subtypes, reported that there was no statistical association between the physical and mental health parameters in patients with oligoarticular JIA (persistent and extended). However, patients with extended oligoarticular JIA showed a tendency to lower social functioning levels (P = .086). Seropositive polyarticular JIA patients presented lower levels of physical function and overall health condition (P = .049). Whilst patients with seronegative JIA, did not exhibit any significant changes in the HRQL scores. In the systemic onset JIA subtype and in ERA, there were no statistically significant associations with low HRQL scores. The psoriatic JIA subtype exhibited a tendency to lower levels of physical (P = .087) and emotional performance (P = .069). No association was found with low quality of life in the other parameters. Patients with undifferentiated JIA showed higher ratings in physical health (P = .064) and general health (P = .045), and this difference was statistically significant (Table 2).
Relationship between the JIA subtype and the SF-36 parameters.
| Persistent oligoarticular JIA | Extended oligoarticular JIA | RF (+) Polyarticular JIA | RF (-) Polyarticular JIA | ERA | Systemic JIA | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | IQR | P-value | Median | IQR | P-value | Median | IQR | P-value | Median | IQR | P-value | Median | IQR | P-value | Median | IQR | P-value | |
| Physical function | 90 | 80-95 | 0.993 | 85 | 80-95 | 0.743 | 80 | 35-85 | 0.049 | 90 | 65-97.5 | 0.965 | 90 | 75-100 | 0.781 | 95 | 82.5-100 | 0.291 |
| Physical Performance | 88 | 75-100 | 0.962 | 75 | 25-100 | 0.459 | 75 | 50-100 | 0.536 | 100 | 50-100 | 0.874 | 100 | 50-100 | 0.685 | 100 | 100-100 | 0.137 |
| Discomfort | 76.3 | 60-100 | 0.944 | 77.5 | 35-100 | 0.928 | 65.0 | 57.5-90 | 0.372 | 83.8 | 32.5-100 | 0.705 | 90.0 | 45-100 | 0.672 | 100.0 | 52.5-100 | 0.250 |
| Emotional Performance | 83.3 | 66-100 | 0.388 | 100.0 | 0-100 | 0.852 | 100.0 | 66.6-100 | 0.788 | 100.0 | 78.3-100 | 0.447 | 100.0 | 66.6-100 | 0.866 | 100.0 | 33.3-100 | 0.763 |
| Mental Health | 80 | 52-96 | 0.797 | 64 | 32-68 | 0.104 | 72 | 70-80 | 0.898 | 78 | 64-86 | 0.539 | 76 | 52-96 | 0.975 | 70 | 56-94 | 0.947 |
| Vitality | 50 | 50-60 | 0.173 | 60 | 25-65 | 0.344 | 65 | 50-75 | 0.957 | 68 | 45-75 | 0.886 | 65 | 50-90 | 0.432 | 68 | 57.5-87.5 | 0.361 |
| Overall health | 60 | 45-75 | 0.945 | 55 | 45-75 | 0.746 | 45 | 30-55 | 0.049 | 65 | 37.5-85 | 0.743 | 70 | 50-90) | 0.432 | 63 | 50-82.5 | 0.573 |
| Social Functioning | 87.5 | 75-100 | 0.494 | 62.5 | 37.5-75 | 0.086 | 87.5 | 75-100 | 0.641 | 93.8 | 75-100 | 0.233 | 75.0 | 50-100 | 0.172 | 100.0 | 62.5-100 | 0.482 |
JIA: juvenile idiopathic arthritis; ERA: enthesitis-related arthritis; RF: rheumatoid factor; IQR: interquartile range.
