Kummel's disease is a crush fracture of a vertebral body caused by a minor trauma, with the most accepted etiology being avascular necrosis. It is more frequent in individuals with risk factors such as osteoporosis or prolonged treatment with corticosteroids. Initially, it usually has normal radiological tests and an asymptomatic period, followed by a progressive onset of pain along with probable kyphosis and a sign of void or fluid abscess on radiological tests, which may create nerve/spinal involvement. The case is presented of a 76-year-old man, who was admitted to this center for the differential diagnosis of a single vertebral lesion. After imaging tests and biopsy, the definitive diagnosis of Kummel's disease was reached. The confirmatory diagnosis was reached by vertebral biopsy, but given its invasive nature, imaging techniques can play a significant role. As regards metabolic imaging tests, bone scintigraphy has shown to be one of the most sensitive tools to detect ischemia in earlier stages or to determine if it affects other locations. The whole body scan with diphosphonates shows an increase in activity in relation to bone remodeling activity in this condition. The 3-phase study makes it possible to differentiate whether it is an acute/subacute or chronic process, and can influence the therapeutic decision. Knowledge of this disease is important to make a differential diagnosis with tumour or infectious pathology, with emphasis on performing imaging tests in the event of persistent pain with a normal initial plaque.
La enfermedad de Kummel es una fractura aplastamiento de un cuerpo vertebral precedida por un traumatismo menor, cuya etiología más aceptada es la necrosis avascular. Es más frecuente en individuos con factores de riesgo como osteoporosis o tratamiento prolongado con corticoides. Inicialmente, suele presentar pruebas radiológicas normales y un periodo asintomático, con aparición progresiva del dolor junto a probable cifosis y signo del vacío o absceso líquido en las pruebas radiológicas, pudiendo llegar a crear compromiso nervioso/medular. Presentamos el caso de un varón de 76 años que ingresa en nuestro centro para el diagnóstico diferencial de una lesión única vertebral, tras la realización de las pruebas de imagen y biopsia, se llega al diagnóstico definitivo de enfermedad de Kummel. El diagnóstico de confirmación de esta enfermedad se alcanza mediante la biopsia vertebral, pero dada su naturaleza invasiva, las técnicas de imagen toman un papel relevante. En relación a las pruebas de imagen metabólicas, la gammagrafía ósea ha demostrado ser una de las herramientas más sensibles para detectar isquemia en fases más tempranas o para conocer si afecta a otras localizaciones. El rastreo corporal de cuerpo completo con difosfonatos muestra un aumento de actividad en relación a la actividad ósea remodelativa en este cuadro. El estudio de 3 fases permite diferenciar si se trata de un proceso agudo/subagudo o crónico, influyendo en la decisión terapéutica. Es importante el conocimiento de esta enfermedad para realizar diagnóstico diferencial con patología tumoral o infecciosa e insistir en la realización de pruebas de imagen ante la persistencia del dolor con una placa inicial normal.
Kummel’s disease is an uncommon condition, more frequent in middle-aged and older people and in men, consisting in a crush fracture of a vertebral body which progresses to kyphosis after a minor trauma. Its pathophysiology seems to be the development of avascular necrosis at that level1; it usually occurs in the last thoracic and first lumbar vertebrae, and often includes a single vertebra2; it is more common in people with risk factors such as osteoporosis or prolonged use of corticosteroids.3
Patients with this entity often have a torpid history of pain that does not go away with the usual medication; to reach its diagnosis, neoplasm and infection have normally had to be ruled out previously by means of diagnostic imaging tests and even with a biopsy.
Knowledge of this disease is important, although due to its low frequency it is not usually included in the differential diagnosis of vertebral lesions; in any case, it must be treated effectively with conservative measures before spinal cord involvement occurs and invasive treatment is required.2 A scintigraphic image of vertebral avascular osteonecrosis, which is scarce in the bibliography, is provided (Fig. 1).