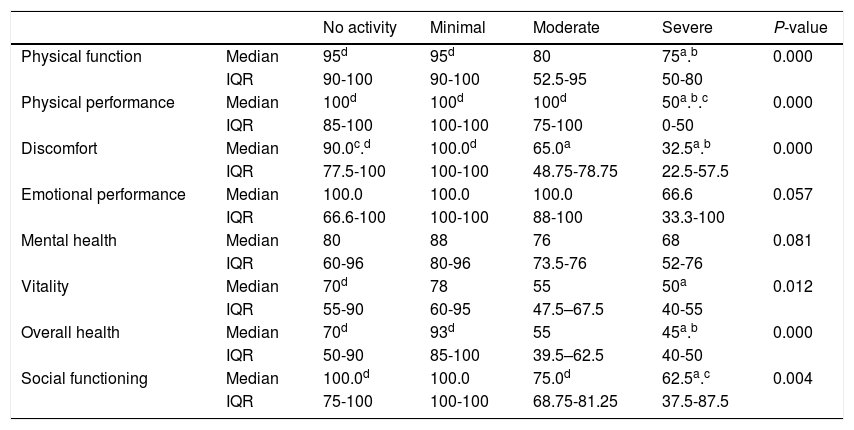
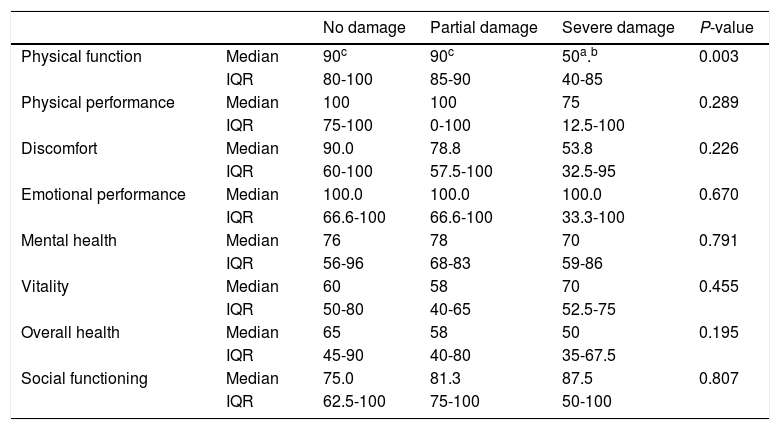
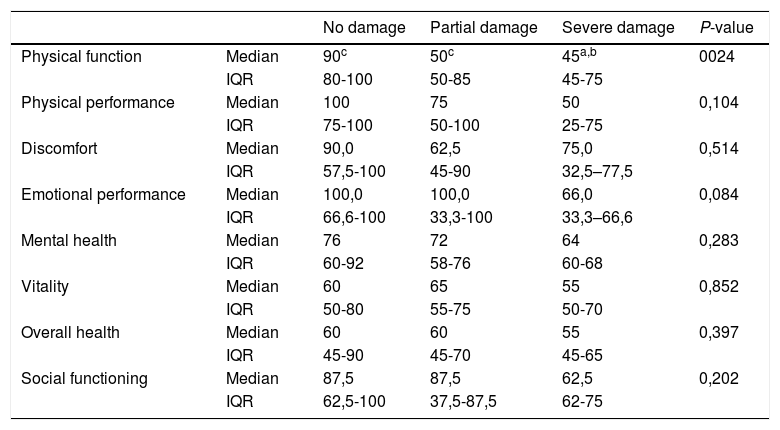
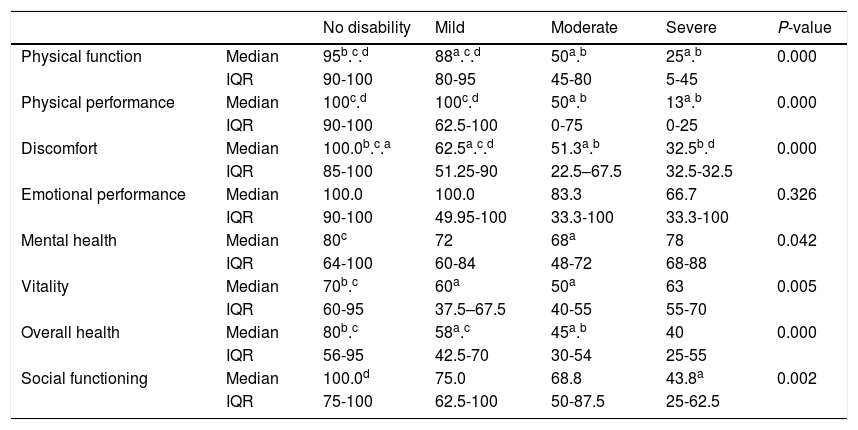
The severity of the disease activity was more significantly associated with low values in all of the physical parameters and vitality scores (Table 3). In terms of the presence of articular and extraarticular damage, patients with severe joint damage (P = .003) and severe extraarticular damage (P = .024) were associated with low physical function, with no compromise of the other physical assessment parameters or mental health (Tables 4 and 5). Patients with moderate to severe disability, showed a significant association with lower levels in all of the physical and mental health parameters, with the exception of emotional performance where there was no association (Table 6).
Health-Related Quality of Life Score Distribution in accordance with the severity of the disease activity (JADASc-71).
| No activity | Minimal | Moderate | Severe | P-value | ||
|---|---|---|---|---|---|---|
| Physical function | Median | 95d | 95d | 80 | 75a.b | 0.000 |
| IQR | 90-100 | 90-100 | 52.5-95 | 50-80 | ||
| Physical performance | Median | 100d | 100d | 100d | 50a.b.c | 0.000 |
| IQR | 85-100 | 100-100 | 75-100 | 0-50 | ||
| Discomfort | Median | 90.0c.d | 100.0d | 65.0a | 32.5a.b | 0.000 |
| IQR | 77.5-100 | 100-100 | 48.75-78.75 | 22.5-57.5 | ||
| Emotional performance | Median | 100.0 | 100.0 | 100.0 | 66.6 | 0.057 |
| IQR | 66.6-100 | 100-100 | 88-100 | 33.3-100 | ||
| Mental health | Median | 80 | 88 | 76 | 68 | 0.081 |
| IQR | 60-96 | 80-96 | 73.5-76 | 52-76 | ||
| Vitality | Median | 70d | 78 | 55 | 50a | 0.012 |
| IQR | 55-90 | 60-95 | 47.5–67.5 | 40-55 | ||
| Overall health | Median | 70d | 93d | 55 | 45a.b | 0.000 |
| IQR | 50-90 | 85-100 | 39.5–62.5 | 40-50 | ||
| Social functioning | Median | 100.0d | 100.0 | 75.0d | 62.5a.c | 0.004 |
| IQR | 75-100 | 100-100 | 68.75-81.25 | 37.5-87.5 |
Conducted with the Kruskal-Wallis test; Mann-Whitney’s U test.
Health-Related Quality of Life Score Distribution in accordance with the presence of joint damage (JADI-A).
| No damage | Partial damage | Severe damage | P-value | ||
|---|---|---|---|---|---|
| Physical function | Median | 90c | 90c | 50a.b | 0.003 |
| IQR | 80-100 | 85-90 | 40-85 | ||
| Physical performance | Median | 100 | 100 | 75 | 0.289 |
| IQR | 75-100 | 0-100 | 12.5-100 | ||
| Discomfort | Median | 90.0 | 78.8 | 53.8 | 0.226 |
| IQR | 60-100 | 57.5-100 | 32.5-95 | ||
| Emotional performance | Median | 100.0 | 100.0 | 100.0 | 0.670 |
| IQR | 66.6-100 | 66.6-100 | 33.3-100 | ||
| Mental health | Median | 76 | 78 | 70 | 0.791 |
| IQR | 56-96 | 68-83 | 59-86 | ||
| Vitality | Median | 60 | 58 | 70 | 0.455 |
| IQR | 50-80 | 40-65 | 52.5-75 | ||
| Overall health | Median | 65 | 58 | 50 | 0.195 |
| IQR | 45-90 | 40-80 | 35-67.5 | ||
| Social functioning | Median | 75.0 | 81.3 | 87.5 | 0.807 |
| IQR | 62.5-100 | 75-100 | 50-100 |
Conducted with the Kruskal-Wallis test; Mann Whitney’s U test.
Health-Related Quality of Life Score Distribution in accordance with the presence of extraarticular damage.
| No damage | Partial damage | Severe damage | P-value | ||
|---|---|---|---|---|---|
| Physical function | Median | 90c | 50c | 45a,b | 0024 |
| IQR | 80-100 | 50-85 | 45-75 | ||
| Physical performance | Median | 100 | 75 | 50 | 0,104 |
| IQR | 75-100 | 50-100 | 25-75 | ||
| Discomfort | Median | 90,0 | 62,5 | 75,0 | 0,514 |
| IQR | 57,5-100 | 45-90 | 32,5–77,5 | ||
| Emotional performance | Median | 100,0 | 100,0 | 66,0 | 0,084 |
| IQR | 66,6-100 | 33,3-100 | 33,3–66,6 | ||
| Mental health | Median | 76 | 72 | 64 | 0,283 |
| IQR | 60-92 | 58-76 | 60-68 | ||
| Vitality | Median | 60 | 65 | 55 | 0,852 |
| IQR | 50-80 | 55-75 | 50-70 | ||
| Overall health | Median | 60 | 60 | 55 | 0,397 |
| IQR | 45-90 | 45-70 | 45-65 | ||
| Social functioning | Median | 87,5 | 87,5 | 62,5 | 0,202 |
| IQR | 62,5-100 | 37,5-87,5 | 62-75 |
Conducted with the Kruskal-Wallis test; Mann Whitney’s U test.