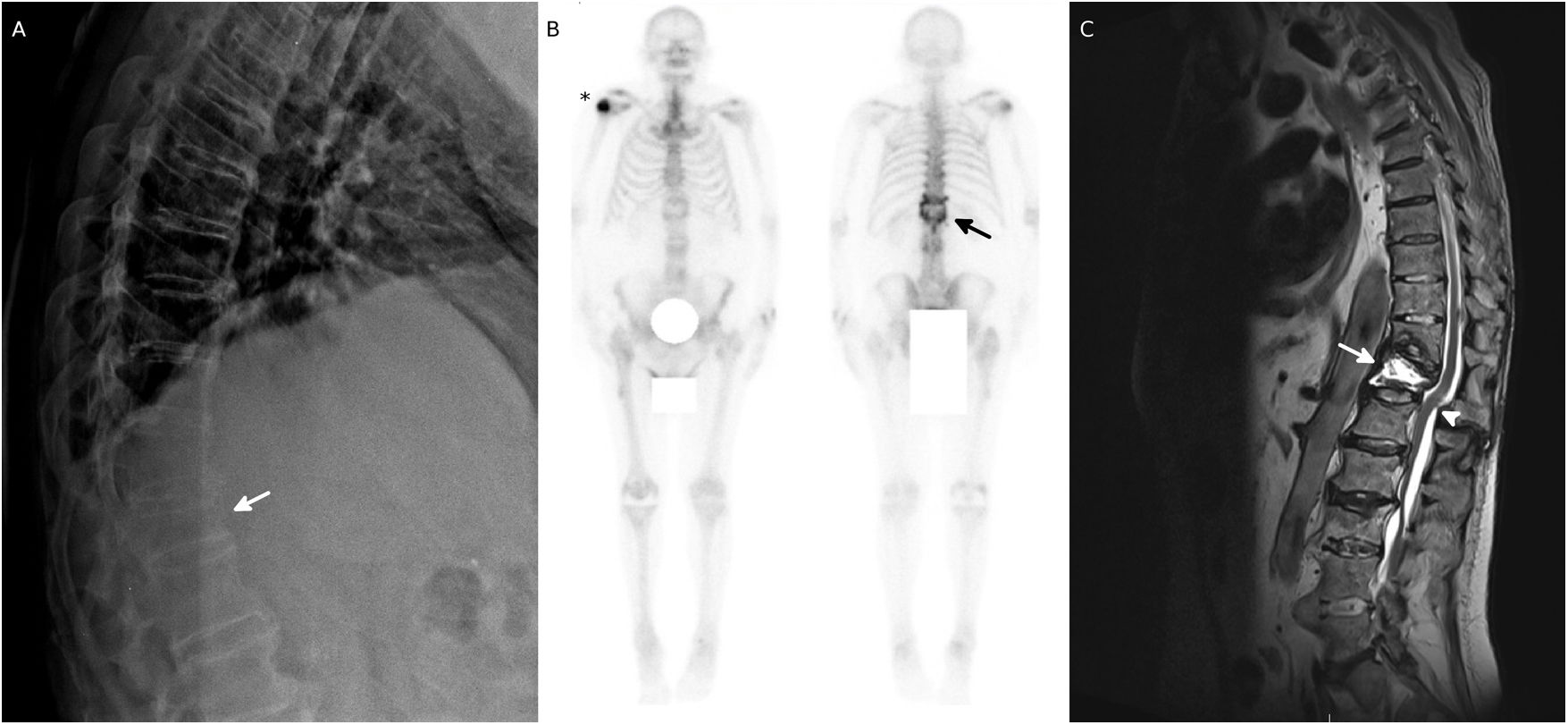
A) Plain radiography with crush-fracture of the vertebral body of T12 (arrow). B) Bone scintigraphy with lesions of high osteoblastic activity in the right humeral tuberosity (asterisk) and thoracolumbar spine (T12-L2 levels). C) MRI of the thoracolumbar spine, in which degenerative spondyloarthritis is observed; spondylodiscitis of T11-T12-L1, with osteolysis of the vertebral body of T12 and intraosseous abscess (arrow); retrolisthesis of T12 and above with deformity of the spinal cord and stenosis of the canal without signs of myelopathy (arrowhead).
Below we present the case of a man with low back pain who came to our center to determine the cause of his illness, due to a poor evolution that increasingly affected his mobility
Presentation of the caseA 76-year-old male patient, with a history of type II diabetes, right total knee prosthesis and femoral intramedullary nail, admitted to our center due to dysphagia, confusion and uncontrolled back pain to be determined, after a trauma that occurred two months earlier, with torpid evolution, which in the plain radiograph showed a crush-fracture of T12.
To assess the osteoblastic activity, a full-body bone scan was performed, in which deposits of high density were observed in the right humeral tuberosity and in the spine (T12, L1, L2) (Fig. 1). The computed tomography revealed partial destruction of the T12 vertebra compatible with spondylodiscitis or tumor lesion and absence of distant neoplastic disease. Subsequently, a MRI showed spondylodiscitis of T11, T12 and L1 and spondylolysis and a fluid abscess in the T12 vertebral body (Fig. 1).