Health-Related Quality of Life Score Distribution in accordance with the level of functional capacity (HAQ).
| No disability | Mild | Moderate | Severe | P-value | ||
|---|---|---|---|---|---|---|
| Physical function | Median | 95b.c.d | 88a.c.d | 50a.b | 25a.b | 0.000 |
| IQR | 90-100 | 80-95 | 45-80 | 5-45 | ||
| Physical performance | Median | 100c.d | 100c.d | 50a.b | 13a.b | 0.000 |
| IQR | 90-100 | 62.5-100 | 0-75 | 0-25 | ||
| Discomfort | Median | 100.0b.c.a | 62.5a.c.d | 51.3a.b | 32.5b.d | 0.000 |
| IQR | 85-100 | 51.25-90 | 22.5–67.5 | 32.5-32.5 | ||
| Emotional performance | Median | 100.0 | 100.0 | 83.3 | 66.7 | 0.326 |
| IQR | 90-100 | 49.95-100 | 33.3-100 | 33.3-100 | ||
| Mental health | Median | 80c | 72 | 68a | 78 | 0.042 |
| IQR | 64-100 | 60-84 | 48-72 | 68-88 | ||
| Vitality | Median | 70b.c | 60a | 50a | 63 | 0.005 |
| IQR | 60-95 | 37.5–67.5 | 40-55 | 55-70 | ||
| Overall health | Median | 80b.c | 58a.c | 45a.b | 40 | 0.000 |
| IQR | 56-95 | 42.5-70 | 30-54 | 25-55 | ||
| Social functioning | Median | 100.0d | 75.0 | 68.8 | 43.8a | 0.002 |
| IQR | 75-100 | 62.5-100 | 50-87.5 | 25-62.5 |
Conducted with the Kruskal-Wallis test; Mann-Whitney’s U test.
A multivariate analysis was conducted using logistical regression models. Low scores in the physical parameters of the quality of life assessment (SF-36) were associated with the presence of a major functional disability (OR = 7.05, 95% CI, 1.46–34.03). In contrast, a history of exposure to non-biological DMARDs in pediatric patients (OR = 0.11, 95% CI, 0.01–0.98) was associated to better scores in the physical parameters of quality of life assessments. There was no statistical association between quality of life physical parameters and: JIA subtype, ANA positivity, RF seropositivity, presence of the HLA B27 antigen, or with the exposure to glucocorticoids and biological DMARDs. In the assessment of mental health parameters in the quality of life questionnaire (SF-36), female patients (OR = 8.33, 95% CI, 1.45–47.76) were associated with lower scores. No association was established with other variables analyzed.
DiscussionThere was a prevalence of females in this study, with the exception of the ERA subtype where there was a higher prevalence of males. These findings are consistent with the findings of other authors, and although the gender distribution is similar for the systemic JIA subtype, we also found a higher proportion of females.10,11 Oliveira et al. published a cohort with 426 adult patients, in which 68% of the patients were females, and in the cohort by Tollisen et al., 74% out of 176 adults were women.12,13 With regards to the age of onset of the JIA, the average observed was 9 years, and in approximately one half of the patients the onset of the disease was during the second decade of life. A statistically significant association was observed between the RF positive polyarticular JIA and a disease onset after 10 years old. Patients with persistent oligoarticular JIA had an onset of the disease before 5 years old, and for ERA after 10 years old. These results are consistent with the literature, with age differences according to the subtype of the disease.1–3,10
The most frequently found subtype of JIA in the population studied was ERA (33%), followed in frequency by RF negative polyarticular JIA, oligoarticular JIA, systemic JIA, RF positive polyarticular JIA, undifferentiated arthritis and psoriatic arthritis. When comparing the proportion of patients based on subtype, these results vary with regards to what is reported in the literature, where there is a predominance of patients with the oligoarticular subtype (30–60%), followed by RF negative polyarticular JIA (10–25%), systemic onset arthritis (5–15%), ERA (5–10%), RF positive polyarticular JIA (3–7%), psoriatic arthritis (3–10%) and undifferentiated arthritis (10–20%).1,2,10 A large ethnic variation has been established in the distribution of JIA subtypes. Among Caucasians, there is a prevalence of the oligoarticular and psoriatic subtypes, while in patients with Asian and Hispanic origin, there is a high frequency reported of the ERA subtype, polyarticular JIA and systemic. Black and North American indigenous peoples develop the seropositive JIA subtype more frequently.1,10,11,14 However, the size of the sample in this study does not necessarily reflect the real distribution of the disease in Colombian patients and the results are not comparable with population studies.
In terms of the educational achievement of patients, this factor was not influenced by the severity of the disease or by the presence of functional disability. 91% of the population had a university degree or a technical or technological specialization; only 9% had high school education, and there were no patients with lower academic levels. These findings are consistent with the reports from Oliveira et al., who found that the level of education was not affected by the subtype of JIA, but if differs with this study in which the authors observed that severe disability did have an impact on the educational level.12
The studies that assess the labor impact of the disease have reported variable results. In a literature review conducted by Jetha, they found that the employment rate reported in the various studies varied between 18 and 71%, and that young adults with JIA have less chance of finding a job, as compared against healthy adults. However, this association has not been statistically significant in all the trials.15 This study found that 91% of the patients were actively working or studying, and only 5.8% were unemployed. Although there was no control group available to compare against, this percentage was lower than the unemployment rate reported by DANE (National Administrative Department of Statistics) in October 2018 in 13 cities and metropolitan areas of Colombia.16 Some differences were found with studies by other authors such as Oen, who reported a retrospective cohort with 392 patients with JIA, of which 55% were employed, 23% were students, 8% were housewives, and 9% were unemployed, and this unemployment rate was higher than in the healthy population.17 Tollisen et al. reported that although the academic achievements were similar to the controls, the difference was evidenced in terms of vocational achievements, since adults with JIA have a lower frequency of being in a full-time job, as compared to the control population. Moreover, receiving a life subsidy, having a low academic level and the lack of a full-time job, were associated with a lower score in the physical parameters of the HRQL scale (P < .001). 13
The prevalence of adults with active disease ranges between 40 and 60%.3,6,12 Selvaag et al. reported that 41% of the patients persisted with active disease, 7.4% achieved pharmacological clinical remission, and 59% achieved non-pharmacological remission. The JADASc assessment showed that 13% presented a mild activity of the diseae, 18% moderate and 28% severe. Patients with RF positive polyarticular JIA had a severe activity, with a statistically significant difference (P < .01) when compared against patients with systemic and persistent oligoarticular JIA, who presented lower levels of JADASc.18 Our study found that 33% of the patients persisted with active disease. According to the subtypes, 42% were ERA, 21% were RF polyarticular JIA, 17% RF negative polyarticular JIA, 8% oligoarticular JIA and 4% systemic JIA and psoriatic arthritis. Severe activity was identified in 25% of the patients. Persistently active disease during adulthood was associated with FR positive polyarticular JIA (P = .007), in whom high JADAS c-71 levels were documented; this also indicates a significant association with severe disease (P = .003).
This study found that 26% of the patients had high JADI-A levels, which were statistically significant in patients with the RF negative polyarticular JIA subtype (P = .001) and in patients who were RF positive (P = .055). The small joints were the most affected and although no statistical significance was identified, younger patients and with an earlier onset and longer duration of the disease, were found to present with a more severe joint involvement. Moreover, a late onset of the disease (OR = 0.16, 95% CI, 0.0035–0.80) was associated to a lower risk of presenting articular damage as adults. Similar findings have been reported by other authors.19–25 Articular damage is a frequent finding and in some series it has been more frequently identified in RF positive polyarticular JIA, since RF positivity has been associated with early articular damage and a stronger tendency to disability in the short and long term.26,27
With regards to extraarticular damage, this was found in 14% of the patients presenting with musculoskeletal involvement and ophthalmological sequelae, mostly as a result of uveitis. Adult patients with higher JADI-E scores were associated with an younger age of onset of the disease (P = .028) and a longer disease duration (P = .009). Treatment compliance in pediatric patients (OR = 0–10, 95% CI, 0.012 to 0.83) was associated with less extraarticular damage in adult age. No statistically significant difference was identified between the subtype of JIA and the JADI-E. Oliveira et al. reported low JADI-E scores, and these were associated with a longer duration of the disease (p = 0.001) and to the exposure to glucocorticoids (P = .001).12
In 46.4% of the patients some degree of functional disability was identified, which was moderate to severe in 25%. There was an association between a higher level of functional disability and the RF positive polyarticular JIA subtype (P = .001), the presence of articular damage (OR = 5.75, 95% CI, 1.06–31.12) and being a female (OR = 13.73, 95% CI, 2.35–80.56). Moreover, patients with higher levels of disability had an earlier onset of the disease. However, this finding did not show statistical significance. There was improved functional ability among patients who were compliant with the medical treatment (P = .002) in the pediatric age range. These results are consistent with the reports from other authors.24 Packham and Hall reported severe disability in a larger proportion of patients (42%).28 Tollisen et al. evidenced some degree of physical disability in 47% of the patients (including patients in clinical remission without medication), 3% presented with severe disability after 30 years of follow-up (the same percentage found in our study).13