Due to the findings, a biopsy of the T12 vertebral body and T11-T12 disk space was performed, with the absence of malignant neoplastic signs, without the presence of microorganisms and bone fibroregenerative changes related to fracture. Kummel’s disease was concluded as a diagnosis of exclusion and a vertebroplasty was scheduled.
DiscussionKummel's disease is a rare condition that usually occurs in people over 50 years of age, more often in men. It is more common in people with risk factors such as osteoporosis or prolonged use of corticosteroids.3 Its incidence to the present day is unknown. It is a crush-fracture of a vertebral body after a minor trauma, which will develop a progressive kyphosis.1 It usually occurs in the last thoracic and first lumbar vertebrae (T8-L4) (the most frequent area of fractures in the spine); and often includes a single vertebra.2,3
There are several theories about its etiology (pseudoarthrosis, microfractures, fatigue fractures), but the most widespread advocates that the traumatism damages the vascularization of the vertebral body; the anterior third is the most frequently affected, due to the fact that it has a more precarious vascularization, and therefore, avascular necrosis is developed on this area.3,4
It is characteristic that after a trauma there is pain for a short time and the radiograph is normal. Then there is an asymptomatic period (from months to years) until the pain progressively reappears along with the development of kyphosis, and the X-ray shows a crush fracture. If the fracture generates spinal cord-nerve involvement, neurological symptoms can appear.1
The gold standard technique for the diagnosis of avascular osteonecrosis is biopsy, but since it is a very invasive method, we must initially rely on imaging studies and their specific findings.2
A radiological finding specific for osteonecrosis (sensitivity 85%, specificity 99% and positive predictive value 91%),5 although not pathognomonic for Kummel's disease, is the vacuum sign: a horizontal gas line in the vertebral body, in its center or adjacent to the vertebral endplate that can appear in the radiological tests.4 A fluid abscess in the vertebral body visualized on magnetic resonance imaging has also been described as a classic sign of osteonecrosis.2
Some systematic reviews2,6 and few case reports5 that show the usefulness of scintigraphy are found in the bibliography, although the publication of scintigraphic images in this entity is scarce.
Bone scintigraphy usually shows increased tracer uptake in relation to bone remodelling activity; it is one of the most sensitive tools to detect early ischemia, earlier than by the radiological tests. Likewise, it is useful to know if there are other locations. Through the three-phase study, we can differentiate whether it is an acute/subacute process, or rather chronic, which influences the therapeutic decision. A bone uptake of the tracer in all three phases tells us of an acute process, while if we only see activity in the late phase, we should think more of a chronic process; however, the presence of activity indicates that the fracture is not yet consolidated and may respond to treatment. Nevertheless, the presence of an uptake defect in the injured vertebra has been described,5 which could suggest that the study was carried out in a very early stage of necrosis, in which there would not yet be a bone regenerative response, being infrequent the visualization of this acute phase of the necrosis. On the other hand, the SPECT-CT helps to determine anatomically the metabolic changes observed in the scintigraphy.6
In our case, the scintigraphic image was compatible with this pathology and showed a single vertebral lesion, with increased uptake of the tracer at this level; infectious or neoplastic lesions were included in the differential diagnosis and the latter were ruled out by means of biopsy.
Timely diagnosis of this disease is important to apply an adequate treatment, since the delay can lead to spinal deviations, neurological deficits and a subsequent loss of quality of life.2 Factors such as comorbidities, pain or disability must be taken into account for the therapeutic choice, which includes from conservative measures with rest, analgesia or treatment of the osteoporosis in the absence of nervous symptoms and preservation of the posterior wall of the vertebral body, to vertebroplasty, decompression or arthrodesis when the former measures fail, the conditions for these are not met or there is a severe kyphotic deformity.6,7
ConclusionKummel's disease is rare, we must know about it in order to make a differential diagnosis with other pathologies that also cause lesions of the vertebral bodies (neoplasms or infections) and treat it appropriately to avoid the appearance of neurological symptoms. It is important to insist in performing radiographs when there is persistence of pain with an initial normal plain X-ray.
Ethical ConsiderationsPersonal information about the patient is not provided, therefore his anonymity is preserved, and a clinical trial was not conducted with him.
Conflict of interestThe authors declare that they have no conflict of interest.