An RF positive polyarticular JIA subtype and the presence of functional disability (OR = 7.05, 95% CI, 1.46–34.03) were associated with an involvement of the physical parameters in the HRQL assessment. Patients with active disease and severe articular and extraarticular damage, showed a significant association with low scores in the physical and mental health parameters. The presence of severe clinical activity was associated with a compromise in the SF-36 physical assessment. These findings are consistent with the reports from other authors that confirmed the involvement of the HRQL physical component in adulthood.6,27,29,30
Tollisen et al. found that patients with JIA (active and in clinical remission) had lower scores in the SF-36, specifically the parameters that measure the physical component, as compared against the control group (P < 0.001) and with no significant differences in the mental health parameters. In contrast with the scores of the physical parameters in SF-35 with oligoarticular JIA, patients with ERA and psoriatic arthritis had lower scores (P = .001). There were no statistically significant differences in the mental health parameters of the various subtypes. Moreover, high HRQL scores were predictors of physical component involvement in the HRQL assessment (P < 0.001).13 Arkela et al. found no significant compromise in the HRQL assessment in adults with JIA in clinical remission, as compared with the control population.31
This study shows important information about the articular and extraarticular long term results, functional capacity assessment and HRQL in Colombian adult patients with JIA. One of the limitations of the study is the size of the sample, since this is an analysis of a population with a disease that represents 7 different clinical subtypes with variable clinical evolution and variable morbidity; this factor may have an impact on the results obtained. Keeping in mind that when patients reach the adult age they should continue their medical care with an adult rheumatologist, this gave rise to some difficulties to relocate patients. There may be a selection bias and this may represent more severe cases or cases with a longer follow-up, rather than reflecting the true distribution by JIA subtypes.
This is the first study of its kind conducted in Colombia, thus confirming the need to continue educating the medical community about this condition, since most of the complications and sequelae are preventable with early diagnosis, and proper, timely and dynamic treatment to promote an adequate quality of life in the short and long term. Patient and family education is a must for achieving adequate treatment compliance, which is a decisive prognostic factor.
ConclusionsJIA is the most frequent rheumatic disease in pediatric patients, and although clinical remission is usually achieved, a significant proportion of patients remained with the active disease during their adult life. The academic achievements were not compromised in adult patients with JIA; however, there was a low academic level or unemployment in a small percentage of patients with severe articular or extraarticular damage and severe functional disability.
Articular damage may be present in the 7 subtypes of the disease. However, patients with the RF positive polyarticular JIA subtype were severely compromised. The most frequent extraarticular manifestation identified was uveitis, which was associated with significant extraarticular damage. There is a need to emphasize a regular ophthalmological follow-up both in children as in adults, in order to monitor the development of new onset eye involvement and reactivations to avoid short and long term ophthalmological complications that may significantly impact the patient’s quality of life.
It is important to foster pharmacological treatment compliance since it promotes sustained remission, reduces the risk of articular and extraarticular complications, and preserves the functional capacity. The HRQL assessment was mostly affected in patients with the RF positive polyarticular subtype, in patients with active disease and with severe functional disability. The HRQL was mostly compromised in terms of the physical parameters (physical function, physical performance, discomfort, and overall health status) and not in terms of the mental health assessment variables (emotional performance, mental health, vitality and social functioning).
These results confirm the relevance of this trial. Considering that JIA is not a disease restricted to pediatric patients and once they become adults, rheumatologists will have to cope with a disease that has evolved over several years, patients that have been exposed to multiple drug therapies, and a clinical progression with already stablished damage, leading to changes in the therapeutic objectives. The study acquaints both pediatric and adult rheumatologists with the evolution of the disease over time. Currently, the HRQL assessment in clinical practice complements the traditional approach used to monitor patients. Finally, we are currently working on a new classification of the disease in patients with JIA, so that we all speak the same language and hence will be able to improve communications between pediatric and adult rheumatologists.
DisclosuresThe authors declare not having received any institutional financial support to conduct this project.
Please cite this article as: Reina Ávila MF, Malagón C. Calidad de vida relacionada con la salud en pacientes adultos con artritis idiopática juvenil. Rev Colomb Reumatol. 2020;27:26–36.